Ependymoma
| Classification according to ICD-10 | |
|---|---|
| C71.7 | Brain stem, IV ventricle, infratentorial onA |
| C72.0 | Spinal cord |
| ICD-10 online (WHO version 2019) | |
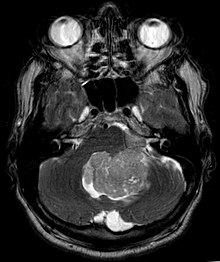

Ependymomas are mostly slowly growing tumors of the central nervous system, which are morphologically similar to the ependymal cells lining the brain cavities and the spinal canal . Two thirds of the ependymomas are located infratentorial on the 4th ventricle, the remaining third are supratentorial and mostly in the periventricular white matter. Although they tend to occur in children and adolescents, ependymomas can occur at any age.
Symptoms
Due to their location near the ventricles, ependymomas often obstruct the flow of cerebrospinal fluid, which can lead to an increase in intracranial pressure . This can result in persistent headaches, nausea and vomiting, and hydrocephalus .
diagnosis
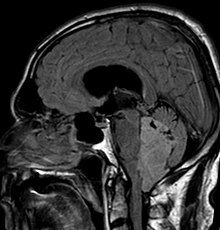
In magnetic resonance imaging of the head, the ependymoma typically presents itself as a circumscribed lesion with reference to the ventricular system, which has a heterogeneous signal pattern with cystic components and a moderate, garland-like accumulation of contrast medium . Calcifications can be seen in the sectional imaging in 50%. Cytological examination of the cerebrospinal fluid as well as tumor biopsy can contribute to the diagnosis.
pathology

According to the WHO classification of tumors of the central nervous system , ependymomas are assigned to grade II, anaplastic ependymomas to grade III. The ependymoblastoma, which is related by name , on the other hand, belongs to the group of primitive neuroectodermal tumors ( PNET ), which are not histogenetically related to ependymomas. A special form is the so-called myxopapillary ependymoma, which is predominantly spinally (in the area of the filum terminale ) and which usually has a more favorable prognosis (WHO grade I).
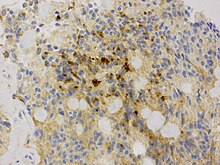
Intraoperatively, ependymomas usually appear as a well-defined, whitish mass. Histologically, they are glial tumors with ependymal differentiation, that is, the tumor cells, like the ependymal cells, tend to form surfaces. So-called ependymal rosettes, in which several tumor cells form a central lumen, are diagnostic. Perivascular pseudorosettes are also typical, in which the tumor cells located around blood vessels align fine fibrillar processes with them. As glial tumors, ependymomas (especially in the area of the perivascular pseudorosettes) express the acidic glial fiber protein ( GFAP ). In addition, intracytoplasmic microlumens can often be detected in the immunohistochemical staining for the epithelial membrane antigen (EMA).
In individual cases, ependymomas can also have unusual histological features such as giant cells, cysts or islands with neuronal differentiation.
therapy
The location directly at the brainstem makes an operation extremely difficult; however, it is the most effective therapy. The importance of radiation therapy for completely removed ependymomas is unclear, but it seems certain that patients in whom a full resection could not be achieved can benefit from radiation therapy. Outside of controlled clinical trials, adjuvant chemotherapy is usually not of major importance. However, in young children, chemotherapy can possibly postpone radiation therapy, which has many side effects in this age group. Current data support this assumption. In children in particular, therapy should be sought as part of clinical studies.
forecast
Since ependymomas are often only partially resected due to their location, the extent of the resection is of particular importance for the prognosis. On the other hand, the neuropathological classification, including a central neuropathological assessment agency, was not classified as prognostically relevant in the study by Robertson and colleagues. Other investigations came to opposite results with an unfavorable prognostic significance of cell density (cellularity), mitosis density (number of mitoses per visual field), endothelial proliferation and degree of differentiation. However, depending on the examination or study carried out, the histological prognostic factors can vary. In addition to the histology or neuropathological classification, age obviously also plays a prognostic role. Children under 3 years of age tend to have a worse prognosis.
Individual evidence
- ↑ Lord et al .: Fourth ventricle ependymoma in father and son. In: Br J Neurosurg , 2007; 1-3. PMID 17952721
- ↑ Prayson & Suh: Subependymomas: clinicopathologic study of 14 tumors, including comparative MIB-1 immunohistochemical analysis with other ependymal neoplasms. In: Arch Pathol Lab Med , 1999; 123 (4): 306-9. PMID 10320142
- ^ Zec et al .: Giant cell ependymoma of the filum terminale. A report of two cases. In: Am J Surg Pathol , 1996; 20 (9): 1091-101. PMID 8764746
- ↑ Arsene et al .: Highly cystic brain tumor: rare histological features in an ependymoma. In: Neuropathology , 2007; 27 (4): 378-82. PMID 17899693
- ↑ Rodriguez et al .: Ependymomas with neuronal differentiation: a morphologic and immunohistochemical spectrum. In: Acta Neuropathol , 2007; 113 (3): 313-24. PMID 17061076
- ^ Grundy et al .: Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG / SIOP prospective study. Lancet Oncol. 2007; 8 (8): 696-705. PMID 17644039
- ↑ a b Robertson et al .: Survival and prognostic factors following radiation therapy and chemotherapy for ependymomas in children: a report of the Children's Cancer Group. In: J Neurosurg. 1998; 88 (4): 695-703. PMID 9525716
- ↑ a b Agaoglu et al .: Ependymal tumors in childhood. In: Pediatr Blood Cancer . 2005; 45 (3): 298-303. PMID 15770637
- ↑ a b Spagnoli et al .: Combined treatment of fourth ventricle ependymomas: report of 26 cases. In: Surgical Neurology . 2000; 54 (1): 19-26. PMID 11024503
- ^ Pollack IF, et al .: Intracranial ependymomas of childhood: long-term outcome and prognostic factors. In: Neurosurgery . 1995; 37 (4): 655-66. PMID 8559293
- ↑ Figarella-Branger et al .: Prognostic factors in intracranial ependymomas in children. In: J Neurosurg . 2000; 93 (4): 605-13. PMID 11014538
- ↑ Prayson: Clinicopathologic study of 61 patients with ependymoma including MIB-1 immunohistochemistry . In: Ann Diagn Pathol . 1999; 3 (1): 11-8. PMID 9990108
- ↑ Kurt et al .: Identification of relevant prognostic histopathologic features in 69 intracranial ependymomas, excluding myxopapillary ependymomas and subependymomas . In: Cancer . 2006; 106 (2): 388-95. PMID 16342252