Glomerulonephritis
| Classification according to ICD-10 | |
|---|---|
| N00.- | Acute Nephritic Syndrome |
| N01.- | Rapid progressive nephritic syndrome |
| N03.- | Chronic nephritic syndrome |
| N05.- | Unspecified nephritic syndrome |
| N08 .- * | Glomerular Diseases in Diseases Classified Elsewhere |
| ICD-10 online (WHO version 2019) | |
As glomerulonephritis (from " Nephritis ", Greek and Latin for nephritis; plurality: glomerulonephritis ; abbreviation: GN) bilateral inflammation of the kidney is known, in which the glomeruli ( glomeruli ) are affected first. A distinction is made between various forms which, taken together, are among the most common causes of chronic kidney failure . The glomerulonephritis are a subgroup of the glomerular diseases ( glomerulopathies ).
to form
The classification of glomerulonephritis is not uniform, as they can be classified based on their origin, histological appearance and clinical form and can therefore be classified from different angles. Based on the pathogenesis, one can differentiate between primary and secondary glomerulonephritis.
Primary forms
This is understood to mean different forms of autoimmune- induced glomerulonephritis that are not preceded by any other disease or have not yet been identified. Most forms of glomerulonephritis exist in primary and secondary forms. For example, IgA glomerulonephritis can also be seen as secondary to liver cirrhosis. Primary membranous glomerulonephritis is attributed to autoantibodies (mostly of the IgG4 isotype) against PLA2R. Other primary glomerulonephritis are anti- basement membrane antibody glomerulopephritis, membranoproliferative GN and C3 glomerulonephritis. The focal segmental glomerulosclerosis referred initially only a glomerular scarring, less concerned than half of the glomeruli in less than half of each glomerulus. It can also occur as a primary or secondary form. Secondly, it is possible in any glomerulonephritis. Focal and segmental glomerulosclerosis, like minimal glomerular lesions, are not counted among the glomerulonephritis.
Secondary forms
The secondary glomerulonephritis can be traced back to a disease outside the kidneys or generalized diseases, such as infection in the endocapillary proliferative GN (= post-infectious GN or post-streptococcal GN), autoimmune diseases such as Goodpasture's syndrome , granulomatosis with polyangiitis , the Disseminated lupus erythematosus , drugs such as gold or penicillamine . Alport's syndrome , which can be traced back to a genetic defect in type IV collagen , only leads to degenerative changes in the glomeruli with glomerulonephritis-like symptoms and findings, but glomerulonephritis is not present.
Other classifications
The necrotizing intra- / extracapillary proliferative GN with diffuse crescent formation (= rapid-progressive GN, RPGN) has a special role, since it can occur in different forms of GN and describes the clinical course.
Kidney diseases that do not belong to the glomerulonephritis as well as degenerative changes in the glomerula in systemic diseases such as diabetes mellitus , lupus erythematosus or amyloidosis , like glomerulonephritis, can ultimately lead to sclerosis of the kidney corpuscles ( glomerulosclerosis ).
Glomerular minimal lesions ( minimal change glomerulopathy ) and primary forms of focal segmental glomerulosclerosis cannot formally be regarded as glomerulonephritis because they lack characteristic features of inflammation (-itis). Nonetheless, minimal change glomerulopathy is erroneously referred to as minimal change glomerulonephritis (MCGN) by nephrological laypeople.
List of glomerulonephritis
- fibrillar glomerulonephritis and immunotactoid glomerulonephritis, with congo-red negative extracellular microtubular and fibrillary deposits, respectively
- membranoproliferative glomerulonephritis type I , type II and type III
- membranous (epimembranous) glomerulonephritis
- mesangioproliferative glomerulonephritis, with the most common special form IgA nephritis
- clinically necrotizing glomerulonephritis as rapidly progressive glomerulonephritis referred
- post- infectious or, better, infection-associated glomerulonephritis, usually as post-streptococcal glomerulonephritis
- Alport syndrome is a synonym for hereditary glomerulonephritis , mostly X-linked dominant, rarely autosomal recessive inherited defect of type IV collagen , which occurs in the kidneys, inner ear and eye.
- (Löhleinsche) Herd-shaped glomerulonephritis, which mainly affects the glomeruli, also known as glomerulitis
Symptoms
Glomerulonephritis express themselves mostly as nephritic syndrome (hematuria, proteinuria less than 3 g / day, salt and water retention, arterial hypertension) or nephrotic syndrome (urinary protein excretion> 3.0 to 3.5 g / day in adults, hypoalbuminemia , Hyperlidpidämie , Tendency to thrombosis , edema ). It is by no means correct that chronic glomerulonephritis always expresses itself with a nephrotic syndrome and acute always with a nephritic syndrome. The nephrotic syndrome usually occurs in membranous glomerulonephritis and membranoproliferative glomerulonephritis (the latter often with hematuria). Mesangioproliferative glomerulonephritis usually expresses itself as nephritic syndrome, extracapillary proliferative glomerulonephritis usually as rapidly progressive glomerulonephritis with hematuria, proteinuria and rapidly deteriorating kidney function.
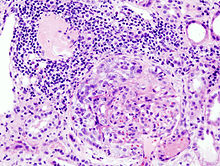
The exact diagnosis can be narrowed down through serum examinations; the definitive diagnosis can only be made through a kidney biopsy .
diagnosis
The suspicion of glomerulonephritis is based on laboratory diagnostics of blood and urine . In most cases, a kidney biopsy should be aimed for as a definitive diagnosis. Exceptions are self-limiting forms such as post-streptococcal glomerulonephritis . Conclusions for therapy and prognosis can be drawn from the tissue examination in conjunction with an electron microscopic examination and immunohistochemical staining of the biopsy .
therapy
Treatment methods also vary depending on the form of the disease. Immunosuppressive therapies are usually used. However, the type of disease should be known for treatment.
Individual evidence
- ^ Claus-Peter Adler, Ursus-Nikolaus Riede: General and special pathology . Thieme, Stuttgart et al. 1993, ISBN 3-13-778701-7 .
- ^ Herbert Renz-Polster, Steffen Krautzig, Jörg Braun: Basic textbook internal medicine . 4th edition. Urban & Fischer-Verlag / Elsevier, 2008, ISBN 3-437-41053-9 .
- ^ Noel Weidner, Richard J. Cote, Saul Suster: Modern Surgical Pathology . Elsevier Health Sciences, July 8, 2009, ISBN 1-4377-1958-9 , p. 1006.
- ↑ Gerd Herold et al. : Internal medicine. A lecture-oriented presentation . Self-published, 2016, ISBN 978-3-9814660-5-8 , p. 610-621 .
- ↑ Joachim Frey : Haemorrhagic nephritis. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 926-951, here: pp. 938-940 ( Herdnephritis ).
Web links
- University of Greifswald: New therapy for severe kidney disease (RPGN) discovered (press release at idw)