Large intestine
The large intestine ( Latin intestinum crassum ) is the last part of the digestive tract of vertebrates and therefore also of humans. It is the part of the intestine that begins after the small intestine and ends at the cloaca or anus . Its main function is to transport and store the chair . The large intestine draws water from the stool and thickens it. By its ability to sodium -, potassium - and chloride - ion accommodate or eliminate, it is on the fine regulation of the electrolyte involved -Haushaltes. The intestinal flora is mainly found in the large intestine. Colon disorders are common in humans: Acute appendicitis is a common surgical condition and colon cancer is one of the most common cancer diagnoses.
Comparative anatomy of the large intestine

The large intestine is the part of the midgut (intestine) that is differentiated from the small intestine in vertebrates , i.e. the middle section of the intestine between the stomach and the appendage organs and the cloaca or anus. In the simplest case, both midgut sections form a simple and elongated tube in which both the enzymatic decomposition and the absorption of the nutrients take place. This simple form is found in the hagfish , the lampreys and the bony fish . In the cartilaginous fish, the midgut is characterized by a specific fold formation to increase the surface, which, depending on the taxon, runs more or less helically and is referred to as a spiral intestine .
Amphibians and reptiles usually only have a short large intestine in a few loops. The appendix is small or absent. In both groups, the colon ends in a short rectum and then in the cloaca. There are two sections of the large intestine in birds: the appendix and the rectum. The structural differences mainly affect the appendix, which is created in pairs in birds. Hens and ostriches, for example, have large appendixes, while they are very small in pigeons and have no digestive function and are completely absent in parrots and many birds of prey and passerine birds.
With the exception of the monotremes , mammals are the only group of animals in which the sexual opening and the intestinal outlet are separated in the form of an anus. The large intestine shows considerable differences in structure within mammals. Predators have a small appendix, a simple U-shaped colon and a short rectum , none of which have any ligament stripes (tänien). The intestines of primates correspond to the structure in humans, which is detailed in this article. On the other hand, some herbivores such as horses or herbivorous rodents have a very large appendix, which they use as a fermentation chamber. The ascending part of the colon ( ascending colon ) in particular shows considerable variations in shape; in herbivores it is greatly enlarged. In horses, for example, the loops of the ascending colon are arranged in the form of two superimposed horseshoes open to the rear, in pigs they are rolled up like a hive and in ruminants they are rolled up in a disc shape (for details see the article on the respective section of the large intestine). The number of ribbon strips is also different for each species. Elephants have a very long intestine totaling around 25 meters in length, 6 meters of which are in the large intestine and 4 meters in the rectum. In whales , the small intestine and the large intestine can only be distinguished on the basis of the epithelial cells.
Colon anatomy in humans
Location and structure
The large intestine lies mostly in the abdominal cavity , where it frames the loops of the small intestine . In most people it begins in the right lower abdomen , where the small intestine joins laterally and forms the empty intestine-appendix valve ( ileocecal valve , Bauhin valve). Below the confluence of the colon ends blind, according to this section is appendicitis (cecum) called. At its end, the cecum narrowed to appendix (vermiform appendix) , whose position is variable. Above the ileocecal valve begins the colon (Colon) , which below the liver ascends (ascending colon) , below the liver leftward bends (Flexura coli dextra) and across the abdominal cavity in the left upper abdomen moves ( transverse colon , and transverse colon called). Here it bends again (flexura coli sinistra) and descends into the pelvis (descending colon) , where it then pulls back in an S-shape (dorsal) to the sacrum ( sigmoid colon ) . There it bends downwards (caudally) , leaves the abdominal cavity and forms the rectum. This is divided into the rectum and the anal canal . The total length of the colon in humans is about 1.5 meters.
The individual sections can be intraperitoneal, retroperitoneal and extraperitoneal. This means the position to the peritoneum (peritoneum) . An organ lies intraperitoneally when it is completely covered by the peritoneum and is suspended from the trunk wall with a wide band ( mesentery , meso ), which means that it can move relatively freely. In the large intestine, this applies to the appendix, appendix, transverse colon and sigmoid colon. Retroperitoneal means that the organ is not covered on all sides by peritoneum, but is attached directly to the trunk wall on one side. This applies to the ascending and descending colon ( ascending colon , and descending colon ) and the upper rectum. An organ lies extraperitoneally when it lies outside the abdominal cavity and is therefore not covered by the peritoneum. In the case of the large intestine, this applies to the end of the rectum and the anal canal.
The wall of the colon is characteristic of the large intestine. It is characterized by three visible longitudinal muscles, which are called ligamentous strips, crescent-shaped indentations (plicae semilunares) and bulges (Poschen or Haustren) between the indentations (see section Fine construction ) .
Blood supply and lymph drainage
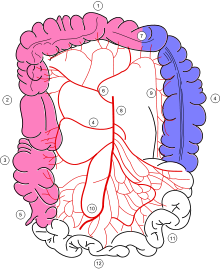
The sections of the large intestine are supplied by the branches of three large arteries. The appendix, appendix, ascending colon and most of the transverse colon receive branches from the superior mesenteric artery , the remainder of the transverse colon, the descending colon, the sigmoid colon, and the upper rectum receive branches from the inferior mesenteric artery . The lower rectum and anal canal receive blood from the internal pudendal artery . Blood drains through veins that run with the arteries and are named identically, i.e. through the superior mesenteric vein , inferior mesenteric vein and internal pudendal vein . The first two of them flow into the portal vein of the liver , only the internal pudendal vein flows into the internal iliac vein , the blood of which enters the inferior vena cava without passing through the liver.
Since lymph vessels usually run with arteries, the lymph drainage areas of the large intestine roughly correspond to the arterial supply areas. The lymph from the flow area of the superior mesenteric artery flows via the mesenteric lymph nodes at the exit point of the artery from the abdominal aorta (noduli mesenterici superiores) into the intestinal trunk , which opens into the chyle cistern . The lymph from the area of the inferior mesenteric artery reaches the cisterna chyli via the lymph nodes next to the arterial outlet (noduli mesenterici inferiores) and via the left lumbar trunk .
Innervation
In the wall of the intestine there is a network of nerve cells that coordinates the movements of the intestine. This so-called enteric nervous system works largely autonomously, but its activity is influenced by the two parts of the autonomic nervous system : the parasympathetic nervous system increases intestinal activity, the sympathetic nervous system decreases it. Similar to the arterial supply, the large intestine is innervated differently until shortly before the left colonic flexure than the intestine behind it. The parasympathetic fibers for the first section originate from the vagus nerve , those for the second section arise from the lowest part of the spinal cord and run as the pelvic splanchnic nerves . The area in which the innervation areas overlap is referred to as the Cannon-Böhm point .
Feinbau
The large intestine shows the typical wall structure of the gastrointestinal tract with four layers. The innermost layer is a mucosa ( tunica mucosa , short mucosa ), which in turn is composed of three layers: the surface is covered with epithelium (epithelial layer) covering the by loose connective tissue ( lamina propria mucosae) by a layer of smooth muscle cells (Lamina muscularis mucosae) is separated. The mucous membrane rests on a loose layer of connective tissue ( tunica submucosa , or submucosa for short ). This leads the blood and lymph vessels for the mucosa and contains a nerve plexus, the submucosal plexus . It also serves as a shifting layer to the third wall layer, the tunica muscularis , which enables the organ to perform peristaltic movements with an inner circular muscle layer (stratum circulare) and an outer longitudinal muscle layer (stratum longitudinal) . Another nerve plexus lies between the muscle layers, the myenteric plexus , which, like the submucosal plexus, belongs to the enteric nervous system . The fourth layer is either loose connective tissue ( adventitia ) or the peritoneum , depending on the section of the large intestine .
An important structural difference to the small intestine is the lack of intestinal villi ; the mucous membrane of the large intestine only has deep crypts , which are lined with cylindrical cells (highly prismatic epithelium) . Many of these cells produce lubricating mucus, while others absorb water and thus thicken the stool . The wall of the large intestine, like the wall of the small intestine, is also wrinkled. However, these arise through local retractions of the inner circular muscle layer, which appear crescent-shaped in cross-section (hence the Latin name Plicae semilunares ). Between the retractions, the intestinal wall forms bulges called Haustren (German: Poschen). In some mammals, including humans, the outer longitudinal muscle layer is thickened into three strong strands ( tänien ). On the outside of these tänien are accumulations of fatty tissue (appendices epiploicae) . The vermiform appendix deviates from this pattern . It has no tänien, but like the other sections of the digestive tract, a continuous layer of longitudinal muscles. Large lymph follicles are found in the lamina propria of the mucous membrane . Instead of the tänien, the rectum has a continuous longitudinal muscle layer, no doors and no fat appendages. At the anal canal , the epithelium of the rectum changes into multi-layered uncornified squamous epithelium .
Development and malformations
From the endoderm , the inner cotyledon of the embryo , the primitive intestinal tube initially develops, on which the foregut, middle and hindgut can be distinguished. As the midgut continues to develop, most of the small intestine and large intestine, including the first two thirds of the transverse colon, emerge. The rest of the colon is formed from the hindgut, while the last piece of the anal canal is formed by the invagination of the ectoderm . The development of the intestine also explains the innervation and blood supply: the midgut artery becomes the superior mesenteric artery and the rectal artery becomes the inferior mesenteric artery .
In the course of development, the ascending colon and descending colon grow together with the back wall of the trunk. In the ascending colon , this adhesion can be incomplete and, in extreme cases, not take place at all, so that like the transverse colon, it has its own mesentery . The ascending colon is then abnormally mobile, volvulus or entrapment of small intestinal loops can occur. During embryonic development, the intestine rotates and “packs” itself in the abdominal cavity. Errors can also occur in this process, with the result that the entire large intestine is on the left side or the transverse colon comes to lie behind the duodenum. As atresia is called the closure of hollow organs: In the colon are most commonly affected rectum and anal canal, in the Rektoanalatresie the connection between the two sections and the colon ends blindly missing. The rectum is often connected to adjacent organs by fistulas . In boys this is often the urethra , in girls the vagina . In the congenital megacolon (Hirschsprung's disease) , nerve cells are usually missing in the end section of the large intestine, which causes the muscles in the affected area to contract and the intestine to close. The intestinal contents build up at the constriction and expand the large intestine ("megacolon").
function
The large intestine absorbs the chyme from the small intestine, transports it on, stores it in the rectum and ultimately excretes it. It removes more water from it by absorbing sodium ions. In addition, it is also involved in the regulation of the chloride and potassium ion balance, whereby, in contrast to the small intestine, it is also able to actively secrete potassium ions. Apart from short-chain fatty acids , no nutrients are absorbed in the large intestine. The bacteria of the large intestine, the intestinal flora, play an important role in the formation of these fatty acids .
Chair transport
The ileo-caecal valve separates the last section of the small intestine, the ileum , from the cecum. At rest this flap is partially closed, so that a slow passage of the food pulp is possible. The passage of the chyme from the ileum into the appendix takes place more intensely when food is ingested: the gastric distension leads via a reflex to increased peristalsis of the ileum and via the release of the hormone gastrin to relax the sphincter belonging to the valve. The food porridge is transported in the small intestine at a fairly constant rate. So chyme accumulates in front of the ileocecal valve and stretches the ileum. Without the relaxing effect of the gastrin, the stretching of the ileum causes the sphincter to contract, so without food the passage of the chyme is blocked.
After the passage of the ileo-caecal sphincter, the chyme collects in the cecum and in the ascending colon. Local movement is typical of all sections of the colon. A front door fills up to a certain degree and then contracts, pushing its contents into the neighboring front door. In addition, a very slow propulsive peristalsis can be observed, in which the constrictions between the house doors move towards the anus, so to speak. Segmentation movements can be observed in the ascending colon and the transverse colon, which mix the stool. Occasionally, antiperistalsis occurs in the transverse colon, driving the stool back into the appendix. In connection with food intake, so-called mass peristalsis occurs: triggered by the expansion of the stomach, a peristaltic wave is created in the middle transverse colon, which quickly transports the stool via the descending colon and the sigmoid colon into the rectum ( gastrocolic reflex ).
The bowel movement is a reflex triggered by the stretching of the rectal wall. The longitudinal muscles of the rectum contract, shortening it and increasing the pressure. The internal sphincter muscle of the anus is involuntarily relaxed. By voluntarily relaxing the external sphincter muscle, the rectum can empty.
The total passage time of the colon varies greatly from person to person and ranges from 12 to 48 hours.
Water, electrolytes and nutrient absorption
The large intestine absorbs less than 2 liters of water a day than the small intestine, but it can increase absorption to 4 to 5 liters. The water transport takes place basically via the resorption of sodium ions: These are actively absorbed, the water follows passively ( osmosis ) . The cells of the large intestine, like the cells of the small intestine, are able to absorb sodium, potassium and chloride ions and, in the case of chloride, also excrete them, although the cellular mechanisms behind them are different. Two essential differences are that the colon cells also absorb sodium ions against a concentration gradient and not only absorb potassium ions, but also excrete them. The large intestine thus plays an important role in the fine regulation of the potassium balance. Carbohydrates and proteins that get into the colon are broken down by bacteria there. The large intestine can only absorb the short-chain fatty acids that are produced.
Bacterial colonization
In all animals, the intestines are colonized by bacteria , which together form the intestinal flora . The composition of the intestinal flora and the distribution of bacteria differ between herbivores, carnivores and omnivores. The bacteria live in symbiosis with their host by digesting non-digestible food components and making them accessible. Since the bacteria have to work anaerobically in the absence of oxygen , it is a fermentation process .
In carnivores and humans, a large part of the intestinal flora is found in the large intestine. When fermenting the porridge, they primarily produce short fatty acids that are absorbed by the large intestine. In addition, there is vitamin K , which is also absorbed.
While ruminants ferment the indigestible components of plant food, namely cellulose , xylan , pectin and other polysaccharides , in their rumen , these processes take place in horses, donkeys, most other odd-toed ungulates and rabbits in the appendix and colon.
The type and quantity, so to speak, the ecosystem of the various bacteria in the colon is the subject of current research. Diet, but also human-to-human transmission, play a role here. The immune system and diseases are influenced by this; stool transplantation is one possible intervention .
Colon diseases
Inflammation
Inflammation of the large intestine is commonly called colitis . Inflammation of the appendix ( appendicitis ) is the most common inflammation in the abdomen. Colon inflammation is caused by infections with pathogens, allergies , certain medications, radiation, insufficient blood flow or unknown factors that play a role in the development of inflammatory bowel diseases , for example .
Infectious colitis
With gastroenteritis , i.e. gastrointestinal inflammation, the large intestine is usually also affected. Such inflammation results from infection with bacteria, viruses and, less often, parasites . Common bacterial pathogens are special types of Escherichia coli ( EHEC , ETEC , EIEC and EPEC ), some Yersinia and Campylobacter species, as well as enteric salmonella and cholera pathogens . In some cases, tuberculosis also manifests in the colon. Small-scale outbreaks of infectious gastroenteritis are often caused by viruses, predominantly noroviruses , and more frequently rotaviruses in young children . Less common viral pathogens are Astro virus , sapoviruses and Human adenovirus F . Bacterial gastroenteritis predominates in Central Europe in the summer months, while viral ones in autumn and winter.
A disease that only affects the large intestine is dysentery (dysentery). In Central Europe it is mainly caused by Shigella (bacterial dysentery). Amoebic dysentery is more widespread in tropical and subtropical regions , the pathogen Entamoeba histolytica of which settles mainly in the colon and liver . If the immune system is poor, for example in people with AIDS , other pathogens can trigger the disease, including some atypical mycobacteria ( MOTT ), cryptosporidia and Candida fungi. Colitis due to reactivation of the cytomegalovirus occurs rarely in immunodeficient patients . In tropical regions, infection with schistosomes also plays a role. The disease caused by these worms is called schistosomiasis .
Inflammatory bowel disease

The chronic inflammatory bowel diseases usually include Crohn's disease and ulcerative colitis , which occur with about the same frequency in Germany with 5–6 new cases per 100,000 inhabitants per year. It is characterized by a permanent (chronic) immune reaction in the intestinal wall that occurs in spurts. In both diseases, the triggers and mechanisms by which the disease develops are still unclear. In 1950, Franz Alexander counted it among the seven psychosomatic diseases, the “ Holy Seven ”, this thesis is now considered outdated. In the meantime, genetic factors have also been identified that could play a role in the development of the diseases. Crohn's disease and ulcerative colitis differ in terms of the course of the disease and its appearance (morphology).
Crohn's disease is the inflammation of the entire intestinal wall with all layers, which is why fistulas (for example anal fistulas ) often occur. Basically the entire digestive tract can be affected, but typically the inflammation affects the end of the small intestine ( ileum ) and the large intestine. The inflammation does not spread continuously from the place of origin, but "jumps" from section to section. Crohn's disease often does not heal completely and is characterized by a high rate of recurrence, i.e. recurring inflammation.
In ulcerative colitis, however, the inflammation is limited to the mucous membrane. As a rule, the inflammation begins acutely in the rectum and spreads from there continuously to the rest of the colon. If the whole colon is affected, it is called pancolitis . In about 10 to 20% of pancolitides, what is known as "backwash ileitis" occurs, in which the inflammation spreads to the ileum of the small intestine. Ulcerative colitis is also recurrent, i.e. with recurring attacks. However, the intestine usually heals completely between attacks. In the acute fulminant course, the toxic megacolon is a rare but life-threatening complication with the risk of purulent peritonitis . Ulcerative colitis increases the risk of developing colon cancer.
Another, poorly researched disease is microscopic colitis , which can also be counted as a chronic inflammatory bowel disease. It causes watery diarrhea, but no changes in the mucous membrane that can be seen with the naked eye or endoscope. The diagnosis can only be made by microscopic examination of the mucous membrane after the biopsy . A distinction is made between two forms: Lymphocytic colitis is characterized by an increase in certain immune cells, the lymphocytes , in the epithelium. Collagenic colitis corresponds to lymphocytic colitis; in addition, a layer of collagen fibers has formed under the basement membrane of the mucous membrane epithelium .
Ischemic colitis
An ischemic colitis occurs when the colonic mucosa (frequently due to vascular constrictions or occlusions atherosclerosis ) not at all or no longer sufficiently supplied with blood and is damaged thereby ( mesenteric ischemia ) . The response to the tissue damage is inflammation in the affected area. In the large intestine, the circulatory disturbance is often limited to smaller areas and occurs somewhat more frequently in the area of the left colonic flexure, since this area lies on the border of the supply areas of the superior mesenteric arteries and inferior mesenteric arteries and the anastomoses between the supply areas are no longer in because of arteriosclerosis are able to compensate for circulatory disorders. The rectum is usually not affected because it is adequately supplied from the pelvic arteries.
Drug Associated Colitis
The effects of many drugs can also damage the small and large intestines and cause inflammation (enterocolitis) , such as nonsteroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid or ibuprofen , antibiotics , cytostatic drugs and antihypertensive agents such as diuretics . It is estimated that every tenth inflammation of the (large) intestine is due to the use of NSAIDs. The inflammation heals when the drug is stopped. Antibiotics inhibit the intestinal flora and thereby promote the multiplication of pathogenic bacteria, especially Clostridium difficile , whose enterotoxins attack the colon mucosa and lead to inflammation. Because of the typical changes in the mucous membrane, these inflammations are called pseudomembranous colitis . A severe decrease in the number of neutrophils in the blood ( neutropenia ), often as a side effect of chemotherapy with cytostatics, can lead to severe, necrotizing inflammation of the appendix and ascending colon, known as neutropenic colitis ( typhlitis ) .
Irritable bowel syndrome
The irritable bowel syndrome is a complex of several gastrointestinal symptoms, which is reacted with psychological stress factors in combination and may also occur after intestinal infection. Irritable bowel syndrome is a diagnosis of exclusion that is made when long-lasting symptoms such as abdominal pain, gas and stool changes cannot be reconciled with any other diagnosis. Around half of the patients with gastrointestinal complaints are said to suffer from irritable bowel syndrome.
Diverticulum
Diverticula are generally protrusions of the wall of a hollow organ that are most common in the large intestine. A distinction is made between real diverticula and false diverticula (pseudodiverticula) . In the former, all wall layers are involved in the formation of the diverticulum, in the pseudodiverticula, as a rule, only the mucous membrane is pressed through the muscle layers. Pseudodiverticula can either still lie in the intestinal wall (intramural) or protrude from it completely ( extramural diverticulum). About two-thirds of colon diverticula occur on the sigmoid colon and are typically pseudodiverticula. The frequent occurrence of diverticula, which does not cause any symptoms, is called diverticulosis , which can turn into diverticulitis , i.e. a purulent inflammation of the diverticulum, and must be treated. In the worst case, inflamed diverticula can break open (perforate), which can lead to abscesses in the abdominal cavity and inflammation of the peritoneum.
Tumors
With over 60,000 new cases each year in Germany, the large intestine is the third most common site of cancer, colorectal carcinoma, after the prostate and the mammary gland . The causes are not exactly known; the risk factors include smoking, lack of exercise, obesity, alcohol and red meat. In addition, there are rare hereditary forms such as familial adenomatous polyposis or hereditary non-polypoid colorectal cancer syndrome . The current model of colon cancer development is based on an adenoma-carcinoma sequence . This means that the glandular epithelium of the large intestine degenerates through genetic changes in a multi-stage process: One cell is sufficient for this, which divides uncontrollably due to these genetic changes. The first thing that develops is a benign tumor, an adenoma , which is seen as a colon polyp on colonoscopy . However, the cells of the adenoma are susceptible to further gene mutations, so that at some point cancer cells develop that grow malignantly into the surrounding tissue and divide quickly. Over 90% of colorectal cancers arise from adenomas, which is why removal of an adenoma is always indicated.
Connective tissue tumors are rare, especially in comparison to the epithelial tumors described above. The most common connective tissue tumors are tumors of adipose tissue , smooth muscle cells , lymphatics and gastrointestinal stromal tumors . Malignant lymphomas , especially mantle cell lymphoma , can manifest as lymphomatous polyposis , with numerous polyps in the colon.
Neuroendocrine tumors originate in the gastrointestinal tract from the cells of the diffuse neuroendocrine system . They are very rare in the colon, whereas 13% of all gastrointestinal neuroendocrine tumors are found in the rectum, while almost one in five of these tumors is located on the appendix.
Investigation options
The colon can be examined using the hands and fingers, endoscopic, and other imaging tests .
Palpation of the abdomen as part of the physical exam may reveal tumors of the large intestine. A frequent examination is digital palpation , the scanning with the fingers (from Latin digitus , finger). The examiner inserts a (usually gloved) finger into the anus, feels the anal canal, checks the resting tone and the pressure of the anal sphincter during active tension, pushes the finger into the rectal ampoule and also feels it. In men, the prostate can also be assessed in this way . In this way tumors or painful areas can be identified. Last but not least, stool, blood or pus on the finger can indicate diseases.
Various methods are available for endoscopic examination. The rectoscope is a rigid endoscope that is only suitable for assessing the anal canal and rectum. A sigmoidoscopy to assess the intestine up to the sigmoid colon can be done with a flexible endoscope up to 60 cm long. The colonoscopy (colonoscopy), the endoscopic examination of the entire colon with a long endoscope. It is considered the gold standard for assessing the mucous membrane. With this method, not only visible changes can be described, but also samples can be taken ( biopsied ) and small therapeutic interventions can be carried out (e.g. the removal of a polyp).
The classic ultrasound examination of the abdomen plays a subordinate role in assessing the large intestine. It is useful for diagnosing acute appendicitis and diverticulitis. The EUS is a combined method wherein a rotating probe is inserted to a flexible endoscope in the intestine. This creates a cross-sectional image of the intestine with which all wall layers can be assessed.
The conventional x-ray of the abdomen offers a quick diagnosis. It is suitable for the identification of free air in the abdominal cavity, which gives an indication of the perforation of a hollow organ, for the diagnosis of an intestinal obstruction (ileus) through the detection of air-liquid levels in the intestinal loops or the detection of foreign bodies or introduced materials. The computed tomography allows the assessment of the wall layers of the colon and other organs and lymph nodes, which is why this method for the staging of tumors (staging) is used. Magnetic resonance imaging (MRI) is used in young patients with inflammatory bowel disease because of the lack of radiation exposure . This procedure also plays a role in the staging of rectal cancer. Contrast agent examinations have lost importance because of the spread of endoscopic procedures. They are used when an endoscopic examination is not possible, for example due to a severe stenosis of the intestinal lumen. This technique can be used to visualize diverticula, for example. The functional examination of the process of stool elimination with contrast media or MRI is called defecography .
The chair itself can also be the subject of the investigation. In particular, the detection of visible ( hematochezia ) or invisible ( guaiac test ) blood in the stool can be the starting point for further diagnostics.
Surgical interventions
Surgical interventions can be performed on the large intestine of humans and animals.
These interventions are performed relatively frequently in humans. The following list is intended to give an overview of the typical surgical procedures in humans. The surgical technique is fundamentally different for benign diseases (such as inflammation) and malignant diseases. In the case of malignant diseases such as tumors, according to the principles of oncological surgery, larger parts of the colon and the surrounding tissue are removed in order to remove possible metastases in the lymph vessels and nodes. All procedures can be performed openly with laparotomy or laparoscopically . In laparoscopically assisted surgery, the surgical area is prepared laparoscopically. The resection itself is then performed openly surgically. Which surgical technique is used depends on the type of disease: while laparoscopy is very important for benign diseases, it has long been controversial in colorectal cancer operations. In the meantime, however, it has been proven that the long-term results of laparoscopy in localized tumors are similar to the long-term results of open surgery, so laparoscopy is an established procedure in these cases too.
- Appendectomy : Surgical removal of the appendix is a common operation that is indicated for acute inflammation of the appendix ( appendicitis ). It can be performed openly and laparoscopically with comparable results.
- Ileocoecal resection : The removal (resection) of the last section of the ileum and the appendix may be indicated in the case of limited, benign changes, for example in Crohn's disease .
- Right hemicolectomy : The surgical procedure of choice for carcinomas of the appendix and ascending colon , parts of the transverse colon behind the right colonic flexure are also removed. In the case of high-lying carcinomas in the area of the right colonic flexure, the resection is widened and the transverse colon is removed beyond the left colonic flexure ("extended right hemicolectomy").
- Left hemicolectomy : As with right hemicolectomy, left-sided hemicolectomy removes the descending colon and the sigmoid colon if the carcinoma is located accordingly. This operation can also be extended to include the transverse colon as far as the right colonic flexure if the tumor is located in the area of the left colonic flexure.
- Colon transverse resection : In the case of carcinomas of the transverse colon, an extended hemicolectomy or subtotal colectomy is more commonly performed today ; transverse colon resection has therefore become rare.
- Sigmoid : laparoscopic sigmoid resection is the standard procedure for diverticulitis.
- Subtotal colectomy : removal of the large intestine while preserving the rectum. These operations may be necessary if there are two carcinomas in different parts of the colon.
- Proctocolectomy : The removal of the large intestine including the rectum while preserving the anal sphincter can be indicated in ulcerative colitis and polyposis coli .
- Anterior Rectal Resection: Standard procedure for cancers at the junction of the sigma and rectum, removing the sigmoid and upper rectum. The rectal ampoule is retained. If a carcinoma is located deeper in the middle third of the rectum, the rectum is completely removed in the so-called deep anterior rectal resection while preserving the sphincter apparatus. If the carcinoma is very deep, the sphincter apparatus must also be resected.
- Abdominoperineal rectal amputation : amputation of the rectum including removal of the sphincter apparatus . This operation may be necessary in the case of deep-seated rectal cancer.
- Hemorrhoidectomy : the surgical removal of pronounced hemorrhoids for which various techniques are available.
In veterinary medicine, surgical interventions are mainly carried out on horses with colic , which often originates from the large intestine. Here it is mainly twisting , blockages and invaginations of the appendix and the "large colon" (ascending colon) that can usually only be removed surgically. In dogs and cats surgery especially when are rectum incidents , tumors or a megacolon performed. Anchoring of the descending colon to the back wall of the trunk ( colopexy ) can be indicated in cases of rectal prolapse as well as perineal hernias .
Web links
literature
- Gerhard Aumüller , Jürgen Engele, Joachim Kirsch, Siegfried Mense; Markus Voll and Karl Wesker (illustrations): Anatomy , online learning program for the preparation course. 3. Edition. Thieme, Stuttgart 2014, ISBN 978-3-13-136043-4 (= dual series ).
- Herbert Renz-Polster, Steffen Krautzig (Hrsg.): Basic textbook internal medicine . 5th edition. Urban & Fischer , Munich 2013, ISBN 978-3-437-41114-4 .
- Renate Lüllmann-Rauch: pocket textbook histology . 4th edition. Thieme, Stuttgart 2012, ISBN 978-3-13-129244-5 .
- Franz-Viktor Salomon, Hans Geyer, Uwe Gille: Anatomy for veterinary medicine . Enke, Stuttgart. 2014, ISBN 978-3-8304-1075-1 .
- Jörg Siewert , Hubert Stein: Surgery . 9th edition. Springer-Verlag , Berlin, Heidelberg 2012. ISBN 978-3-642-11330-7 .
- Erwin-Josef Speckmann, Jürgen Hescheler, Rüdiger Köhling: Physiology . 6th edition. Urban & Fischer, Munich 2013, ISBN 978-3-437-41319-3 .
Individual evidence
- ↑ Michael Starck: X intestinal tract. In: W. Westheide, R. Rieger: Special Zoology. Part 2. Vertebrate or skull animals. Spektrum Akademischer Verlag, Munich 2004, ISBN 3-8274-0307-3 , pp. 139 f.
- ↑ Alfred Goldschmid: Chondrichthyes, cartilage fish. In: W. Westheide, R. Rieger: Special Zoology. Part 2. Vertebrate or skull animals. Spektrum Akademischer Verlag, Munich 2004, ISBN 3-8274-0307-3 , pp. 207 f.
- ↑ a b Alexander Haas: Lissamphibia, Amphibians. In: W. Westheide, R. Rieger: Special Zoology. Part 2. Vertebrate or skull animals. Spektrum Akademischer Verlag, Munich 2004, ISBN 3-8274-0307-3 , p. 315.
- ↑ Franz-Viktor Salomon and Winnie Achilles: Reptiles . In: Franz-Viktor Salomon, Hans Geyer and Uwe Gille (eds.): Anatomy for veterinary medicine . 3. Edition. Enke, Stuttgart 2015, ISBN 978-3-8304-1288-5 , pp. 815-842 .
- ^ Franz-Viktor Salomon and Elisabeth Krautwald-Junghanns: Gut . In: Franz-Viktor Salomon, Hans Geyer and Uwe Gille (eds.): Anatomy for veterinary medicine . 3. Edition. Enke, Stuttgart 2015, ISBN 978-3-8304-1288-5 , pp. 779-782 .
- ^ Franz-Viktor Salomon: Large intestine, intestinum crassum . In: Franz-Viktor Salomon, Hans Geyer and Uwe Gille (eds.): Anatomy for veterinary medicine . 3. Edition. Enke, Stuttgart 2015, ISBN 978-3-8304-1288-5 , pp. 314-326 .
- ↑ Martin S. Fischer: Proboscidea, Elefanten. In: W. Westheide, R. Rieger: Special Zoology. Part 2. Vertebrate or skull animals. Spektrum Akademischer Verlag, Munich 2004; ISBN 3-8274-0307-3 , p. 637.
- ^ Milan climate: Cetacea, cetaceans. In: W. Westheide, R. Rieger: Special Zoology. Part 2. Vertebrate or skull animals. Spektrum Akademischer Verlag, Munich 2004; ISBN 3-8274-0307-3 , p. 637.
- ↑ a b c Gerhard Aumüller et al .: Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 636 f.
- ^ Gerhard Aumüller et al .: Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 634.
- ^ Gerhard Aumüller et al .: Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 643.
- ↑ Detlev Drenckhahn (Ed.): Anatomie, Volume 1 . 17th edition. Urban & Fischer, Munich 2008, ISBN 978-3-437-42342-0 , p. 690.
- ↑ Detlev Drenckhahn (Ed.): Anatomie, Volume 1 . 17th edition. Urban & Fischer, Munich 2008, ISBN 978-3-437-42342-0 , p. 694.
- ↑ Michael Schünke u. a .: Prometheus Learning Atlas of Anatomy. Internal organs . 3. Edition. Georg Thieme Verlag, Stuttgart 2012, ISBN 978-3-13-139533-7 , p. 213.
- ↑ Detlev Drenckhahn (Ed.): Anatomie, Volume 1 . 17th edition. Urban & Fischer, Munich 2008, ISBN 978-3-437-42342-0 , p. 691.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 4th edition. Georg Thieme Verlag, Stuttgart 2012, ISBN 978-3-13-129244-5 , p. 386 f.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 4th edition. Georg Thieme Verlag, Stuttgart 2012, ISBN 978-3-13-129244-5 , p. 407 f.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 4th edition. Georg Thieme Verlag, Stuttgart 2012, ISBN 978-3-13-129244-5 , p. 409.
- ↑ Detlev Drenckhahn (Ed.): Anatomie, Volume 1 . 17th edition. Urban & Fischer, Munich 2008, ISBN 978-3-437-42342-0 , p. 692.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 4th edition. Georg Thieme Verlag, Stuttgart 2012, ISBN 978-3-13-129244-5 , p. 410 f.
- ↑ Thomas W. Sadler: Medical Embryology . Translated from the English by Ulrich Drews. 11th edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-446611-9 , p. 295.
- ↑ Thomas W. Sadler: Medical Embryology . Translated from the English by Ulrich Drews. 11th edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-446611-9 , p. 302 f.
- ^ A b Thomas W. Sadler: Medical Embryology . Translated from the English by Ulrich Drews. 11th edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-446611-9 , p. 293, p. 303.
- ↑ Thomas W. Sadler: Medical Embryology . Translated from the English by Ulrich Drews. 11th edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-446611-9 , p. 299 f.
- ^ A b Gerard J. Tortora, Bryan H. Derrickson: Anatomy and Physiology . Translation edited by Axel Pries. Wiley-VCH, Weinheim 2006, ISBN 978-3-527-31547-5 , p. 1084.
- ^ A b Erwin-Josef Speckmann, Jürgen Hescheler, Rüdiger Köhling (editor): Physiology . 6th edition. Urban & Fischer, Munich 2013, ISBN 978-3-437-41319-3 , p. 533.
- ↑ Gerard J. Tortora, Bryan H. Derrickson: Anatomy and Physiology . Translation edited by Axel Pries. Wiley-VCH, Weinheim 2006, ISBN 978-3-527-31547-5 , p. 1085.
- ↑ Michael Gekle et al .: Physiology . Thieme, Stuttgart 2010, ISBN 978-3-13-144981-8 , p. 466 ff.
- ↑ a b c Georg Fuchs: General Microbiology , 9th edition. Georg Thieme Verlag, Stuttgart 2014, ISBN 978-3-13-444609-8 , p. 632.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 582, p. 600.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 600 f.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 602.
- ↑ Gerd Herold and colleagues: Internal Medicine 2013 . Self-published, Cologne 2013, ISBN 978-3-9814660-2-7 , p. 477.
- ↑ Herbert Renz-Polster, Steffen Krautzig (Ed.): Basic textbook internal medicine . 5th edition. Urban & Fischer, Munich 2013, ISBN 978-3-437-41114-4 , p. 550.
- ↑ Gerd Herold and colleagues: Internal Medicine 2013 . Self-published, Cologne 2013, ISBN 978-3-9814660-2-7 , p. 480.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 603.
- ↑ Gerd Herold and colleagues: Internal Medicine 2013 . Self-published, Cologne 2013, ISBN 978-3-9814660-2-7 , p. 481.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 604.
- ↑ a b Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 607.
- ↑ Herbert Renz-Polster, Steffen Krautzig (Ed.): Basic textbook internal medicine . 5th edition. Urban & Fischer, Munich 2013, ISBN 978-3-437-41114-4 , p. 549.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 608.
- ↑ Gerd Herold and colleagues: Internal Medicine 2013 . Self-published, Cologne 2013, ISBN 978-3-9814660-2-7 , p. 485 f.
- ↑ Gerd Herold and colleagues: Internal Medicine 2013 . Self-published, Cologne 2013, ISBN 978-3-9814660-2-7 , p. 486.
- ^ Cancer in Germany 2009/2010. 9th edition. Robert Koch Institute (ed.) And the Society of Epidemiological Cancer Registers in Germany eV (ed.). Berlin 2013, p. 18 online , accessed on July 2, 2015.
- ^ Cancer in Germany 2009/2010. 9th edition. Robert Koch Institute (ed.) And the Society of Epidemiological Cancer Registers in Germany eV (ed.). Berlin 2013, p. 36 online , accessed on July 2, 2015.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 612.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 615.
- ↑ Werner Böcker et al .: Pathology , 5th edition. Urban & Fischer, Munich 2012, ISBN 978-3-437-42384-0 , p. 347.
- ↑ a b c Jörg Siewert, Hubert Stein: Chirurgie . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 706.
- ↑ a b Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 684.
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 682.
- ↑ Maximilian Reiser, Fritz-Peter Kuhn, Jürgen Debus: Radiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2011, ISBN 978-3-13-125323-1 , p. 434.
- ↑ Maximilian Reiser, Fritz-Peter Kuhn, Jürgen Debus: Radiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2011, ISBN 978-3-13-125323-1 , p. 435.
- ↑ Maximilian Reiser, Fritz-Peter Kuhn, Jürgen Debus: Radiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2011, ISBN 978-3-13-125323-1 , p. 439.
- ↑ a b c Jörg Siewert, Hubert Stein: Chirurgie . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 687.
- ↑ J. Reibetanz, C.-T. Gerber: Laparoscopic vs. open surgery for colorectal cancer. 10-year results of the CLASICC trial . In: The surgeon . Vol. 84, No. 3, 2013, p. 234, doi: 10.1007 / s00104-013-2465-4 .
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 689.
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 685.
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 721 f.
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 722.
- ^ Jörg Siewert, Hubert Stein: Surgery . 9th edition. Springer-Verlag, Berlin, Heidelberg 2012, ISBN 978-3-642-11330-7 , p. 710.
- ↑ Hanns-Jürgen Wintzer: Diseases of the horse: a guide for study and practice . Georg Thieme, Stuttgart 1999, ISBN 978-3-8263-3280-7 , p. 220-227 .
- ↑ Cheryl S. Hedlund: Surgery of the large intestine . In: Theresa Welch Fossum (Ed.): Small Animal Surgery . 2nd Edition. Mosby, St. Louis 2002, ISBN 0-323-01238-8 , pp. 398-415 .




