Rasmussen's encephalitis
| Classification according to ICD-10 | |
|---|---|
| G04.8 | Other encephalitis, myelitis and encephalomyelitis |
| ICD-10 online (WHO version 2019) | |
The Rasmussen's encephalitis, also Rasmussen syndrome and partly in the English language as Chronic Focal encephalitis (CFE) referred to is a by Theodore Rasmussen called progressive inflammation of portions of the cerebral cortex (cerebral cortex). The disease begins in a small area and then spreads to the adjacent areas of a brain hemisphere. The opposite half of the brain is usually not affected. The inflammation leads to the loss of nerve cells with scarring and eventually severe disability.
Epidemiology
The disease is mostly diagnosed in children under 10 years of age, but it can also occur during puberty or in adults. With a frequency of 1: 500,000–1: 1,000,000, it is a very rare disease.
Clinical appearance
Usually the first symptoms of the disease are focal epileptic seizures , later also neurological deficits such as hemiparesis , visual disturbances ( hemianopia ), speech disorders and cognitive disorders.
root cause
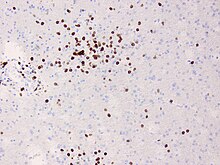
According to a study published in 2009, the disease arises from a targeted attack by the immune system on previously unknown structures in the brain. Cytotoxic CD8- positive T-cell clones seem to attack nerve cells and astrocytes. It is currently unclear whether the triggering structures are structures that belong to the own body or are possibly components of previously unknown viruses. By sequencing T-cell receptors from different compartments, it was possible to show that CD8-cytotoxic cells in particular accumulate strongly clonally and can in some cases be detected over many years.
treatment
In a number of studies, various, sometimes combined, immunosuppressive treatments have been tested; a clear therapy recommendation has not yet resulted. In advanced stages, brain surgery, including hemispherectomy, can be performed. Concomitant anti-epileptic treatment is often difficult and has no effect on the progression of the causative encephalitis.
Individual evidence
- ↑ Alphabetical index for the ICD-10-WHO version 2019, volume 3. German Institute for Medical Documentation and Information (DIMDI), Cologne, 2019, p. 740
- ↑ N. Schwab, CG Bien, A. Waschbisch, A. Becker, GH Vince, K. Dornmair, H. Wiendl : CD8 + T-cell clones dominate brain infiltrates in Rasmussen encephalitis and persist in the periphery. In: Brain. 2009 Jan 29. [Epub ahead of print] PMID 19179379
- ↑ Schneider-Hohendorf T, Mohan H, Bien CG, Becker A, Gorlich D, Kuhlmann T, Widmann G, Herich S, Elpers C, Melzer N, Dornmair K, Kurlemann G, Wiendl H , Schwab N (2016) CD 8 ( +) T-cell pathogenicity in Rasmussen encephalitis elucidated by large-scale T-cell receptor sequencing. Nat Cimmun 7: 11153