OHIP
The Oral Health Impact Profile ( OHIP ) is a method for measuring the oral health- related quality of life in adults. The OHIP is used in dentistry as part of the anamnesis to record dental-relevant problems, but also to monitor the success of therapies and to measure progress. It is also used in oral epidemiology and for research into oral health-related quality of life. The original English language OHIP-E was originally developed in Australia by Garry D. Slade and A. John Spencer and contains 49 questions. Since then, various short versions have been developed, translated and validated in different languages in a culture-equivalent manner. The translation and validation of the German version was done by Mike T. John and others and has been available since 2002. The OHIP can be used without license fees. Internationally, it is the most widespread and scientifically best-researched method for recording oral health-related quality of life.
Content
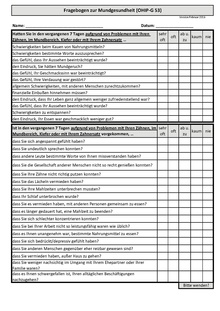
The individual questions (called items) cover important problem areas (called dimensions or domains) of the perceived oral health. While originally seven problem areas were used to group the questions (functional limitation, pain, psychological discomfort / discomfort, physical impairment, psychological impairment, social impairment, disadvantage / disability), today function, pain, aesthetics, and psychosocial influence are the four dimensions respected the MLQ. The response options for the frequency of the problems occurring can be specified by the patient on a multi-level scale (“never” = 0, “rarely” = 1, “now and then” = 2, “often” = 3, “very often” = 4) . The total impairment of a patient as a measure is calculated from the sum of the individual values and can assume values between 0 (= no complaints / impairments) and 196 for the OHIP with 49 questions.
application
The OHIP can describe the individual oral health status of patients and measure and compare disease-related stress over the course of the process. In clinical use, similar to abnormalities in the anamnesis questionnaire, questions are asked about the background of the problems or impairments marked with “Often” or “Very often”. In this context, it is used to record structured, standardized problems. By forming the difference between the summed values before and after therapeutic interventions, the therapeutic effect can be calculated for the individual case, but also for patient groups.
Versions
The German long version, the OHIP-G53, contains 4 additional questions in addition to the 49 original ones. In order to maintain international comparability, only the original OHIP-49 questions are used to calculate the total value. Short versions with twenty-one (OHIP-G21), fourteen (OHIP-G14) and five (OHIP-G5) questions are also available. In contrast to the English-language original version, which uses a reference period of 3 months, all questions in the German version (OHIP-G) refer to the period of the last month.
Administration mode
The questionnaire can be collected in a personal interview (for example by the dentist), in the telephone survey, online, but also by filling out the patient himself. A substantial influence on the OHIP total value in the comparison of personal interviews, telephone interviews and self-completion has not been noticed so far.
material
The templates available here contain the median values (mean value of the general population) and the 90th percentile (value that 10% of the population exceeds) from the German reference publications in order to be able to better interpret OHIP sum values. In the current literature, a reference period of 7 days is recommended for recording the oral health status and for a more comprehensive inclusion of the structures of the masticatory system, the addition of the term “jaw” is recommended.
Interpretation of OHIP sum values
Cumulative values obtained from individual persons or groups of persons can be interpreted using comparative values obtained from the normal population. Since dentures are an important influencing factor for oral health-related quality of life, OHIP norm values are divided accordingly. Standard values are available for the OHIP-G49 as well as the OHIP-G14 and the OHIP-G5. OHIP totals can also be interpreted based on the absolute frequency of oral health problems. Differences in sum values (e.g. the difference before and after a treatment) can be interpreted using the Minimal Important Difference (MID). This is 6 points for the OHIP-G49 and 2 points for the OHIP-G14,
restrictions
The questionnaire does not adequately reflect aesthetic impairments. The problem-oriented approach is also occasionally criticized in the literature, but without showing suitable alternatives. If you are under the age of 15, instruments for children such as B. the Child Perceptions Questionnaire G11-14 apply.
Application examples
The German version of the OHIP was used, among other things, for patients with dentures such as dental implants, craniomandibular dysfunctions (CMD), oral mucosa and periodontal diseases , hypersensitive teeth, extensive loss of tooth structure, fear of dental treatment and misaligned jaws.
Individual evidence
- ^ GD Slade, AJ Spencer: Development and evaluation of the Oral Health Impact Profile. In: Community Dent Health. 11, 1994, pp. 3-11.
- ↑ MI MacEntee, M. Brondani: Cross-cultural equivalence in translations of the oral health impact profile. In: Community Dent Oral Epidemiol. 110, 2015, pp. 425-433.
- ^ MT John, DL Patrick, GD Slade: The German version of the Oral Health Impact Profile - translation and psychometric properties. In: Eur J Oral Sci. 110, 2002, pp. 425-433.
- ↑ O. Schierz, C. Hirsch, MT John, DR Reisman: oral health-related quality of life - human scale in dentistry. In: Senior Dentistry. 3, 2015, pp. 17-22.
- ^ MT John, DL Miglioretti, L. LeResche, TD Koepsell, P. Hujoel, W. Micheelis: German short forms of the Oral Health Impact Profile. In: Community Dent Oral Epidemiol. 34, 2006, pp. 277-288.
- ^ DR Reissmann, MT John, O. Schierz: Influence of administration method on oral health-related quality of life assessment using the Oral Health Impact Profile. In: Eur J Oral Sci. 119, 2011, pp. 73-78.
- ↑ N. Waller, M. John, L. Feuerstahler, K. Baba, P. Larsson, S. Peršić et al: A 7-day recall period for a clinical application of the Oral Health Impact Profile questionnaire. In: Clin Oral Investig accepted.
- ↑ P. Larsson, T. List, I. Lundstrom, A. Marcusson, R. Ohrbach: Reliability and validity of a Swedish version of the Oral Health Impact Profile (OHIP-S). In: Acta Odontol Scand. 62, 2004, pp. 147-152.
- ^ MT John, TD Koepsell, P. Hujoel, DL Miglioretti, L. LeResche, W. Micheelis: Demographic factors, denture status and oral health-related quality of life. In: Community Dent Oral Epidemiol. 32, 2004, pp. 125-132.
- ↑ MT John, L. LeResche, TD Koepsell, P. Hujoel, DL Miglioretti, W. Micheelis: Oral health-related quality of life in Germany. In: Eur J Oral Sci. 111, 2003, pp. 483-491.
- ↑ MT John, W. Micheelis, R. Biffar: Standard values of oral health-related quality of life for short versions of the Oral Health Impact Profile. In: Switzerland Monthly Dental Medicine. 114, 2004, pp. 784-791.
- ↑ DR Reisman, I. Sierwald, G. Heydecke, MT John: Interpreting one oral health impact profile point. In: Health Qual Life Outcomes. 11, 2013, p. 12.
- ^ MT John, DR Reissmann, A. Szentpétery, J. Steele: An approach to define clinical significance in prosthodontics. In: J Prosthodont. 18, 2009, pp. 455-460.
- ↑ DR Reissmann, M. Krautz, O. Schierz, MT John, M. Rudolph, A. Szentpetery: What is clinically relevant in the case of changes in oral health? In: Deutsche Zahnärztl. Z 63, 2008, pp. 668-680.