GIS in healthcare
Geographic Information Systems (GISs) and Geographical Information Science (GIScience) combine computer cartography with additional database management and data analysis tools . Commercial GIS have already gained a foothold in many application areas and industries, such as the environmental sciences , urban planning , agriculture, and others.
The health care is another subject which increasingly takes advantage of GIS. A strict definition of health care is difficult to establish because it is used in different ways by different groups. Basically, health care differs from private health in that its focus is on the health of populations rather than that of individuals, prevention is more important than treatment itself, and it operates in a much more nationalized context than private health does . Therefore, GIS and other spatial analysis tools have been identified as potential implementation options for healthcare goals.
history
Healthcare efforts have been supported by the analysis and application of spatial data for many years. Often seen as the father of epidemiology , the British doctor John Snow is a famous example of such an endeavor. Snow used a hand-drawn map to analyze the geographic locations of deaths during the great cholera epidemic in London in 1854. With this map, he was able to show that the number of cholera deaths was concentrated near wells and that the then large Broadwick water pump was the largest source of the cholera outbreak. The removal of this pump resulted in a rapid decline in new cholera infections, proving his theory and convincing the medical community.
Snow's work serves as a guide to how research and other health science research can benefit from GIS applications. He continued analyzing his data to find out whether the frequency of cholera incidents was also directly related to local elevation, soil conditions and alkalinity. Low-lying areas, especially those with poorly water-absorbing soil, were found to have a higher frequency of cholera incidents. Snow was able to confirm his hypothesis and found that it was caused by large accumulations of water, which in turn proves that cholera is a disease that originates in the groundwater (contrary to the original, widespread assumption that the odor is the cause).
This is a very early example of what is now known as disease diffusion mapping. The basic idea is that a disease always starts from a source or a central point and then spreads through the surrounding environment, depending on certain characteristics and patterns. Desease Diffusion Mapping is therefore another example of research that makes use of the possibilities of GIS.
GIS in healthcare
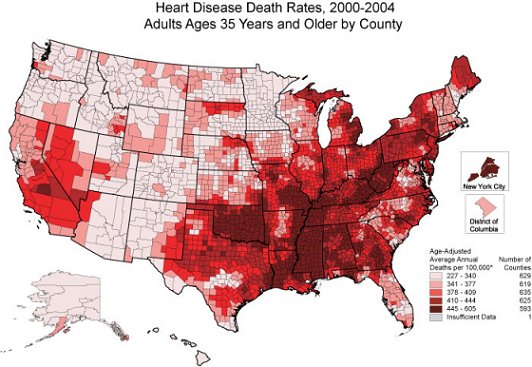
Health problems today are far larger than those that Snow addressed then. Scientists are now dependent on modern GIS and other computer mapping applications to support their analyzes. Take the graph on the right as an example, which shows the death rate from heart disease in white men over 35 in the United States between 2000 and 2004.
Public health informatics (PHI) is a young but rapidly growing field that focuses on providing information science and technologies for applications and research in health care. As part of this, there is the GIS, or more generally, Decision Support System (SDSS), which offers improved geographic visualization technologies and is designed to lead to faster, better, more robust understanding and higher quality decision-making in healthcare.
One example of this is GIS displays, which have been used to show a clear link between accumulations of hepatitis C cases and intravenous drug users in Connecticut. The cause is difficult to show clearly because collocation alone does not establish a cause. Evidence of previous causal relationships (such as the intravenous use of drugs and hepatitis C) can, however, strengthen the acceptance of such relationships and can help to demonstrate the usability and reliability of GIS-based solutions. Conversely, the random, apparent causal dependence of two parameters can help stimulate further investigations in this direction.
Alternatively, GIS techniques were used to show that there was no correlation between different causes and effects. For example, the distributions of birth defects and child mortality rates in Iowa have been studied and no association between these parameters has been discovered by researchers. This in turn led to the conclusion that birth defects and child mortality rates are very likely to be unrelated and that each has different causes and risk factors.
GIS can therefore support healthcare in very different ways. Primarily, GIS displays therefore support the understanding of facts and provide a better basis for decision-making. For example, eliminating the huge health disparities is one of the top two goals of Healthy People 2010, one of the largest health care programs in the United States. GIS can play an essential role in this program by helping people practicing in that field to identify areas of health injustice and, ideally, helping people in these spaces find solutions and address these inadequacies. GIS can also help scientists integrate disparate data from a wide variety of sources and can even be used to enforce measures of quality control of such data. Much data in healthcare is still generated manually and is therefore subject to human error. For example, North Carolina geographic analysis of health care data showed that over 40% of the files contained errors. On the one hand, incorrect geographical information (city, district, zip code) was found and, on the other hand, there were errors that would never have been discovered if the visual GIS displays had not existed. Correcting this erroneous or non-existent data not only resulted in more accurate and correct GIS displays, but also helped to improve all analyzes that were based on this data.
Problems of GIS in Healthcare
There are also concerns or issues about the use of GIS in healthcare. One of the biggest concerns is privacy and the confidentiality of personal information. Healthcare is concerned about the health of the population as a whole, but needs to use data from individuals to make the necessary assessments, and the protection of the privacy and personal information of these individuals is of paramount importance. The use of GIS displays and associated databases requires dealing with the problems just mentioned, so some precautions are necessary to prevent individuals from being recognized based on spatial data. For example, data could be merged and no longer assigned to individual people, but now to larger areas, such as the postcode or a district. Maps could also be constructed to a smaller scale so that less detail is revealed. Alternatively, identifying features (such as the path and road network) can be left out of maps in order to mask exact positions. In fact, it would be advisable to purposely incorrectly draw position markers by a randomly generated value if deemed necessary.
It is well known in the literature that statistical inference based on aggregated data can lead researchers to wrong conclusions, recognizing relationships that do not really exist or remaining hidden relationships that actually exist. This phenomenon is known as the Modifiable Areal Unit Problem ( MAUP ). One example is New York health officials who feared cancer accumulations and causes would be misidentified after they were forced to post maps on the Internet showing cancer cases by zip code. Their rationale was that zip codes were created for a purpose independent of health problems and the use of these arbitrary limits could lead to unsuitable groupings and, consequently, wrong conclusions.
See also
Web links
- National Center for Health Statistics
- GIS and Public Health at Esri
- Consortium for Public Health Informatics
- International Journal of Health Geographics
Individual evidence
- ^ PW O'Carroll (2003). Introduction to public health informatics. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 1-15). New York, NY: Springer.
- ^ JR Lumpkin (2003). History and significance of information systems and public health. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 16-38). New York, NY: Springer.
- ↑ CL Hanchette (2003). Geographic Information Systems. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 431-466). New York, NY: Springer.
- ↑ http://www.cdc.gov/nchs/data/gis/atmappne.pdf , accessed on March 29, 2009
- ↑ WA Yasnoff and PL Miller (2003). Decision Support and Expert Systems in Public Health. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 494-512). New York, NY: Springer.
- ↑ S. Trooskin, J. Hadler, T. St. Louis, and V. Navarro (2005). Geospatial analysis of hepatitis C in Connecticut: a novel application of a public health tool. Public Health, 119 (11), 1042-7. Retrieved from Academic Search Premier database.
- ↑ G. Rushton, R. Krishnamurthy, D. Krishnamurti, P. Lolonis, and H. Song (1996). The spatial relationship between infant mortality and birth defects rates in a US city. Statistics in Medicine, 15, Retrieved from Academic Search Premier database. 1907-19. Retrieved from Academic Search Premier database.
- ↑ CL Hanchette (2003). Geographic Information Systems. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 431-466). New York, NY: Springer.
- ↑ Hanchette, CL (2003). Geographic Information Systems. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 431-466). New York, NY: Springer.
- ↑ Hanchette, CL (2003). Geographic Information Systems. In PW O'Carroll, YA Yasnoff, ME Ward, LH Ripp, and EL Martin (Ed.), Public Health Informatics (pp. 431-466). New York, NY: Springer.
- ^ Rushton G, Elmes G, McMaster R (2003). Considerations for improving geographic information research in public health. URISA Journal, 12 (2), 31-49.