Brown-Séquard syndrome
| Classification according to ICD-10 | |
|---|---|
| G83.88 | Brown-Séquard syndrome |
| ICD-10 online (WHO version 2019) | |
The Brown-Séquard syndrome is a complex of symptoms that occurs when the spinal cord is damaged on one side , resulting in dissociated sensory disorders and muscle paralysis. It was first described between 1850 and 1851 by the neurologist Charles-Édouard Brown-Séquard and usually occurs when the spinal cord is crushed or otherwise injured, and rarely with tumors in the spinal canal .
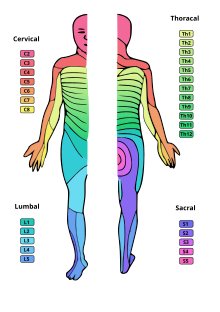
Since the spinal cord consists of both descending motor and ascending sensory nerve tracts , some of which change (cross) to the other side of the marrow, in contrast to total paraplegia, only one-sided lesion of the spinal cord results in an apparently diffuse clinical picture: while it is on the Half of the body, on the side of which the lesion is in the spinal cord (ipsilateral), paralysis of the voluntary muscles and impairment of depth and fine sensitivity occur, on the other side (contralateral) disturbances of temperature, pressure and pain perception occur.
pathology

Anatomical backgrounds
The sensitive afferents for the gross perception ( protopathic sensitivity , gross pressure, temperature and pain sensation ) enter the spinal cord through the posterior root and cross over to the other side (contralateral) in the same segment . From here they run as the spinothalamic tract , consisting of a lateral (5a) and an anterior (5b) tract, to the thalamus and from there, after switching over, to the sensitive area of the cerebral cortex .
The afferents for conveying fine ( epicritical sensitivity ) and deep sensitivity , on the other hand, increase in the posterior cord ( funiculus dorsalis or, in humans, also funiculus posterior , consisting of fasciculus gracilis (3a) and fasciculus cuneatus (3b)) from the posterior root on the same side (ipsilateral) ) of the spinal cord to the brain and only cross to the other side in the area of the extended marrow .
Likewise, the lateral cords of the cerebellum - consisting of the tractus spinocerebellares posterior (4a) and anterior (4b) - do not cross, but rise on the same side as the cerebellum . The tractus spinocerebellaris posterior predominantly conducts proprioceptive impulses, i.e. those of self-perception, the tractus spinocerebellaris anterior both proprio- and exteroceptive , i.e. those of external perception, the localization and quality of a tactile sensation.
Between 70 and 90 percent of the nerve fibers of the pyramidal tract , which is responsible for fine motor skills, cross in the extended marrow in front of the spinal cord and then descend in the lateral cord as the lateral corticospinal tract (1a). The remaining fibers descend ipsilaterally in the anterior cord as the anterior corticospinal tract (1b) and either do not cross at all or only cross at the terminal level.
Likewise ipsilaterally, the extrapyramidal orbits (2a – d) responsible for coarser movement sequences descend like vegetative orbits .
Consequences of a hemilateral lesion
A half-sided transection of the spinal cord results in the interruption of many nerve cords, crossing as well as non-crossing, which leads to neurological failures on both sides. Since the spinothalamic tract crosses before it ascends, a disturbance of gross perception occurs contralateral (on the opposite side of the body) to the lesion and from this downwards: pain and temperature sensation are disturbed. Since neither the posterior cord ( funiculus dorsalis or posterior ) nor the cerebellar lateral cords cross before ascending, a massive disturbance of depth sensitivity and a loss of vibration sensation occur ipsilateral (on the same side of the body) to the lesion and downwards from this. In addition, a small anesthetic zone occurs ipsilateral to the lesion and just above it, which is attributed to the destruction of the posterior root entry zone at the level of the lesion. The severing of the motor tracts (pyramidal tract, extrapyramidal tracts) results in a spastic paresis ipsilateral from the location of the damage downwards . In the affected segment, however, the paresis is flaccid because the motor anterior horn cells themselves are included in the lesion. On the injured side can Hyperesthesia exist already felt a light touch in as pain (hyperalgesia). It is said to be due to the fact that the protopathic sensitivity is retained ipsilaterally with a simultaneous loss of epicritical sensitivity. In addition, due to the damage to the central sympathetic tract, which descends in the lateral cord, the blood vessels expand ipsilaterally, initially the skin reddens and warms up, later it cools down and turns bluish . Sweat production in the same area has decreased or has ceased .
Since vegetative pathways descend on both sides, a pure Brown-Séquard syndrome usually does not lead to bladder , rectal or potency disorders . A lesion at the level of the cervicothoracic junction (C 7 / Th 1 ) also leads to ipsilateral Horner syndrome .
|
|
|
|
|
clinic
causes
Brown-Séquard syndrome in its pure form is rare. A variety of causes are possible. The more common ones include penetrating or blunt injuries, epi- or subdural hematomas of the spinal cord membranes , herniations of the intervertebral discs in the cervical region, or local primary tumors or metastases. Spinal canal stenosis can rarely manifest itself as Brown-Séquard syndrome. The occlusion of a sulcocommissural artery, these are branches from the anterior spinal artery that only supply one side of the anterior spinal cord, sometimes leads to an incomplete Brown-Séquard syndrome with preserved epicritical sensitivity.
Diagnosis
At first glance, the patient experiences symptoms that appear diffuse: the half of the body on the side of the damage is paralyzed below the lesion and its sense of position is severely restricted - at the same time, he feels neither pain nor temperature on the apparently intact side.
Pure Brown-Séquard syndrome is a rarity. Often incomplete forms occur, or due to the frequent damage to the other half of the spinal cord, paraparesis is found instead of the expected hemiparesis.
The diagnostic focus is on a neurological examination with a corresponding examination of the motor skills, the sense of temperature and surface and depth sensitivity. For localization determination of the height of the lesion one orientates oneself on the upper limit of the epicritical loss of sensitivity (“sensitive mirror”); the delimitation of the loss of protopathic sensitivity, on the other hand, is fuzzy, since these paths cross over several segments. The segmental flaccid paresis can be masked, as neighboring spinal nerves have a certain overlap area in their supply area - the decisive factor here is the extent of the spinal cord damage in the cranio-caudal direction.
The main imaging techniques used to determine the extent and cause of the lesion are x-rays , computed tomography, and magnetic resonance imaging .
therapy
If the lesion is based on a tumor that is pressing on the spinal cord, the spinal cord can be relieved by surgical removal of the tumor.
If the symptoms appear acute and mechanical spinal cord compression can be identified, the patient must be operated on immediately.
Although spinal surgery does little to improve neurological deficits, it facilitates patient remobilization and aftercare in the further course of treatment, the long-term results are better and the patient's ability to use a wheelchair is also better.
Physiotherapy should be considered after medical care .
swell
- Werner Kahle: Pocket Atlas of Anatomy . Volume 3: Nervous System and Sense Organs . 8th edition, Thieme, Stuttgart / New York 2002, ISBN 3-13-492208-8 .
- K. Masuhr, M. Neumann: Dual Series - Neurology . 4th edition, Hippokrates Verlag, Stuttgart 1998, ISBN 3-7773-1334-3 .
Individual evidence
- ↑ C.-E. Brown-Séquard: De la transmission croisée des impressions sensitives par la moelle épinière. In: Comptes rendus de la Société de biologie . (1850) 1851, 2, pp. 33-44.
- ↑ a b Masuhr, Neumann: Dual Series - Neurology . 4th edition, p. 123.
- ↑ a b c Kahle: Pocket Atlas of Anatomy . Volume 3: Nervous System and Sense Organs . 8th edition, p. 56.
- ^ Kahle: Pocket Atlas of Anatomy . Volume 3: Nervous system and sense organs 8th edition, p. 58, p. 309.
- ↑ a b Kahle: Pocket Atlas of Anatomy . Volume 3: Nervous System and Sense Organs . 8th edition, p. 68.
- ↑ a b Mumenthaler, Bassetti, Daetwyler: Neurologische Differentialdiagnostik 5th edition, p. 16.
- ↑ S. Sani et al .: Cervical stenosis presenting with acute Brown-Sequard syndrome: case report . In: Spine. 2005, 30 (16), E481-3, PMID 16103843 .
- ^ A b Röscher, Rüther: Orthopedics and trauma surgery . 19th edition.
