Barotrauma
| Classification according to ICD-10 | |
|---|---|
| T70.0 | Barotrauma, ear |
| T70.1 | Barotrauma, paranasal sinuses |
| T70.2 | Other and unspecified damage from great heights |
| T70.8 | Other damage from air and water pressure |
| ICD-10 online (WHO version 2019) | |
A barotrauma ('pressure injury ', from the Greek βάρος báros 'heaviness', 'weight', and τραύμα trauma 'wound') is an injury or lesion caused by changes in ambient pressure and its effects on air or gas-filled cavities and their envelopes in living things including humans.
In addition to the extent of the pressure change, the speed of the pressure change is also responsible for the development of a barotrauma. In humans, all air or gas-filled cavities and their envelopes can be affected, regardless of whether the cavities are of natural, artificial or pathological origin. These include lungs , middle ear ( ear drum ), sinuses , caries caves and gas-filled cavities between tight fitting clothes and skin (for example, wetsuit or diving mask ).
Different forms of barotraumas (or barotraumas) are distinguished according to the affected cavities. In a narrower sense, barotrauma is used to denote damage (pressure increase damage) that occurs as a result of exposure to excess pressure . Barotraumas also arise from exposure to negative pressure . Medical significance of the barotrauma with different shapes when diving , flying , Diving and mechanical ventilation . The medical use of positive pressure (as part of hyperbaric oxygen therapy or recompression treatment) and negative pressure can also lead to barotraumas. A common cause of eardrum is the slap .
Cause and pathomechanism
The physical relationship between pressure and volume (volume) of gases or gas mixtures such as air is fundamental for the development of a barotrauma . According to Boyle and Mariotte's law of physics , pressure and volume are inversely proportional to one another when the temperature is constant. This means that with increasing external pressure, the volume of gases or gas mixtures such as air decreases. Conversely, when the external pressure is reduced, the volume increases. The more the pressure changes, the more the volume also changes.
Essentially, this connection also applies to cavities that are filled with gas or gas mixtures. In the case of humans, these would be, for example, the lungs, paranasal sinuses, middle ear and gastrointestinal tract. In addition to the relationship between pressure and volume, the envelope or limitation of the cavities plays an important role here: depending on the nature of the envelope ( muscle rigidity , elasticity , compliance ), a change in pressure (and thus a change in volume) can be tolerated more or less without damage. The time span in which the pressure and thus also the volume change is made is also decisive. In principle, rapid changes in pressure and volume are more damaging than slow changes.
A barotrauma thus always arises when a change in the ambient pressure causes a change in volume of the air or gas-filled cavity, which the cavity itself or its envelope cannot withstand. Depending on the relationship between the pressures and volumes in the cavity and its surroundings, two forms of barotrauma can be distinguished:
- If the ambient pressure is increased by a gas- or air-filled cavity, the result is a volume reduction (shrinkage) of the gas- or air-filled cavity. During this process pressure from the outside and suction from the inside is exerted on the envelope of the cavity. Depending on the surrounding pressure, this form is called overpressure barotrauma .
- If the ambient pressure is lower around a cavity than in itself, this results in an expansion of the cavity. During the process, internal pressure and external suction are exerted on the cavity envelope. Accordingly, this form is known as negative pressure barotrauma .
In humans, it is not possible to differentiate between the two forms with certainty on the basis of symptoms alone; this often requires information about the course and course of the symptoms ( anamnesis ).
Forms of barotrauma
Depending on the air or gas-filled cavity affected, different forms of barotrauma can be distinguished.
Barotrauma of the lungs
The lungs can experience barotrauma associated with diving, flying, mechanical ventilation, hyperbaric oxygen therapy, or bronchoscopy . The barotrauma of the lungs caused by mechanical ventilation is more common than the barotrauma of the lungs that occurs during diving. Barotraumas of the lungs from flies, hyperbaric oxygen therapy, and bronchoscopy are very rare.
Barotrauma of the lungs (diving)
Barotrauma of the lung as part of diving is one of the Auftauchphase ( decompression (English: typical) injury pulmonary barotrauma of ascent ). It can also - but much less often - occur while diving ( compression ). During the ascent, the ambient pressure of the diver is reduced (decreasing water depth ). As a result, the volume of both lungs expands accordingly and the elastic lung boundary or envelope ( pleura ) expands . If there is no exhalation from the lungs with continued pressure reduction in the environment (decreasing water depth ), the air or gas remains in the lungs and expands them further in accordance with the decreasing ambient pressure. If the volume expansion of the lungs exceeds the elastic capacity of the pleura, it is more or less destroyed at its weakest point. To put it simply, a rupture of the lung occurs .
If the pleural injury (lung tear) is small and not in connection with the pleural space ( pleural space ) or the blood vessel system of the lungs, the barotrauma of the lungs can have no consequences. More typical, however, is a connection between the pleural injury and the vascular system of the lungs, particularly pulmonary veins . In the event of a continued pressure reduction (surfacing) and thus expansion of the air in the lungs, this leads to air entering the pulmonary blood vessels. If a pulmonary vein is connected to the lungs via a pleural injury, air (or another gas mixture) enters the heart via the pulmonary vein. From there, the air or gas or gas mixture bubble is pumped through the left main chamber into the arterial blood circulation. Depending on the position of the diver or the size of the air or gas bubble, it is first pumped into the aorta (main artery) and may come to a standstill in arteries with a smaller diameter and partially or completely block them. These can be the arteries of the brain , spinal cord , coronary arteries, or any other arterial blood vessel.
Corresponding to the location of the stagnation or lying staying of the air or gas bubble results in a pathology: the brain is affected, cerebral gas embolism (CAGE; cerebral arterial gaseous embolism ) occurred. The damage corresponds to an embolic stroke . If the spinal cord is affected, a spinal gas embolism (SAGE; spinal arterial gaseous embolism ) has occurred. This damage also corresponds to a stroke of the spinal cord. If the gas bubbles in the coronary arteries come to a standstill and they become blocked, a heart attack occurs due to the gas bubbles.
When the pleural injury creates a connection between the pleural space and the lungs through the barotrauma of the lungs, air or gas enters the pleural space. This eliminates the negative pressure that exists there compared to the contents of the lungs: a pneumothorax is created . In this case, by releasing the relative negative pressure in the pleural space, the lungs are no longer kept stretched and - to simplify - collapse. As a result, the area available for gas exchange is suddenly reduced. As the decompression continues, not only the lungs, but also the “faulty” air in the pleural space increases in volume, the collapsed lung shifts towards the middle layer ( mediastinum ). In the further course, the mediastinum itself is pushed towards the unaffected lungs. This situation is that of a tension pneumothorax .
In contrast to decompression sickness , the risk of developing barotrauma is greatest at low depths (0 to 10 meters water depth). In this depth range, the increase in pressure by approx. 1 bar causes the greatest change in volume (up to 50%). If, especially in this depth range, the patient ascends very quickly without breathing (no “letting out of the expanded air in the lungs”), a barotrauma of the lungs is particularly likely.
| Table 1. Change in volume of the lungs as a function of the water depth and ambient pressure | |||||
|---|---|---|---|---|---|
| Depth (from water surface) | Place (example) | Ambient pressure | Lung volume | Change in lung volume | |
| 0 m | Water surface | 1.0 bar | 6.00 L | ± 0.00% | ± 0.00 L |
| 1 m | Non-swimmer pools | 1.1 bar | 5.45 L. | - 9.09% | - 0.55 L. |
| 2 m | Swimmer pool | 1.2 bar | 5.00 L. | - 16.67% | - 1.00 L |
| 3 m | Under 3 m diving platform | 1.3 bar | 4.62 L. | - 23.08% | - 1.38 L. |
| 4 m | Under 5 m diving platform | 1.4 bar | 4.29 L. | - 28.57% | - 1.71 L |
| 5 m | Under 7 m diving platform | 1.5 bar | 4.00 L | - 33.33% | - 2.00 L |
| 10 m | Rhine at flood in Cologne | 2.0 bar | 3.00 L | - 50.00% | - 3.00 L |
| 20 m | Diving depth without deep intoxication with compressed air | 3.0 bar | 2.00 L. | - 66.67% | - 4.00 L |
| 50 m | 6.0 bar | 1.00 L. | - 83.33% | - 5.00 L | |
| 100 m | Middle depth of the Baltic Sea | 11.0 bar | 0.55 L. | - 90.91% | - 5.45 L. |
| The ambient pressure was calculated using the approximation that 10 mWS corresponds to 1.00 bar. | |||||
Barotrauma of the lungs (ventilation)
Barotrauma of the lungs is lung damage caused by increased intrathoracic pressure (pressure in the chest ) and can occur during mechanical ventilation. Frequent manifestations of barotrauma can be interstitial emphysema or soft tissue emphysema as well as pneumothorax and pneumomediastinum , and more rarely pneumopericardium , pneumoperitoneum and gas embolism .
Barotrauma of the lungs (flies)
Barotrauma of the lungs can also occur while flying a commercial aircraft and the associated lowering of the ambient pressure. It is significantly less common than lung barotraumas that occur in connection with diving or mechanical ventilation. A major reason for this frequency distribution is that the pressure differences when flying due to exposure to negative pressure at altitude are lower than when exposed to positive pressure, for example in water.
| Table 2. Change in volume of the lungs as a function of the height above sea level (atmospheric pressure or ambient pressure) | |||||
|---|---|---|---|---|---|
| Altitude above sea level) | Place (example) | Ambient pressure | Lung volume | Change in lung volume | |
| 0 m | Water surface | 1.013 bar | 6.00 L | ± 0.00% | ± 0.00 L |
| 10 m | Dike crown by the sea | 1.012 bar | 6.01 L. | + 0.12% | + 0.01 L |
| 100 m | Roof of a large skyscraper | 1.001 bar | 6.07 L. | + 1.19% | + 0.07 L |
| 1000 m | 0.899 bar | 6.76 L. | + 12.74% | + 0.76 L | |
| 2000 m | Internal cabin pressure of a commercial aircraft (rule) | 0.795 bar | 7.65 L. | + 27.30% | + 1.65 L |
| 2500 m | Internal cabin pressure of a commercial aircraft (minimal) | 0.747 bar | 8.14 L. | + 35.67% | + 2.14 L |
| 2963 m | Zugspitze (highest mountain in Germany ) | 0.704 bar | 8.63 L. | + 43.84% | + 2.63 L |
| 4792 m | Mont Blanc (highest mountain in the Alps ) | 0.555 bar | 10.95 L | + 82.62% | + 4.96 L |
| 8848 m | Mount Everest (highest mountain on earth ) | 0.315 bar | 19.33 L. | + 222.18% | + 13.33 L |
| 10,000 m | Travel height of aircraft | 0.264 bar | 22.99 L | + 283.19% | + 16.99 L |
| The calculation of the ambient pressure was carried out according to the international altitude formula with 15 ° C as the assumed temperature. Thus, the calculated values are to be understood approximately to clarify the relationship between altitude (ambient pressure) and volume. | |||||
Barotrauma of the lungs (hyperbaric oxygen therapy)
Barotrauma of the lungs can occur when using hyperbaric oxygen therapy (HBO). Similar to diving, barotrauma of the lungs is possible, especially in the decompression phase of the HBO treatment unit (colloquially known as "diving trip"). Barotrauma of the lungs is a rare to very rare, but very serious side effect in the context of hyperbaric oxygen therapy.
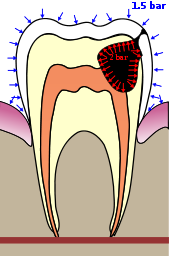
Barotrauma of the teeth
A barotrauma of the teeth or a tooth cannot occur in completely healthy teeth. Barotrauma cannot occur with faultless fillings, bridges and implants, since there is no air or gas-filled cavity with no connection to the environment.
If an air or gas-filled cavity forms in a tooth as a result of caries, for example (see Fig. 1), then if the connection to the oral cavity is missing or blocked, no pressure equalization can take place. With increasing ambient pressure, the result is a reduction in the volume of air or gas in the cavity (for example a caries cavity) in the tooth. Since the tooth, for example in contrast to the lungs, is made of non-elastic material, the pressure in the cavity of the tooth drops and leads to an implosion if the tolerance limits of the tooth substance are exceeded .
At the same time, there is barotrauma of the teeth, which occurs in connection with decompression. In this case, too, with a missing or closed connection, for example a caries cavity to the oral cavity, with falling ambient pressure, the volume in the tooth cavity increases. However, this is limited by the rigidity of the tooth material, so that the pressure in the tooth cavity increases. If the pressure in the tooth cavity exceeds the tolerance point of the tooth substance, it is subsequently broken up. If the ambient pressure is reduced very quickly (and thus the pressure difference increases), the tooth can explode . If the tooth cavity affects a filling or bridge, it can also break.
Teeth barotrauma occurs mainly when diving. Like other forms of barotrauma, it is less common when flying.
Middle ear barotrauma
The most common barotrauma of all is the barotrauma of the middle ear, also called baro-otitis or aero-otitis.
The barotrauma of the middle ear almost always only occurs during an increase in pressure in the environment (descent when diving, landing approach when flying, impact when jumping in the water or water skiing), since the relative overpressure in the middle ear leads to a decrease in pressure in the environment (ascent, starting when flying) Passive opening of the tube leads and thus a pressure equalization is established. In the event of a sudden and strong drop in pressure in the environment ("explosive decompression"), barotrauma of the middle ear including tearing of the eardrum is possible, even if the pressure is reduced. Decompression sickness is to be distinguished from barotrauma caused by pressure reduction , which can also lead to the involvement of the inner ear .
If there is overpressure in the surrounding area, the tube ( Eustachi tube ) must be actively opened by muscles ( Musculus tensor veli palatini , Musculus salpingo-pharyngeus ) either by swallowing or chewing or - if possible - deliberately, which is achieved with a vacuum of 80 up to 90 mm Hg in the middle ear is no longer possible. However, it may still be possible to open the tube with a Valsalva maneuver or forcing in air with a Politzer balloon ( tube burst ). With increasing external pressure or negative pressure in the middle ear, depending on the extent and duration of the pressure difference, the mucous membrane becomes - painful - oedematous and blood- fibrinous exudate gradually emerges from the mucous membrane, which also leads to a hearing impairment. The accumulation of fluid eventually leads to a bulging of the eardrum, which appears bright red and shows bleeding. A tympanic membrane rupture is possible with a rapid and strong increase in pressure. Baro-otitis and a tear in the eardrum usually heal without any consequences. Pain reliever medication is recommended. In the case of baro-otitis, antibiotic treatment is pointless and should therefore be avoided. However, if the eardrum is perforated, water penetration can lead to bacterial otitis media , which must be treated with antibiotics.
In individual cases, barotraumas of the middle ear in connection with nitrous oxide anesthesia (laughing gas) have also been observed.
Barotrauma of the middle ear from diving
If the ambient pressure is increased in the course of diving (compression), the volume of the air (or gas or gas mixture) contained in the middle ear behind the eardrum decreases. As a result of these conditions the eardrum is pressed by the water towards the middle ear. If the pressure in the middle ear cannot be increased by supplying air or gas through the Eustachian tube , the changes in the middle ear described above will result with increasing pain. If the elasticity of the eardrum is exceeded, the eardrum tears ( torn eardrum ). When diving, water then gets into the middle ear, which, because the water temperature is usually lower than that of the body, leads to caloric nystagmus with dizziness due to irritation of the equilibrium organ in the affected ear.
Any blockage of the Eustachian tube such as by colds , ear infections , Tubenkatarrh difficult or congenital or acquired narrowing or prevent especially the inflow of air or gas in the middle ear (tubal ventilation disorder). A pressure difference or a change in volume cannot then be compensated for by supplying air, which can lead to a tear in the eardrum.
A tear in the eardrum is associated with temporary hearing loss. Repeated tears of the eardrum can lead to permanent hearing loss due to the resulting scarring when healing. Injuries to the eardrum such as reddening and bleeding usually heal without any consequences.
Barotrauma of the middle ear due to hyperbaric oxygen therapy
In the context of hyperbaric oxygen therapy, barotraumas of the middle ear (eardrums) occur mainly during the compression phase ("diving down") in analogy to diving. The barotrauma of the middle ear is the most common side effect of hyperbaric oxygen therapy, although rarely severe in the sense of a torn eardrum. Even patients who are not able to adjust the pressure in the middle ear to the ambient pressure (for example ventilated patients) often suffer from barotraumas of the middle ear or eardrum.
Barotrauma of the middle ear from flying
During a flight with an airliner there are two “opportunities” to suffer from a barotrauma of the middle ear (eardrum). Compared to the barotrauma during diving, the barotrauma is due to decompression at the beginning of a flight, the barotrauma due to compression at the end of a flight.
After take-off, the pressure inside the cabin is reduced to approx. 0.75-0.85 bar with increasing flight altitude, which corresponds to an altitude of 1500 to 2500 m . Barotrauma of the middle ear (eardrum) can occur - albeit extremely rarely - when the eustachian tube is blocked, especially if the internal cabin pressure is reduced very quickly . Blockages of the Eustachian tube are particularly common in children compared to adults. The second "opportunity to acquire" middle ear (eardrum) rotrauma is during landing. Here the internal cabin pressure is brought back to the level of the ambient pressure; If the ambient pressure corresponds to the atmospheric pressure at sea level, the result is pressure increases of 0.15 to 0.25 bar. Again, people are particularly affected who cannot achieve proper ventilation of the middle ear due to blockages in the Eustachian tube. To prevent barotrauma when traveling by air, the use of a decongestant nasal spray can be helpful.
Barotrauma of the digestive tract
Barotrauma of the digestive tract (stomach, intestines) is extremely rare.
Barotrauma of the skin
Barotrauma of the skin, which can occur when diving with a dry suit, is less common . This barotrauma is also called suit squeeze and occurs when the negative pressure created in the suit is not compensated in time by letting in air when diving. Wrinkles in the suit then lead to skin bruises.
Barotrauma of the eye
Another, albeit lighter, form can occur both in recreational diving with a device and in apnea diving , the barotrauma of the eye. When diving down, a negative pressure is created in the cavity between the eye and the diving mask , which affects the eyes. The diver feels a pain in the eyes. He can remedy this by wearing a suitable diving mask and regularly exhaling gently through his nose, thus compensating for the negative pressure.
Web links
swell
Textbooks
- C. Edmonds, C. Lowry, J. Pennefather, R. Walker: Diving and subaquatic medicine. 4th edition. Hodder Arnold Publishing, London 2002, ISBN 0-340-80629-X .
Original and review articles
- ^ H. Schubothe: Changes in atmospheric pressure and damage and illnesses caused by a lack of oxygen. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 1184-1191, here: pp. 1184 f. ( Pressure rise damage ).
- ↑ Das Ohr IV - Barotrauma , www.barotrauma.de
- ↑ CG Wherrett, RJ Mehran, MA Beaulieu: Cerebral arterial gas embolism following diagnostic bronchoscopy: delayed treatment with hyperbaric oxygen. In: Can J Anaesth. 49 (1), 2002, pp. 96-99.
- ↑ RW Smerz: Concomitant cerebral and coronary arterial gas emboli in a sport diver: a case report. In: Hawaii Med J. 64 (1), 2005, pp. 12-13. PMID 15751753 .
- ↑ GD Becker, GJ Parell: barotrauma of the ears and sinuses after scuba diving. In: Eur Arch Otorhinolaryngol. 258 (4), 2001, pp. 159-163.
- ^ HB Newton: Neurologic complications of scuba diving. In: Am Fam Physician. 63 (11), 2001, pp. 2211-2218.
- ^ CR Carpenter: Recurrent pulmonary barotrauma in scuba diving and the risks of future hyperbaric exposures: a case report. In: Undersea Hyperb Med. 24 (3), 1997, pp. 209-213.
- ^ WP Butler: Cases from the Aerospace Medicine Resident's Teaching File: unsuspected pulmonary barotrauma. In: Aviat Space Environ Med. 71 (11 Pt 1), 2000, pp. 1153-1156.
- ↑ Hilmar Burchardi: Etiology and pathophysiology of acute respiratory failure (ARI). In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid. 1994, ISBN 3-540-57904-4 , pp. 47-91; here: p. 89 f.
- ↑ GC Briassoulis, ST Venkataraman, AG Vasilopoulos, LC Sianidou, JH Papadatos: Air leaks from the respiratory tract in mechanically ventilated children with severe respiratory disease. In: Pediatr Pulmonol . 29 (2), 2000, pp. 127-134.
- ^ RM Cooper, S. Grgas: Fatal barotrauma resulting from misuse of a resuscitation bag. In: Anesthesiology. 93 (3), 2000, pp. 892-893.
- ↑ H. Jantsch, G. Lechner: Radiological monitoring of the ventilated patient. In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unaltered edition, ibid 1994, ISBN 3-540-57904-4 , pp. 134-168; here: pp. 149–158.
- ^ GG Cable, T. Keeble, G. Wilson: Pulmonary cyst and cerebral arterial gas embolism in a hypobaric chamber: a case report. In: Aviat Space Environ Med. 71 (2), 2000, pp. 172-176.
- ↑ MJ Hickey, CL Zanetti: Delayed-onset cerebral arterial gas embolism in a commercial airlinemechanic. In: Aviat Space Environ Med. 74 (9), 2003, pp. 977-980.
- ↑ CT Lee: Cerebral arterial gas embolism in air force ground maintenance crew - a report of two cases. In: Aviat Space Environ Med. 70 (7), 1999, pp. 698-700.
- ↑ K. Tetzlaff, M. Reuter, J. Kampen, C. Lott: Hyperbaric chamber-related decompression illness in a patient with asymptomatic pulmonary. sarcoidosis. In: Aviat Space Environ Med. 70 (6), 1999, pp. 594-597.
- ↑ J. Capeder, A. Frutiger, J. Gartmann, U. Wulser: Traumatic pulmonary pseudocysts. In: Dtsch Med Wochenschr. 109 (28-29), 1984, pp. 1116-1121.
- ^ IM Calder, JD Ramsey: Ondontecrexis - the effects of rapid decompression on restored teeth. In: J Dent . 11 (4), 1983, pp. 318-323.
- ↑ G. Magnano, GE Solimei, L. Cingano, A. Benedicenti: The maxillo-dental apparatus in hyperbaric conditions (II - toothache). In: Parodontol Stomatol (Nuova). 23 (1), 1984, pp. 175-178.
- ^ MA Delbeke, R. van Peteghem: [Dental injuries in diving]. In: Rev Belge Med Dent. 38 (1), 1983, pp. 21-22.
- ^ JG Grenier: Diving as related to dentistry. In: Can Forces Dent Serv Bull. 1982; (2), pp. 6-7.
- ↑ RE Holowatyj: Barodontalgia among flyers: a review of seven cases. In: J Can Dent Assoc. 62 (7), 1996, pp. 578-584.
- ↑ J. Jensen: Barodontalgia among Danish fighter pilots. In: Tandlaegebladet. 88 (20), 1984, pp. 726-729.
- ↑ E. Lehnhardt: The occupational damage of the ear. In: Arch ear, nose and larynx healing. 185, 1965, pp. 11-242.
- ↑ JA Carter, FM Nofal: Tympanic membrane rupture during nitrous oxide anaesthesia. In: Br J Anaesth. 53 (2), 1981, p. 194.
- ^ M. Boni: Middle and inner ear barotrauma caused by scubadiving (author's transl). In: ENT. 27 (11), 1979, pp. 373-374.
- ↑ GJ Bayliss: Aural barotrauma in naval divers. In: Arch Otolaryngol. 88 (2), 1968, pp. 141-147.
- ↑ SM Green, SG Rothrock, EA Green: Tympanometric evaluation of middle ear barotrauma during recreational scuba diving. In: Int J Sports Med. 14 (7), 1993, pp. 411-415.
- Jump up ↑ J. Blanshard, A. Toma, P. Bryson, P. Williamson: Middle ear barotrauma in patients undergoing hyperbaric oxygen therapy. In: Clin Otolaryngol Allied Sci. 21 (5), 1996, pp. 400-403.
- ↑ M. Beuerlein, RN Nelson, DB Welling: Inner and middle ear hyperbaric oxygen-induced barotrauma. In: Laryngoscope. 107 (10), 1997, pp. 1350-1356.
- ↑ C. Plafki, P. Peters, M. Almeling, W. Welslau, R. Busch: Complications and side effects of hyperbaric oxygen therapy. In: Aviat Space Environ Med. 71 (2), 2000, pp. 119-124.
- ↑ G. Presswood, WA Zamboni, LL Stephenson, PM Santos: Effect of artificial airway on ear complications from hyperbaric oxygen. In: Laryngoscope. 104 (11 Pt 1), 1994, pp. 1383-1384.
- ↑ HW Kortschot, WJ Oosterveld: Barotrauma in Boeing 737 cabin crew. In: ORL J Otorhinolaryngol Relat Spec. 55 (2), 1993, pp. 114-116.
- ^ Eustachian tubes and airplanes. In: Pediatr Infect Dis J 9 (4), 1990, p. 304.
- ^ Hazards of air travel for a child with otitis. In: Pediatr Infect Dis J. 8 (8), 1989, pp. 542-543.
- ^ PF King: The Eustachian tube and its significance in flight. In: J Laryngol Otol. 93 (7), 1979, pp. 659-678.
- ↑ H. Vuilleumier, D. Vouillamoz, JF Cuttat: Gastric rupture secondary to barotrauma in the framework of a diving accident. Speaking of a case report and literature review. In: Swiss Surg. 1995; (5), pp. 226-229.