Full denture
A full denture (also full denture, popularly "dentition" or "third teeth", in dental jargon "14" or "28" according to the number of teeth replaced) is understood in dentistry to mean the replacement of all teeth and the alveolar bone of one or both of them The jaw thanks to removable dentures , which consist of a plastic base made of polymethyl methacrylate (PMMA) and the artificial teeth made of plastic or porcelain attached to it. A total denture is held in the mouth by suction, adhesion and cohesion forces and the interaction of muscles. For this purpose, the edge of the prosthesis is individually adapted using a functional impression. A full denture not only replaces the teeth, but also the dismantled jaw. The bone loss of the jawbone (jaw loss ) can result from tooth loss , periodontitis or bone resorption caused by the pressure applied by prostheses. A full denture is manufactured hand in hand between the dentist and the dental technician . The dental technology production of a full denture takes place on plaster models in standardized devices. The insertion of the prosthesis into a living organism with all its individual characteristics is one of the greatest challenges for the dentist. The success of the treatment requires great experience. The production of a full denture takes about six treatment sessions, which usually extend over a period of four to six weeks. This is followed by several follow-up sessions, which can extend over a further two to eight weeks.
Hold a full denture
The hold of a prosthesis depends primarily on the shape of the jaw. The larger and more pronounced the alveolar ridge , the better the hold. The prosthetic saddle sits like a riding saddle on the alveolar process. The hold of a prosthesis can deteriorate over many years because the jawbone is subject to bone loss. In edentulous teeth, the pressure on the dentures acts on the gingiva propria (mucous membrane) and thus on the underlying jawbone, which reacts with increased resorption .
The hold of the prosthesis also depends on the static design. This means that the denture teeth in their occlusion (clenching of the upper and lower jaw teeth ) must contribute to a stable position and must not cause the denture to be levered out by chewing movements.
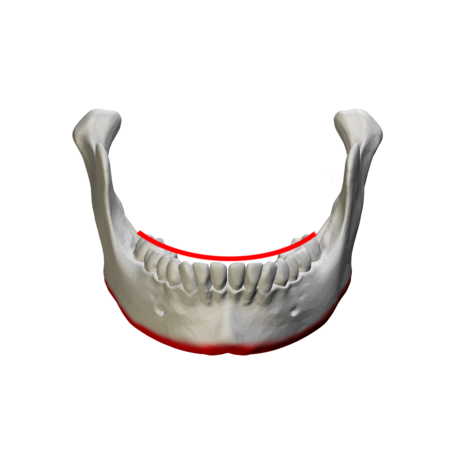
The hold differs between the upper and lower jaw prosthesis. With the latter, the hold is considerably lower due to the smaller contact surface, the reduced suction effect and the movements of the tongue . The hold of the lower jaw prosthesis in particular depends on the interaction of the cheek and tongue muscles that balance the prosthesis. In the lower jaw, a number of muscles have a stabilizing effect, in addition to the buccinator muscle (cheek muscle) and the circular mouth muscles ( orbicularis oris muscle ), the mylohyoid muscle (mandibular hyoid muscle ), the mentalis muscle (chin muscle) and the tongue muscles. In order to compensate for the lower suction effect of the prosthesis, the prosthesis wearer must develop a certain skill to hold the mandibular prosthesis in place through the tongue and the rest of the muscles. In the course of time, the movement pattern of the muscles is imprinted and the hold is thereby unconsciously established.
The mucous membrane (mucosa) contains mucus-forming cells. The formation of slime is important for the adhesion of the prosthesis. The function of the mucus is similar to that of a liquid between two panes of glass, which makes them stick together better. Something similar can be observed when moistening a suction cup . Ultimately, the hold is created by the negative pressure, which corresponds to about a fifth of atmospheric air pressure, between the prosthesis and the mucous membrane. Too little saliva or saliva flow from the salivary glands or a dry mouth (xerostomia) can significantly impair the hold of a prosthesis.
The mucous membrane usually forms mucus continuously. Too much mucus reduces the suction effect, as the increasing mucus increases the distance between the prosthesis and the mucous membrane. Therefore the suction effect of the prosthesis only lasts for about 20 minutes. After this time has elapsed, the prosthesis must be pressed against the jaw again by clenching it firmly in order to attach it again. This clenching presses out the excess mucus between the prosthesis and the mucous membrane.
Differences in occlusion compared to natural teeth
Canine guidance
In natural dentition, the canine guidance ensures that the lower jaw is forced to open when it moves sideways (laterotrusion movement). When the lower jaw moves sideways, the canines of the upper and lower jaw block sideways movement. It is only possible when the canine of the lower jaw slides along the canine of the upper jaw, forcing the mouth to open. As a result, the teeth in the posterior area ( premolars and molars ) get out of contact. The front teeth ( incisors and canines) have the same effect when the lower jaw moves forward, the front teeth of the lower jaw then sliding along the inside of the front teeth of the upper jaw and forcing the molars to open. Due to their long roots, canines are suitable for absorbing lateral load forces, which can lead to loosening of the remaining teeth, which have shorter roots.
Balance contacts
This function does not apply to a full denture. Just guiding the front and canine teeth would cause the prostheses to be levered out and tilted. In exceptional cases, it can serve as a basis, for example in the case of a pronounced ridge and young prosthesis wearers. For this reason, denture teeth are set up and ground in in such a way that there are no levering guide zones. Rather, balance contacts are intentionally made. This means that when the lower jaw moves sideways - in contrast to natural full dentition - the teeth on both sides slide against one another in contact. During the advance movement of the lower jaw, in addition to the front teeth, the molars of the upper and lower jaw prosthesis slide over one another and provide distal (rear) support. For this purpose, the teeth are set up according to the Spee curve (sagittal compensation curve ).
The Wilson curve is important when setting up the artificial teeth in the calotte articulation of full dentures. The posterior teeth of a lower jaw prosthesis are set up - from the chewing surface - against a dome-shaped arched template and form a transversal compensation curve. In this way, a bilateral “balanced” occlusion is achieved later in function (when chewing). The curvature of the calotte depends on the inclination of the cusp of the denture teeth and the inclination of the condylar path. The inclination of the condylar path is the inclination of the articulated path against the Camper plane or the Frankfurt horizontal ( see below ). The application of the Wilson curve has its origin in the space-filling theory of George S. Monson (1920). Then the tooth axes of all upper jaw teeth meet at a common point, which is in the area of the cock's crest ( Latin crista galli ) of the ethmoid ( Latin os ethmoidale ). The chewing surfaces lie on the curved surface of a segment of a sphere with a diameter of 28.8 cm.
Breakdown of the alveolar bone

The breakdown of the alveolar bone in the first year after tooth loss is about 0.5 mm in the upper jaw and 1.2 mm in the lower jaw. In the following years the reduction is 0.1 mm in the upper jaw and 0.4 mm in the lower jaw, each year. The faster breakdown of the lower jaw bone results, among other things, from the fact that the contact surface for a prosthesis is only about half the size of that of the upper jaw. In the upper jaw, the prosthesis also rests on the palate . As a result, the loading forces that act on the lower jaw are twice as great as in the upper jaw . As a result, after around 20 years of wearing the prosthesis, the alveolar ridge of the lower jaw is completely broken down and the lower jaw has become flat. It then no longer offers a hold for a full denture. In such cases, the jaw can be reconstructed using various surgical jawbone augmentation procedures. The prosthesis can also be held in place with implants . In order for the jaw resection to take place as slowly as possible, the prosthesis must lie firmly on it. This must be done by regularly relining (“padding”) the prosthesis every one to two years . A new product should be made after about five years, as the plastic becomes brittle over time and the risk of breakage of the prosthesis increases when chewed.
In the so-called normal bite , the buccal (outer) cusps of the upper posterior teeth are further out than the buccal cusps of the lower posterior teeth. In severely atrophied jaws, the toothless mandibular arch is usually larger than the maxillary dental arch. The alveolar ridge arches often cross in the area of the second premolars, which results in the teeth being set up in the crossbite . Here the buccal cusps of the mandibular posterior teeth bite laterally past the buccal cusps of the upper posterior teeth. The outer limiting structures for setting up the posterior teeth are the zygomaticoalveolar crest (zygomatic alveolar ridge) in the upper jaw and the mandibular oblique line (oblique lower jaw line) in the lower jaw.
Pre-prosthetic surgery
The pre-prosthetic surgery is used to improve the denture. The vestibuloplasty in the upper jaw is a surgical procedure to deepen the oral vestibule . This indirectly increases the alveolar ridge and improves the hold of the prosthesis. A distinction is made between open vestibuloplasty, in which the tissue is detached via a circular incision of the mucous membrane and sewn on again cranially (above), from the closed method according to Hugo Obwegeser , in which the mucous membrane is tunnelled and the soft tissue and muscles below are shifted cranially . The floor of the mouth can be deepened, particularly in the rear area, which results in a retromolar lowering of the floor of the mouth. Here, the mucous membrane of the floor of the mouth and the insertion of the mylohyoid muscle (mandibular hyoid bone muscle ) are shifted caudally (below) with the lowering of the floor of the mouth according to Richard Trauner , Edlan and Mejchar or Martin Waßmund . Both fibroids (Gewebshyperplasien) and deep inserierende lip and cheek tapes should be removed as they might otherwise be bypassed only by recessing the prosthesis edge. This would eliminate the need for a prosthesis edge that seals well on all sides. By excision of the bands, the prostheses edition is enlarged and improved their fit and support.
Dental preparations
For the production of a full denture, a plaster of paris model of a jaw is made by means of an impression with a ready-made impression tray using mainly alginate , on which a patient-specific plastic impression tray is made. This already largely resembles the final denture base, the "plate" that rests on the jaw.
Mucodynamic impression
The dentist takes a functional impression with the individual impression tray . With the help of the dentist, while the impression material is setting, the patient performs all movements that should later be possible with the prosthesis, such as pointed mouth, opening mouth, sucking, laughing, extending tongue to the left and right, making faces and the like.
The soft tissues in the mouth can loosen or pry off the prosthesis with various mouth and tongue movements. The prosthesis must therefore allow the various muscle ligaments a range of motion, such as the frenulum of the tongue or the frenulum and cheek frenulum. In the lower jaw, the functional impression also takes into account the freedom of movement of the floor of the mouth , as the floor of the mouth rises and falls in conjunction with the tongue. The prosthesis must not be lifted off the lower jaw and levered out. The edge of the prosthesis must at the same time largely seal the prosthesis, which is the objective of the mucodynamic impression . A distinction is made between the outer and inner valve edge of the prosthesis. The inner edge of the valve is located between the mucosa (mucous membrane) of the alveolar ridge and the inner edge of the prosthesis base. The outer edge of the valve is located between the outer edge of the prosthesis and the lining of the cheek. In the upper jaw, a distal (rear) final edge of the prosthesis is created at the transition from the soft to the hard palate (by erasing the so-called A-line on the plaster model). The A-line is named after the fact that when the sound "A" is pronounced, the soft palate moves downwards and thus becomes visible to the practitioner. The edge can then be marked with a pen and is shown on the impression material. This allows the dental technician to recognize the A-line after the plaster model of the upper jaw has been produced. With a special impression material (FITT Functional Impression Tissue Toner ), a long-term functional impression is possible in difficult jaw conditions. The material can be worn for several days both to aid in the repair of injured tissue and to take an impression during daily use.
Jaw relation determination
After the functional impression, the dental technician creates the working model as the basis for the further work steps. This is followed by the production of registration templates (formerly: bite templates), with the help of which the dentist determines the jaw relation, determines the occlusal plane (masticatory plane) and draws the center line and the position of the canines . There are numerous methods for determining the jaw relation, e.g. B. the support pin registration . For this purpose, the movements of the lower jaw are recorded by means of an auxiliary construction in the patient's mouth. The so-called habitual occlusion lies at the intersection of the movement lines . This is the position of the lower jaw that the patient assumes in the usual way (normal bite position). The alignment of wax walls on bite templates is another method for determining jaw relation. By applying or reducing the wax walls, the patient can bite to different heights. When the jaw is in a relaxed position, the bite distance is determined. The ideal distance between the jaws for clenched (replaced) teeth is about two millimeters less. Overall, however, no clear recommendation for the choice of one of the methods can be given. The drawing of the so-called smile line in the wax walls enables the dental technician to recognize the area that is visible when laughing, because the denture plastic should not be visible when laughing, only the teeth. If this cannot be avoided, there are resins available in various red tones for the gingiva. The dental technician can set up the teeth accordingly. The denture teeth should also be placed in the middle of the alveolar ridge, since the denture could also be levered out by an eccentric arrangement.
Aesthetic aspects
Various factors contribute to the impression of the age of a toothless. These include the loss of lip support with the development of an enlarged angle between the nose and the upper lip, the development of deepened nasolabial folds and vertical folds in the mouth area, the reduction of red lips , the loss of lower face height , the development of pseudoprogenia (protrusion of the lower jaw) and a pronounced crease under the chin (submental fold). Setting up the front teeth includes the correction of the disturbed physiognomy and is intended to reconstruct the patient's profile . The determination of the jaw relation in toothless patients is particularly difficult because the loss of all teeth or all teeth in a jaw means that the three-dimensional relationship between the upper and lower jaw, secured by the occlusion, no longer exists. It is usually done by determining the closest speaking distance, the rest floating position . Alternatively, the Hromatka swallow bite position is used. Furthermore, the color and the shape of the artificial teeth are selected. Characteristics from the time of the natural dentition should be reconstructed to some extent, for example slight positional deviations or color nuances of the teeth. The subtleties of the aesthetic reconstruction of the dentition are aimed at preventing outsiders from recognizing that the person is wearing a prosthesis. The younger the person wearing the prosthesis, the more shameful it is to wear a prosthesis. A prosthesis should therefore give the impression of natural teeth.
Denture teeth are made of plastic or ceramic. Teeth made from ceramic materials show less wear and tear and greater color stability. Ceramic denture teeth are harder than plastic teeth, so the clenching of the teeth is more audible ("teeth chattering"). In return, plastic teeth can be fine-tuned in the chewing pattern due to slight abrasion. The disadvantage is that plastic teeth wear out more quickly.
Tooth shape and size
The patient's stature is reflected in the tooth shape, based on Kretschmer's constitutional types . A leptosomer often has very slender, long teeth, the pycnic rather short, stocky and the athlete has trapezoidal teeth.
If there are no models or photos of the original, natural teeth, the denture teeth are determined according to these constitution types. The tooth shape and position of close relatives can also be used as an aid. According to the embryo-genetic principle specified by Albert Gerber for full dentures, a person with a narrow nasal root and a wide nose base has a side incisor that is narrower than the central incisors . The one with a narrow root and base of the nose has both narrow central and lateral incisors, and the one with a wide root and base of the nose has both wide central and lateral incisors. The width of the teeth and thus their size can be determined from the distance between the outer nasal alar boundary ("canine lines"). The distance gives the total tooth width of the top six front teeth. Numerous scientists have developed various concepts for this. Teeth wear out with increasing age ( abrasion dentium ). This can be imitated by grinding the teeth according to their age. Laypeople are often mistaken that the tooth edges of the front teeth meet. In natural dentition, however, the upper jaw teeth stand in front of the lower front teeth (overbite) and only enable the shearing movement that is necessary for biting. The tooth edges are not straight, but rounded. The lateral incisors of the upper jaw are shorter than the central incisors. Only in the case of a progeny (protrusion of the lower jaw) are the tooth edges placed on top of one another ("head bite position"). The color, shape and position of the teeth should produce a natural appearance as much as possible.
Mold board of a street dentist in Bangalore
Tooth shade determination
By determining the tooth color of prefabricated prosthetic teeth (industrially manufactured), the color is determined to match the skin type and age, but can be individualized by the dental technician, i.e. both the shape can be individually changed by grinding and the tooth color by painting. The color of the vestibular (lip-side) denture plastic in the anterior region is adapted to age, skin color and constitution type. The leptosome type has clearly pronounced Jugae alveolariae (protrusions of the bony tooth sockets), while the athlete tends to have tight gums without any scarring. In older patients, a slight receding of the gums should be imitated. Otherwise, pure white teeth in an "ideal" configuration (often expressed by patients' wishes) would immediately indicate that they are wearing a prosthesis. With an artificial tooth, nature is imitated, because a tooth consists of numerous shades of color. The lighter the tooth color is selected, the less the color nuances differ and the tooth looks artificial. The impression of the degree of brightness of the teeth depends not only on the actual color of the teeth, but also essentially on the contrast with the color of the lips and the skin of the face. In dark-skinned or sun-tanned people (even when using a darker lipstick ), teeth therefore appear lighter than in light-skinned people.
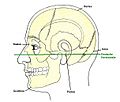
Transfer sheet
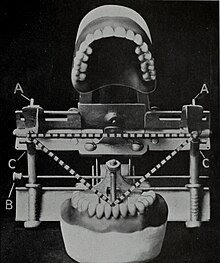
With the help of a transfer arch , the temporomandibular joint-related assembly of the working models in the articulator (a chewing simulator) is made possible. Without creating a face bow, the plaster models have to be mounted according to mean values in an average value articulator. These articulators are based on the mean of the Bonwill triangle . This is formed by the contact point of the lower central incisors and the center of the condyles (temporomandibular joint heads of the lower jaw). This triangle forms the Balkwill angle to the occlusal plane , which on average is between 20 ° and 25 °. With the help of the face bow, this angle and the Bonwill triangle can be customized. The plaster model of the upper jaw can be mounted in the articulator based on the skull. Depending on the articulator system, the face bow is positioned on the patient either on the Frankfurt horizontal or the Camper's plane . The Frankfurt horizontal runs through the lower edge of the orbit (eye socket) and the upper edge of the two Pori acustici externi (outer bony ear opening). The Camperian plane runs through the anterior nasal spine (lower spine on the anterior bony nostril) and the upper edge of the external acoustic porus on both sides. The Camper plane runs approximately parallel to the occlusal plane. The individualization of the articulator should have an advantageous effect on the creation of the static occlusion (final bite), which means that less subsequent corrections of the masticatory relief by grinding in are necessary.
Try-in
After the teeth have been set up in wax on a prosthesis base modeled from wax or made of plastic by the dental technician , a try-in of the dental work takes place . There are various doctrines for the treatment process as well as for the setting up of the denture teeth, for example setting up according to Gysi , according to Gerber , according to Lerch , according to the APF method (aesthetics, phonetics, function), according to the TiF method (total dentures in function), the AIl-OraI method, the Gutowski or Reusch methods . Usually 14 teeth are replaced per jaw. Wisdom teeth are not replaced. According to some doctrines, the replacement of 12 teeth is sufficient. The two second molars (and the wisdom teeth) are not replaced. During the try-in, the determination of the jaw relation and the appearance of the prosthesis can be assessed by the dentist and patient and corrected if necessary. Often only a compromise is possible between the requirements for aesthetics, phonetics and function, depending on the anatomical starting point.
Dental completion
The dental technician embeds the wax model with the denture teeth in a flask and pours it out with a special plaster of paris. After the plaster of paris has hardened, the wax is melted with hot water, whereby the teeth remain in the flask and a negative shape results. Various methods are used to insert the plastic into the negative mold and to harden it. After the plastic has hardened and the prosthesis has been devested, any excess on the prosthesis is ground away and the prosthetic plastic is polished to a high gloss with brushes and polishing pastes .
Metal base
Instead of plastic, the prosthetic base of an upper jaw prosthesis can be made of a chrome-cobalt-molybdenum alloy . Only the palate is covered by the plate called the “steel base”, where the metal is normally not visible. A full denture does not have to be relined in this area, which is not subject to bone resorption. The metal base does not extend to the A-line, but ends just before it. In the area of the A-line, the end edge is made of plastic at retentive areas because plastic can be more easily corrected and, above all, relined. Such a steel base is used when the shape of the jaw (for example high, pointed palate, pronounced exostoses) would result in an increased risk of the prosthesis breaking. A steel base can also increase the wearing comfort because it can be made much thinner (approx. 0.5 mm) than a plastic base due to its greater stability. This gives the tongue more space. A plastic denture base must have a thicker material (approx. 3 mm) so that it does not break when the chewing forces act on it. A metal base is expensive when it is cast from dental gold. No steel base is used in the lower jaw because it could not be relined for material reasons.
CAD / CAM
Using a new process, full dentures can be manufactured using the CAD / CAM process, the digital workflow only starting after the functional models have been produced and these have been introduced into the articulator in a known manner. The situation is recorded with an optical 3-D scanner . In digitally controlled manufacturing processes, additive processes ( selective laser sintering , stereolithography , 3D printing ) contrast with subtractive processes (milling, grinding). This is followed by the automatic digital setup of the denture teeth. The software suggests suitable tooth sets based on the model analysis. After the automatic basal adjustment of the denture teeth to the alveolar ridge, the software suggests the gingival design. The milling data for the upper and lower jaw bases including the tooth sockets are sent to a milling machine, which is milled from a gum-colored wax blank with water cooling. The denture teeth are adjusted using a further data set. The teeth are manually fixed in the tooth sockets with wax. The prosthesis is completed in the classic way. In another process, the prosthesis base is milled from a highly cross-linked, industrially manufactured, pore-free PMMA blank. A polymerization with distortion of the plastic base completely eliminated. This achieves a high degree of accuracy of fit of the plastic base.
Incorporation of the prosthesis
After the prosthesis has been completed in the dental laboratory, it is used on the patient and its function is checked. In most cases, the denture teeth have to be ground in until all teeth have even contact with the antagonists . Any existing canine or front tooth guidance is removed by grinding. To do this, the dentist uses an articulation film , an 8 µm to 40 µm thin ribbon of color that is held between the teeth of the upper and lower jaw. With articulation foils in different colors, the chewing patterns during the closing and chewing movements are reproduced on the occlusal surfaces. Interfering contacts and slideways can be sanded away at the colored areas in order to create a balanced dynamic occlusion (formerly: articulation). The molars should slide evenly over each other on both sides.
If it can be seen that extensive grinding measures are necessary, a so-called reassembly is carried out. A new jaw relation determination is carried out with the prostheses and the prostheses are sent back to the dental laboratory to make the corrections in the articulator. Only then are the fine corrections made in the patient's mouth.
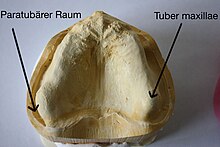
Aftercare
The treatment does not end with the insertion of the prosthesis. Material and manufacturing-related inaccuracies in the prosthesis can lead to pressure points, inflamed and painful areas in the area of the prosthesis contact surface. The prosthesis sits on the plaster model under a certain tension. If the tension subsides after removing the prosthesis, there will be deviations in the occlusion. Due to the absorption of water during the first 14 days of wearing the prosthesis plastic swells and changes the contact surface of the prosthesis base. Unavoidable inaccuracies in the determination of the jaw relation and the functional impression create a need for correction. The mucous membrane has a variable thickness, so that the load on the jawbone is uneven. Sharp edges of the jawbone under the mucous membrane can also cause pain when pressed. The resulting pressure points are removed by placing the denture base slightly hollow in the affected areas. This is done by grinding away the plastic in the area of the pressure points with a plastic cutter. Predilection sites are the maxillary tuberosity in the upper jaw and the mylohyoid crest in the lower jaw. In difficult cases, is remounting the prosthesis performed in the articulator when extensive corrections of articulation are necessary. For this purpose, bite registrations in the centric, protrusion and laterotrusion are recorded with the prostheses in order to be able to imitate the individual chewing patterns in the articulator.
Bruises
If a prosthesis causes pressure points and hurts when chewing, then understandably the prosthesis is not pressed firmly onto the jaw, which means that the prosthesis cannot suck in properly and thus cannot hold. Pressure points must therefore be removed by a dentist immediately. If the alveolar ridge bone is angular, a lining that remains soft can dampen the stresses of chewing and thus prevent pressure points. Plasticizers are added to the plastic . In cases that cannot be controlled, the jawbone must be surgically smoothed. If the mucous membrane does not lie tightly on the jawbone and wrinkles form, pressure points are created by squeezing these mucous membrane folds. In this case, either the excess gingiva must be surgically removed or the prosthesis placed hollow in this area. In addition, pressure points lead to mucosal ulcers , which can become infected and, in the worst case, degenerate. The healing of the pressure points can be accelerated by using adhesives .
It is not uncommon for several treatments to be necessary as part of the follow-up care in order to remove all pressure points, because after every change to the prosthesis base, the distribution of stress on the jaw changes, which can lead to new pressure points.
Prosthetic intolerance
A distinction is made between iatrogenic, somatogenic and psychogenic prosthesis intolerance and psychogenic prosthesis tolerance.
Iatrogenic prosthesis intolerance
Iatrogenic prosthesis incompatibility is the term used to describe errors in the manufacture and incorporation of the denture, including locally irritating factors.
Somatogenic prosthesis intolerance
The causes of a somatogenic prosthesis intolerance lie in the patient's organic area. These include in particular allergies , gastritis , metabolic diseases , xerostomia , tongue hypertrophy, parafunctions or dyskinesias .
Psychogenic prosthesis intolerance
A psychogenic prosthesis intolerance is present if the patient brings up complaints that cannot be objectified. Some patients associate their aging process with prostheses and ultimately refuse to adapt the prosthesis. There is also a feeling of shame. They often complain of nausea , disgust , difficulty swallowing, burning mouth, lips or tongue and inexplicable pain sensations. This also includes patients with the luminary killer syndrome , who usually show up with a bag full of prostheses and complain to the new practitioner of their years of suffering as a prosthesis wearer. The doctor-patient relationship is characterized by an initial idealization of the doctor, which soon turns into rejection because of his limited ability. The patient can only tolerate brief contacts with the doctor. Narcissistic traits and the persistence of an external ideal object stand out in the personality . The therapy of the syndrome or the psychosomatic illness consists of psychotherapy , which must precede the manufacture of new prostheses.
Psychogenic prosthesis compatibility
A special form is the psychogenic prosthesis compatibility, a disease in which patients dentally unacceptable dentures due to psychological features such as dementia , oligophrenia , alcoholism , Alzheimer's disease , for years tolerated and even accept to vollster satisfaction. This leads to considerable damage to the orofacial system. These include pressure points with ulcerations , temporomandibular joint damage, palate perforations and even tumor diseases .
Impairments
Wearing a prosthesis is associated with limitations and impairments. Sometimes the desire of patients after extraction uttered all teeth, in the belief that that all dental problems are eliminated. Apart from the fact that the extraction of teeth without medical indication - also at the request and thus with the consent of the patient (which is ineffective) - constitutes a criminally relevant bodily harm according to § 223 StGB and entails claims for damages and compensation for pain and suffering , "problems" sometimes arise replaces other impairments.
Ingestion
The bite force is mainly of the four muscle masseter (masseter muscle), temporal muscle (temporal muscle), medial pterygoid muscle (inner wing muscle) and lateral pterygoid muscle (outer wing muscle) exerted. The first three muscles mentioned are the elevators, i.e. those muscles that lift the lower jaw and cause the clenching. The latter is a guide muscle (for the advancement movement of the lower jaw). The maximum bite force between the molars of a full denture wearer (118 N ≈ 12 kp ) is considerably reduced compared to a fully dentate patient (1470 N ≈ 150 kp). This also reduces the chewing efficiency for prosthesis wearers. Chopping up the food takes four to five times as long as it does with fully-toothed people.
Biting off is only possible to a limited extent with a full denture. The prerequisite is that the maxillary tuberosity is pronounced and the prosthesis extends into the paratubar space and encompasses the tuberosity, otherwise the maxillary prosthesis will be pried off. If the maxillary tuberosity is only one-sided, it can be bitten off with the contralateral side if necessary. Otherwise the food has to be chopped up instead of bitten off.
Thin dishes such as lettuce leaves can only be chopped up if the cusps and dimples of the upper and lower teeth can work with the mortar and pestle principle. The so-called slide articulation (glide bite) is a complete wear and tear of the tooth cusps of the dentition. If the chewing surfaces are ground flat or chewed, these foods can no longer be chopped up.
The consumption of sticky food ( e.g. caramel candy , chewing gum ) should be avoided, as this can cause the prostheses to stick and loosen.
One-sided chewing should be avoided, that is, the food should be evenly distributed on both sides while chewing. One-sided chewing increases the risk of the prosthesis being pried out.
If the prostheses are levered out during grinding movements, the prosthesis wearer may have to change their chewing habits and carry out a chewing pattern that is more like chopping movements. In this case, grinding movements of the jaws should be reduced.
Sense of taste
Taste buds are mainly located in the tongue , but also in the palatal mucosa . By covering the palate with a full denture, gustatory perception (taste sensation) is impaired ( hypogeusia ). This also includes the reduced perception of temperature and the reduction of the sensory perception of the food bolus . The "culinary delights" are noticeably reduced. Furthermore, the now covered folds of the palate ( Latin: Plicae palatinae transversales ) can no longer be used to rub the aromatic substances of the food into the taste buds of the tongue. The latter can be countered - to a limited extent - by incorporating artificial palatal folds into the prosthesis.
salivation
Because of the unfamiliar foreign body in the mouth, excessive saliva is initially produced, which normalizes in the course of the process of getting used to the prosthesis. If the saliva is very thin, the viscosity can be increased using adhesive powder .
Elderly patients and those who have had head and neck radiation therapy or chemotherapy often complain of dry mouth . In pathological lack of saliva, there are saliva substitutes (gel, carmellose Spray, oil, mucin Spray).
Sound formation
Missing palatal folds can lead to lisp . A prosthetic base that is too thick and smooth can disrupt sound formation (articulatory phonetics). The pronunciation must be practiced by a newbie to the prosthesis by reading aloud alone.
Chattering teeth
An audible chattering of teeth can result from the use of porcelain teeth. It is therefore preferred to use plastic teeth. Chattering of teeth can also result from incorrect determination of the bite height (resting position). The teeth of the upper and lower jaw are too close to one another and touch each other when speaking, which leads to the annoying noise. At the same time, too great a bite height makes it difficult to close the lips.
Tooth color
Dental materials are not able to make the tooth color of artificial teeth appear natural and identical in all lighting conditions. Direct sunlight, headlights, artificial lighting or different degrees of brightness during the day and at night produce different color impressions of the tooth color. The luminescent effect can make artificial teeth shine undesirably under disco lighting ( black light), for example . The UV rays contained in daylight stimulate red and yellow as well as fluorescent green, with the result that green and red complement each other as complementary colors to white, and this with yellow results in the yellowish appearance of the tooth in daylight. In contrast, there are no UV rays in artificial light , which means that only yellow and red are reflected and the tooth appears reddish.
Gag reflex
A gag stimulus can be caused by an upper jaw prosthesis that is “too long” if the end edge comes to lie in the area of the so-called soft palate , thus crossing the A-line.
Prosthetic stomatitis
In the case of denture wearers, poor denture care (plaque and / or adhesive cream residue on the denture) can trigger stomatitis . The oral mucosa is inflammatory, including the classic signs of inflammation of redness ( Latin rubor ), overheating ( Latin calor ), swelling ( Latin tumor ), pain ( Latin dolor ) and restricted function ( Latin functio laesa ). The fungus Candida albicans is particularly often the trigger, but staphylococci , streptococci , enterobacteria or Neisseria can also be involved.
Numbness
In the lower jaw, due to the breakdown of the alveolar bone, the pressure of the prosthesis on the mental nerve (chin nerve), which emerges from the mental foramen (chin hole), can lead to a feeling of numbness in the lower lip. In this case, the prosthesis must be placed hollow in this area. Alternatively, the mental nerve can be relocated caudally (below) by means of a surgical nerve displacement.
Torus palatineus
The torus palatinus , an exostosis (bony bulge) in the middle of the so-called hard palate, can make it more difficult to hold a full denture in the upper jaw, as the surrounding mucous membrane is flexible, but the torus palatinus is not. Therefore, the prosthesis can rock right and left over the torus. This can be remedied by “relieving” the torus. For this purpose, a tin foil about 1 to 2 mm thick is placed on the plaster model over the area of the torus as a placeholder during the manufacture of the prosthesis , whereby the torus will be hollow in the finished prosthesis. This hollowing can also - to a limited extent - take place subsequently by grinding out this prosthesis area. When the chewing pressure is exerted, the surrounding mucous membrane gives way before the prosthesis comes into contact with the torus. The incidence (frequency) of the torus palatinus and torus mandibularis (in the lower jaw) in the population is given as about 30%.
Tongue enlargement
If there is toothlessness over a long period of time that has not been treated by dentures, the tongue enlarges in the sense of muscular hypertrophy ( macroglossia ). In this case, the incorporation of full dentures is felt to be very tight for the tongue. It takes longer to get used to a prosthesis, a period in which the tongue also shrinks a little.
Angular rhinitis
Should it by breaking the alveolar bone and / or wear of the artificial teeth or by coming from the outset to low occlusal height to bite reduction can angular cheilitis ( Latin angular cheilitis ) arise, poorly healing inflammatory changes in the mouth caused by tears ( fissures ) and superficial tissue defects ( erosions ) are characterized. In this case it is necessary to raise the bite, if necessary by making a new prosthesis.
Schlotterkamm
One of the mechanically induced changes in the mucous membrane is the " ridge ", which is caused by permanent mechanical stimuli. In the case of the Schlotterkamm, the alveolar process in the oral cavity appears to be well preserved. Under the mucous membrane, however, the bony alveolar process is replaced by connective tissue, so that the alveolar ridge is mobile and "shakes". A typical situation is the Schlotterkamm in the front of the upper jaw due to long years of wearing a full upper denture with unrestored, anterior (front) residual dentition in the lower jaw. The result is that the upper jaw prosthesis is not in a stable position because it moves along with the ridge of ridge below.
Broken prosthesis
If the prosthesis is hollow because it has not been relined for a long time or the plastic has become brittle or the prosthesis slipped during cleaning, the prosthesis can break. A broken prosthesis can usually be repaired within a day. The prerequisite is that no amateur repair attempt has been carried out, because in this case the fragments can no longer be precisely repositioned. This would make the prosthesis unusable.
Weight loss
When you lose weight, the soft tissues of the face change significantly. The interaction between muscles and ligaments makes a significant contribution to the retention of the prosthesis. In the event of weight loss, the prosthesis must therefore be adapted to the new circumstances.
Bite injuries
During the acclimatization phase, bite injuries can occur in the cheek or tongue because the mouth muscles first have to get used to the new prosthesis. The chewing of the food should therefore be practiced at the beginning by “chopping up” the food with soft foods ( mashed potatoes , porridge ). After a bite injury, the gums swell, which increases the risk of another bite injury. In the course of a few weeks, the new chewing patterns pass into the subconscious.
Pipe smoker
With full dentures in the upper and lower jaw, pipe smokers can only hold the pipe between their teeth with great difficulty , as the lower denture in particular tends to tip over much more easily. The lightest possible (20 g), short, curved pipe ("podge") with a flat, but wider bite ("fishtail" mouthpiece) made of the softer natural rubber ( ebonite ) should be preferred. Acrylic mouthpieces are difficult to hold between the teeth, also depending on the pipe weight. It is possible to grind the teeth in such a way that a pipe fits between the teeth when the rows of teeth are closed (" pipe holes "), but without a pipe unsightly gaps between the upper and lower teeth in the area of the pipe inlet remain visible.
Holding a pipe between your teeth increases the flow of saliva, which also shortens the time it takes to hold the prosthesis.
Diver
Divers should use an orthopedic mouthpiece (JAX), which the dentist adjusts or produces individually to the dentition if possible. Alternatively, you can dive with a full face mask . When snorkeling , an upper full denture should be fixed to the palate with a very tough adhesive cream, even if no adhesive cream is used in everyday life. A lower full denture is omitted, instead a mouthpiece made individually by the dentist is used on the snorkel, which is firmly connected to the snorkel. Both when diving and snorkeling there is a risk of losing the prosthesis when removing the mouthpiece. Their specific weight is greater than that of water. Even when swimming there is a risk of the prostheses being washed out.
Special forms
In addition to the classic full denture, there are various special forms.
Immediate prosthesis
A special form is the immediate prosthesis (immediate prosthesis). If a row extraction is necessary, a prosthesis is prepared in advance of the extractions , which is inserted immediately after the extraction of the teeth, so that the patient does not leave the practice toothless. For this purpose, an impression of the dentition that is still toothed is made. The teeth are ground away on the plaster model and a full denture is made on it. Such a prosthesis is corrected after a few weeks, e.g. B. by relining, because the jaw changes and is broken down significantly as the extraction wounds heal. A side effect of immediate care is that such a prosthesis also serves as a dressing plate for the numerous extraction wounds.
Interim prosthesis
A transitional prosthesis is called an interim prosthesis. This is made if a full or immediate prosthesis cannot be made immediately due to difficult anatomical conditions. An interim prosthesis can bridge the period up to the completion of a full prosthesis, which can take several weeks to months.
Second prosthesis
In order to prevent even temporary toothlessness, a second prosthesis (also: travel prosthesis, replacement prosthesis, duplicate prosthesis) can be made, because if a prosthesis is lost, a new one needs several weeks, which can be bridged with a second prosthesis. In the event of a repair that has become necessary, for example a broken prosthesis, the continuous supply of a prosthesis is also guaranteed. Full dentures are duplicated in the dental laboratory: The finished original denture is molded and a second copy is made on the basis of this hollow form. An interim prosthesis can also be expanded into a second prosthesis.
Religious reasons
The Jewish dietary laws ( Hebrew כַּשְרוּת Kaschrut , 3rd Book of Moses (chap. 11)) write, among other things, the temporal separation of enjoyment from “fleshy” ( Hebrew בשרי basari ) and "milky" ( Hebrew חלבי Chalawi ) dishes (Deut. 14, 21b). Meat and dairy products may not be eaten together, but only with the prescribed time interval. The strict separation goes so far that different dishes are used for meat and dairy dishes. Orthodox Jews sometimes have two pairs of prostheses made in order to be able to use a separate prosthesis for each of the two types of food. Most rabbinical authorities , however, take the view that this is not necessary.
Wind musician
Wind musicians need a special prosthesis, which is made depending on the instrument and thus depending on the type of sound generation and shape of the mouthpiece and which stabilizes the prosthesis while playing. Additional anchoring with implants is definitely preferable to full dentures. If this is not possible, a bite ridge is made in the molar area for stabilization, for example, without teeth in the molar area. The height of this corresponds approximately to the resting position, with a slight protrusion (undershot) of the lower jaw. The bite ridges can be interlocked by two or three so-called “inclined planes” and thus press the prosthesis in the direction of the alveolar ridge. Alternatively, elastic blowing aids can be made from plastic that remains soft. In this case, wind musicians need a second prosthesis in the sense of a "normal" full prosthesis for everyday use, as an eating and speaking prosthesis.
Cover Denture
As Cover Denture (also: overdenture ) refers to a dental prosthesis, in which even a few remaining teeth in the dentition are present, with telescopic crowns are provided or root caps. Implants (implanted artificial tooth roots) can also perform the same function . A full denture is slipped over these crowns. The teeth treated in this way ensure a better hold, especially in the sense of a transitional treatment if the remaining teeth also have to be extracted at a later point in time. In this case, they are used to make it easier to get used to a prosthesis.
Two implants in the lower jaw with patrixes for attaching a cover denture prosthesis
The matching lower jaw prosthesis with the integrated matrices
Defective prosthesis
With a defect prosthesis (also: resection prosthesis), in addition to the aforementioned replacement of teeth and the alveolar process of a full denture, parts of the jaw that have arisen as a result of a congenital malformation, an accident or a tumor operation are also replaced. A special form is the obturator (also: palate obturator), which is used to secure the function of sealing the oral cavity against the nasal cavity or maxillary sinus in the case of inoperable jaw defects. The full denture is expanded to include a plastic bead that takes on this function.
Denture cleaning
Due to their structure and surface structure, prostheses are prone to plaque adhesion and thus bacterial contamination . For cleaning a full denture, the trade has special denture brushes available. Liquid soap , dishwashing detergent, but also curd soap can serve as cleaning agents . Toothpastes containing abrasives should not be used as they roughen the denture resin, thereby promoting the accumulation of tartar and plaque . It should be cleaned over a wash basin filled with water so that the prosthesis does not break if it is dropped. Alternatively, a towel can be placed in the sink to cushion the impact of the prosthesis. In addition, the prosthesis should be rinsed off after every meal, because food residues that slide under the prosthesis, on the one hand, impair the hold of the prosthesis and, on the other hand , can lead to bad breath . Cleaning tablets should be used cautiously. The denture plastic is leached out with frequent use of cleaning tablets, the surface becomes rough and the plastic loses its color. With prolonged use, the elasticity of the prosthesis is impaired. Percarbonates , sodium hypochlorite , chlorhexidine digluconate , tensides and enzymes are used as active ingredients . The use of cold plasma for cleaning and disinfection is currently (2017) being researched. Cleaning tablets also do not replace mechanical cleaning.
Denture cleaning device
There are denture cleaning devices that work on the basis of ultrasound , and others that use magnetic polishing needles to clean the dentures. With ultrasound devices, the prostheses are placed in a water bath and the water is made to vibrate using ultrasound. This also creates tiny water bubbles, which also increase the cleaning power. Dentists and dental laboratories also have denture cleaning devices with polishing needles (eddy current devices). To do this, the prosthesis is placed in a water bath with cleaning additives. In addition, special polishing needles are placed in the water bath. The polishing needles contained in the water bath are set in vibrations, which clean the prosthesis of dirt.
Epidemiology

|
|
|
|
According to statistical Yearbook of the cash-dental Federal union 297,700 full dentures in the maxilla and 170,600 complete dentures in the lower jaw were at in 2015 in Germany insured patients remade. In addition, there are 420,400 newly manufactured cover denture prostheses in the upper and lower jaw (with a remaining number of teeth up to three teeth per jaw). This does not include around 10% of those with private insurance. Assuming that new prostheses are made every five to eight years, the absolute number of full denture wearers (plus cover denture) is correspondingly higher (estimated over 4 million affected people, which corresponds to around 5% of the population). According to the Fifth German Oral Health Study (DMS V), which was carried out from October 2013 to June 2014, every eighth out of the 65 to 74-year-old age group is toothless; in 1997 it was every fourth.
Around 158 million people worldwide are affected by complete toothlessness, which makes up 2.3% of the world population (as of 2010). With a share of 2.7%, women are more affected than men with 1.9%.
costs
Germany
In Germany there has been a fixed subsidy system for dentures in statutory health insurance since 2005. A full denture is a so-called standard care , for which a fixed allowance of 50% of the average costs is. Without confirmation of a regular annual visit to the dentist in a bonus booklet , the patient's own contribution for each upper and lower complete denture is around € 600–800. Depending on the frequency of visits to the dentist in the last 5 or 10 years, the co-payment is reduced to 40 or 35% ( Section 55 (1) SGB V ).
Austria
In Austria, for example, the cost of a full denture per jaw for those insured with the Salzburg Regional Health Insurance Fund is € 852.
Switzerland
In Switzerland, the costs of a full denture range from CHF 3200 to CHF 3800 .
history

It is known from the early 16th century that full dentures were made of wood in Japan. This continued until Japan opened up to the West in the 19th century. Various attempts in the past to replace teeth with functional prostheses were ultimately unsuitable.
When George Washington became the first President of the United States in 1789, he was 57 years old and had only one tooth. Washington made do with a cosmetic prosthesis made from hippo teeth, ivory, and human teeth that John Greenwood had made. Formerly a carpenter and mechanic of nautical instruments in New York City , this had made a name for himself as a dentist . The prosthesis should be held in place by spiral springs. George Washington regularly left the room at a banquet in order to be able to eat undisturbed without prostheses, because he did not want to come out as a prosthesis wearer.
Waterloo teeth
Human teeth were stolen from crypts by corpse bats or taken from the executed and incorporated into dentures by dentists. In 1799 Francisco de Goya recorded a scene in the painting A caza de serves ( Spanish hunting for teeth ) in which a well-dressed woman breaks the teeth of a hanged man .
A large fund of human teeth for prostheses was the Battle of Waterloo (1815), in which several 10,000 soldiers were killed, including many young men with healthy teeth. The trade in these teeth, with which dentures were made, took on such proportions that they were later called Waterloo teeth ( English Waterloo teeth ). Waterloo teeth were already collected after the Battle of the Nations near Leipzig from October 16 to 19, 1813. There, where around 600,000 soldiers from several European countries faced each other, over 91,000 of them lost their lives. After the battle, the battlefields on the outskirts of Leipzig were ravaged by a band of looters trying to get hold of anything of value. “Worst of all were the Fledderers”, as a Leipzig city official is quoted, “who broke the jaws of the dead and tore out the most beautiful and whitest teeth in order to sell them for insertion. Sometimes they tore their teeth from those who were still dying ”.
The teeth of a hippopotamus were also carved onto the jaw as a prosthesis . Waterloo teeth were partially attached to the carved denture base made from teeth of a hippopotamus. Only wealthy circles in the Victorian era could afford both . Another “reservoir” for human teeth was the American Civil War (1861 to 1865). There, too, teeth were extracted from the fallen and sent en masse to London . These teeth were also called Waterloo teeth using the term that has now become established. The end of the bat is likely to have been due to the changed treatment of prisoners of war and fallen soldiers after the signing of the first Geneva Convention on August 22, 1864.
Porcelain teeth
In 1789, the Frenchman Nicolas Dubois de Chémant wanted to meet his desire for natural-looking dentures and applied for a patent for the porcelain teeth he had developed . They were called incorruptible ( French indestructible, imperishable ), in contrast to the foul-smelling bone dentures. Chémant took up the idea of the pharmacist Alexis Duchâteau (1714–1792), who in 1774 had experimented with the manufacture of porcelain teeth. The Italian dentist Giuseppangelo Fonzi (1768–1840) acquired this knowledge and achieved fame in 1815 for his successful production of porcelain teeth, which he firmly attached to the denture base with metal pins. The reputation of this incorruptible spread to the Bavarian royal court in Munich , to the Russian Tsar Alexander I and from there to the Spanish Bourbons . On March 9, 1822, Charles M. Graham of New York was granted a US patent for his invention of an improvement in the construction of artificial teeth.
vulcanization
In 1839, invented Charles Goodyear the vulcanization , a method wherein the rubber under the influence of time, temperature and pressure to atmospheric and chemical agents and to mechanical strain is made resistant. This soon resulted in the rubber prostheses according to Thomas W. Evans and Clark S. Putnam (1864), into which porcelain teeth could be built. The intimate connection of rubber and metal on a metal base proved to be difficult. During vulcanization, the sulfur excretion of the rubber formed a sulfide layer on the metal , which made it difficult for the two materials to adhere.
Around 1840 around 500,000 porcelain teeth were exported from Paris to the USA, which was accompanied by a rapid increase in the number of dentists and dental technicians. In 1844, Samuel Stockton White (S. S. White) began making porcelain teeth in the United States . According to a survey in the USA in 1940 about 70% of all dentures there were made from rubber. At the beginning of the 20th century, when the functional impression to generate the suction effect and thus hold a prosthesis was not yet invented, suction cups were built into upper jaw prostheses . However, over many years of use, these produced jaw defects and even perforations of the palate , whereupon this aid was abandoned.
plastic
The prosthesis plastic polymethyl methacrylate (PMMA) was developed around the same time in Germany, Great Britain and Spain in 1928. In Germany, the chemist Walter Bauer (1893–1968) was involved in this. In 1936, the Kulzer & Co. company introduced the chemoplastic processing method (Paladon method) developed by Bauer. It corresponds to the method that is widespread today to paste the polymer particles into a paste with monomer liquid and to introduce them plastically into hollow molds, where the plastic hardens under pressure. The plastic was so developed in the 1950s that it replaced rubber.
Impression and model material
After Edwin Thomas Truman had developed the gutta-percha , in 1856 the London dentist Charles T. Stent (1807–1885) added stearin in particular , which improved the plasticity of the material and its stability, talc as an inert filler to give the material more bulk, also resin and red dye, and the thermoplastic material named after him was created for molding the jaws (and teeth). Stent replaced beeswax and plaster of paris , which had been used up until then, as impression materials.
A special, easily breakable impression plaster was used for the plaster cast, which could be broken out of the mouth piece by piece after it had set. The fragments were then glued together and filled with hard plaster to produce the final model. Peppermint was added to the plaster of paris to "improve the taste" while taking the impression .
The British chemist and pharmacist Edward Curtis Stanford is considered to be the discoverer of alginate, which extracted alginic acid from brown algae in 1880 . In 1940 the salts of alginic acid, commonly known as alginates, were introduced into dentistry as an impression material. In addition to sodium alginate, it usually also contains calcium sulfate (gypsum), sodium phosphate as a retarder and a large proportion of kieselguhr (diatomaceous earth). With the reversible hydrocolloids , the first elastic impression materials were introduced in 1925 . At the beginning of the 1950s, the elastomeric impression materials were introduced, initially the elastomeric polysulphides (thiocoles) and the condensation-curing silicones , followed in 1965 by the polyethers (Impregum, 3M ESPE ) and in 1975 by the addition-curing silicones (vinyl polysiloxane).
Articulators
The development of the articulator , which, as a chewing simulator, should enable the movements of the lower jaw and thus the reproduction of the chewing pattern, began with an occludator that only allowed the opening and closing of the dentition to be imitated. In 1893 , Julius Parreidt describes in detail various methods common in the 19th century, initially using a door hinge to fix the two jaw models in exactly the same way as the jaws in the mouth relate to one another when biting. After preliminary work by Daniel Evans , William Gibson Arlington Bonwill (1833–1899) from Philadelphia developed the first above-average articulator in 1864, a device for simulating the movements of the temporomandibular joint. For this purpose, plaster models of the dental arches of the upper and lower jaw are mounted in occlusion in the articulator. The Gysi-Simplex articulator developed by the Swiss dentist Alfred Gysi (1865–1957) around 1910 was to prove to be a milestone. Due to the condylar guide surface in the lower part and the joint drum in the upper part, these types are referred to as so-called non-arcon articulators , as the movements take place in reverse to the anatomical-physiological process in the real joint. The Hanau articulator, which is based on the same principle, the Whip-Mix articulator or the Schul-Articulator-Munich (SAM) became better known. Over 100 different articulators have been developed over the past 150 years.
The search for a better hold
The historical prosthetic collection of the Center for Dentistry, Oral and Maxillofacial Medicine of the Martin Luther University Halle-Wittenberg shows numerous attempts from the past to improve the hold of a prosthesis. After the rubber suction cups, a Heintz compression ring was created by erasing the plaster model in the base of the upper jaw prosthesis. He was followed by the etching after Stadler. His 1–2 mm deep etchings were arranged on the roof of the mouth without crossing the palatine torus. These ran parallel to the palatine torus, dorsally parallel to the A-line. Modifications with the Frankfurt etching and the Walser etching followed. Etchings on the plaster model result in beads of 1–2 mm in size on the finished prosthesis, which should create small suction chambers in the palate area for a better hold. The construction with pads (gingival brackets) followed a different approach until first the mucostatic and later the mucodynamic impression significantly improved the hold of the prosthesis.
At the same time, attempts were made to improve the hold by shaping and positioning the prosthetic teeth. Mention should be made here of the tooth set-ups according to Strack, who modified them depending on the bite position, namely with type K for the head bite or the progeny , type D for the cover bite or distal bite and type S for the scissor bite. This was followed by the static-articular arrangement according to R. Fischer, according to Hiltebrandt and the spherical cap arrangement according to Fehr, followed by the arrangement according to Haller, until one returned to the classic arrangement according to Gysi. Another variant was the setup with furrowed molars.
Due to the inadequate possibilities of constructing the lower jaw total prosthesis in a stable manner, various aids were used. Attempts were made to weigh down the prosthesis with metal shavings, to use the repulsive force of a magnet each in the upper and lower jaw prosthesis, or to increase the absorbency with suction plates. Another consideration was bit feathers. You should use great force to press the lower replacement onto the jaw. This was followed by subperiosteal implants in the 1950s and 1960s, metal framework between jaw bone and periosteum were used (periosteum) under the mucous membrane of which post sticking out through the mucosa, where you could attach the prosthesis. The subperiosteal implants, however, were not biocompatible and caused inflammation.
The concept developed by Albert Gerber (1907–1990) was another milestone in improving the retention of the prosthesis, on which he had worked from 1948 to 1984 in the form of a life's work. This included the development of articulators (Condylator), from tooth shapes (Condyloform teeth) in 1958 to manufacturing that conforms to the temporomandibular joint.
outlook
Since the beginning of the 20th century, dozens of materials, tooth shapes, instruments and procedures have been developed for every treatment and work step in providing patients with full dentures. However, to date it has not been possible to achieve reproducible values and treatment results. The success of the treatment ultimately depends on the experience of the dentist who has gained experience with the procedure they prefer. The trend is increasingly towards implant-anchored dentures. Implants (implanted artificial tooth roots) can considerably improve the hold of the denture. The prerequisites are appropriate anatomical conditions and the financial framework. However, the described basic rules of treatment for the production of a full denture must be observed.
literature
- Klaus Fuhr, Thomas Reiber: The total denture. Urban & Schwarzenberg, Munich et al. 1993, ISBN 3-541-12071-1 .
- Horst Gründler, Ulrich Stüttgen: The total denture (= basic knowledge for dental technicians. Vol. 4). 3rd, revised edition. Neuer Merkur, Planegg 2014, ISBN 978-3-929360-84-4 .
- Lorenz Hupfauf (Ed.): Total prostheses (= practice of dentistry. Vol. 7). 2nd Edition. Urban & Schwarzenberg, Munich et al. 1987, ISBN 3-541-15270-2 .
- Bernd Koeck (Hrsg.): Total dentures (= practice of dentistry. Vol. 7). 4th edition. Urban & Schwarzenberg, Munich et al. 2005, ISBN 3-437-05360-4 .
Web links
- S3 guideline for implant prosthetic restoration of the edentulous upper jaw, Working Group of the Scientific Medical Societies , AWMF register number: 083-010, as of November 2014. Valid until November 2019. Online , accessed on April 10, 2017.
Individual evidence
- ^ Anne Wolowski: Psychosomatics. In: Bernd Koeck (Ed.): Total prostheses. 4th edition. 2005, pp. 15–34, here pp. 19–22, ( limited preview on Google Books ).
- ^ A b Jarg-Erich Hausamen, Henning Schliephake : Pre-prosthetic surgery. Change in the jawbone. In: Norbert Schwenzer, Michael Ehrenfeld (ed.): Dental surgery (= tooth-mouth-jaw-medicine. 3). 3rd, updated and expanded edition. Thieme, Stuttgart a. a. 2000, ISBN 3-13-116963-X , pp. 106-108, ( limited preview on Google Books ).
- ↑ Horst Gründler, Ulrich Stüttgen: The total denture (= basic knowledge for dental technicians. 4). 2nd, revised edition. Neuer Merkur, Munich 2005, ISBN 3-929360-84-5 , p. 134, ( limited preview on Google Books ).
- ↑ Klaus M. Lehmann, Elmar Hellwig, Hans-Jürgen Wenz: Dental Propaedeutics. Introduction to Dentistry. 12th, completely revised and expanded edition. Deutscher Zahnärzte-Verlag, Cologne 2012, ISBN 978-3-7691-3434-6 , p. 361, ( limited preview on Google Books ).
- ↑ Horst Gründler, Ulrich Stüttgen: The total denture (= basic knowledge for dental technicians. 4). 2nd, revised edition. Neuer Merkur, Munich 2005, ISBN 3-929360-84-5 , p. 151, ( limited preview on Google Books ).
- ↑ George H. Wilson: The Anatomy and Physics of the Temporomandibular Joint. In: The Journal of the National Dental Association. 7, 1920, p. 414, doi: 10.14219 / jada.archive.1920.0080 .
- ↑ Wolfgang Gühring, Joachim Barth: Anatomie. Special biology of the masticatory system (= basic knowledge for dental technicians. Vol. 3). 3rd, corrected edition. Neuer Merkur, Munich 1992, ISBN 3-921280-84-2 , p. 150, ( limited preview in Google Books ).
- ↑ Dieter Riediger: preprosthetic surgery. Anatomical consequences of tooth loss. In: Norbert Schwenzer, Michael Ehrenfeld (eds.): Dental surgery. 4th, completely revised and expanded edition. Thieme, Stuttgart a. a. 2009, ISBN 978-3-13-116964-8 , p. 199.
- ↑ Ralf Gutwald, Nils-C. Gellrich, Rainer Schmelzeisen: Introduction to dental surgery and implantology. For studies and work. 2nd, revised and expanded edition. Deutscher Zahnärzte-Verlag, Cologne 2010, ISBN 978-3-7691-3418-6 , pp. 439-446.
- ↑ Hermann Böttger, Horst Gründler: The dental and dental technology procedure for the telescope system in prosthetics. Telescopic crowns, bars, attachments, joints, bolts and the peripheral areas of the precision mechanical fastening devices. 3rd, unchanged edition. Neuer Merkur, Munich 1982, ISBN 3-921280-23-0 , pp. 77-79, ( limited preview on Google Books ).
- ^ Arnold Hohmann, Werner Hielscher: Dental technology in questions and answers. Questions about anatomy, prosthetics, orthodontics and materials science. 2nd Edition. Neuer Merkur, Munich 2003, ISBN 3-921280-93-1 , p. 240, ( limited preview on Google Books ).
- ^ Karl-Heinz Utz, Marc Schmitter, Wolfgang B. Freesmeyer, Thomas Morneburg, Alfons Hugger, Jens C. Türp, Peter Rammelsberg: Scientific report from the German Society for Prosthetic Dentistry and Biomaterials eV (formerly DGZPW): Determination of jaw relation. In: German Dental Journal. Vol. 65, No. 12, 2010, ISSN 0012-1029 , pp. 766-775, ( digitized version ).
- ↑ Antje Zorn: Comparison of different methods for determining the jaw relation using the IPR system. Dissertation, Medical Faculty Charité - Universitätsmedizin Berlin, 2015. Digitized . Retrieved January 28, 2017.
- ↑ A. Hromotka: The functional bite registration . In: German Dental Journal. Vol. 15, 1960, ISSN 0012-1029 pp. 769-776.
- ↑ Jürgen Setz, Eva Engel: The total denture. Clinical Guide. ( Memento of the original from August 24, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Ivoclar Vivadent, Ellwangen (Jagst) 2003, ISBN 3-00-022411-4 , p. 36.
- ^ Arnold Hohmann, Werner Hielscher: Dental technology in questions and answers. Questions about anatomy, prosthetics, orthodontics and materials science. 2nd Edition. Neuer Merkur, Munich 2003, ISBN 3-921280-93-1 , p. 257, ( limited preview on Google Books ).
- ↑ Jürgen Setz, Eva Engel: The total denture. Clinical Guide. ( Memento of the original from August 24, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Ivoclar Vivadent, Ellwangen (Jagst) 2003, ISBN 3-00-022411-4 , p. 40.
- ↑ Musa Dilmac: Studies on the selection of anterior sets using the BlueLine FormSelector TM in the context of full dentures. Gießen 2007, p. 9, (Gießen, Justus Liebig University, dissertation, 2007). Retrieved January 18, 2017.
- ↑ a b Horst Gründler, Ulrich Stüttgen: The total prosthesis (= basic knowledge for dental technicians. 4). 2nd, revised edition. Neuer Merkur, Munich 2005, ISBN 3-929360-84-5 , p. 129, ( limited preview on Google Books ).
- ↑ Thomas R. Morneburg, Alfons Hugger, Jens C. Türp, Marc Schmitter, Karl-Heinz Utz, Wolfgang Freesmeyer, Peter Rammelsberg: Scientific Communication of the German Society for Prosthetic Dentistry and Biomaterials e. V. (DGPRo) (formerly DGZPW): Use of the face bow in functionally healthy patients as part of restorative measures. In: German Dental Journal. Vol. 65, No. 11, 2010, pp. 690-694, ( digitized version ).
- ↑ Gerd Ude: Language and teeth. In: Quintessenz Zahntechnik. Vol. 37, No. 11, 2011, ISSN 0340-4641 , pp. 1438-1450. Retrieved December 10, 2016.
- ↑ Horst Gründler, Ulrich Stüttgen: The total denture (= basic knowledge for dental technicians. 4). 2nd, revised edition. Neuer Merkur, Munich 2005, ISBN 3-929360-84-5 , p. 207, ( limited preview on Google Books ).
- ↑ Complete dentures based on CAD / CAM. ZWP, March 11, 2015. Accessed December 4, 2016.
- ↑ Carlo P. Marinello, Alexander Deak: CAD-CAM application in full dentures. In: Swiss Dental Journal . Vol. 125, No. 6, 2015, pp. 713–720, ( digitized ).
- ↑ Wilm-Gert Esders: Rational workflows in the dental practice. Thieme, Stuttgart a. a. 2007, ISBN 978-3-13-132261-6 , pp. 163-164, ( limited preview on Google Books ).
- ↑ Reinhard Marxkors: Textbook of dental prosthetics. 4th, revised edition. Deutscher Zahnärzte-Verlag, Cologne 2007, ISBN 978-3-7691-3353-0 , pp. 176–178, ( limited preview on Google Books ).
- ↑ Wilm-Gert Esders: Rational workflows in the dental practice. Thieme, Stuttgart a. a. 2007, ISBN 978-3-13-132261-6 , pp. 163-164, ( limited preview on Google Books ).
- ↑ Barbara Elferich, Daniela Tittmann: Oral hygiene in the FOTT: therapeutic - structured - regular. Dentures and their care. In: Ricki Nusser-Müller-Busch (Hrsg.): The therapy of the Facio-Oralen Trakt. FOTT according to Kay Coombes (functional, complex, everyday related). Springer, Berlin a. a. 2004, ISBN 3-540-42318-4 , p. 104, ( limited preview on Google Books ).
- ^ Hans Sellmann: Prosthesis incompatibility. In: Hans Sellmann: The older, multimorbid patient in the dental practice. Volume 2: Geriatric dentistry in concrete terms. Spitta, Ballingen 2009, ISBN 978-3-938509-88-3 , pp. 88-90. Retrieved January 18, 2017.
- ^ Stephan Doering, Anne Wolowski: Scientific report of the working group on psychology and psychosomatics in the DGZMK on psychosomatics in dentistry, oral medicine and maxillofacial medicine. 2008. Retrieved January 18, 2017.
- ↑ Dieter Beck : The luminary killer syndrome. In: German Medical Weekly . Vol. 102, No. 9, 1977, pp. 303-307, doi: 10.1055 / s-0028-1104882 .
- ↑ Gerhard Kreyer: The psychosomatics of the orofacial system - a professional and ethical challenge. In: Dominik Groß (ed.): Ethics in dentistry (= between theory and practice. Vol. 3). Königshausen & Neumann, Würzburg 2002, ISBN 3-8260-2421-4 , pp. 87–97, here pp. 93–94, ( limited preview in Google Books ).
- ^ Christian Jäger: Exam revision course criminal law general part. 4th, revised edition. CF Müller, Heidelberg a. a. 2009, ISBN 978-3-8114-9723-8 , pp. 117-118, ( limited preview on Google Books ).
- ↑ Ammar Leyka: Changes in biting force after replacement or relining of total prostheses. Giessen 2001, pp. 8-22, (Giessen, Justus Liebig University, dissertation, 2002). Retrieved January 18, 2017.
- ↑ Bernd Lindemann: Receptors and transduction in taste. In: Nature . Vol. 413, No. 6852, 2001, pp. 219-225, PMID 11557991 , doi: 10.1038 / 35093032 .
- ↑ David V. Smith, John D. Boughter, Jr.: Neurochemistry of the Gustatory System. In: Abel Lajtha, Dianna A. Johnson (Eds.): Handbook of Neurochemistry and Molecular Neurobiology. Sensory Neurochemistry. 3rd edition. Springer, New York NY 2007, ISBN 978-0-387-30349-9 , pp. 109-135.
- ↑ Tuomas Waltimo, Susanne Christians, Jukka H. Meurmann, Andreas Filippi : Dental care for leukemia patients. In: Swiss monthly for dentistry. Vol. 115, No. 4, 2005, ISSN 0256-2855 , pp. 308-315, ( digitized version ).
- ^ Arnold Hohmann, Werner Hielscher: Dental technology in questions and answers. Questions about anatomy, prosthetics, orthodontics and materials science. 2nd Edition. Neuer Merkur, Munich 2003, ISBN 3-921280-93-1 , p. 246, ( limited preview on Google Books ).
- ↑ Klaus M. Lehmann, Elmar Hellwig, Hans-Jürgen Wenz: Dental Propaedeutics. Introduction to Dentistry. 11th, revised and expanded edition. Deutscher Zahnärzte-Verlag, Cologne 2009, ISBN 978-3-7691-3370-7 , p. 77, ( limited preview in the Google book search).
- ↑ André Hoffmann: Systematic research and analysis of tooth color and dental optical phenomena. New scientific knowledge and new methods for tooth shade creation, perception, measurement and determination. AtheneMedia, Dinslaken 2010, ISBN 978-3-86992-039-9 .
- Jump up ↑ P. Lewis White, David W. Williams, Tomoari Kuriyama, Shamim A. Samad, Michael AO Lewis, Rosemary A. Barnes: Detection of Candida in Concentrated Oral Rinse Cultures by Real-Time PCR. In: Journal of Clinical Microbiology. Vol. 42, No. 5, 2004, ISSN 0095-1137 , pp. 2101-2107, doi: 10.1128 / JCM.42.5.2101-2107.2004 .
- ↑ Lukasz Jablonowski, Rutger Matthes, Kathrin Duske, Thomas Kocher: Plasma applications in dentistry, oral medicine and maxillofacial medicine. Use of plasma for cleaning and disinfecting dental prostheses. In: Hans-Robert Metelmann, Thomas von Woedtke, Klaus-Dieter Weltmann (eds.): Plasma medicine. Cold plasma in medical applications. Springer, Berlin a. a. 2016, ISBN 978-3-662-52644-6 , pp. 127–130, ( limited preview on Google Books ).
- ↑ Bernd Quantius: The nerve shift in implantology. ZWP, October 29, 2010. Retrieved January 18, 2017.
- ↑ Hans H. Caesar: The training as a dental technician. Neuer Merkur, Munich 1996, ISBN 3-929360-01-2 , p. 90.
- ↑ Fernando V. Raldi, Rodrigo D. Nascimento, José R. Sá-Lima, Caio A. Tsuda, Michelle B. de Moraes: Excision of an atypical case of palatal bone exostosis: a case report. In: Journal of Oral Science. Vol. 50, No. 2, 2008, ISSN 1343-4934 , pp. 229-231, PMID 18587217 , doi: 10.2334 / josnusd.50.229 .
- ↑ Peter Pospiech: The prophylactically oriented supply with partial dentures. Thieme, Stuttgart a. a. 2002, ISBN 3-13-126941-3 , p. 4, ( limited preview on Google Books ).
- ↑ Sandro Palla: Determination of the jaw relation. In: Bernd Koeck (Ed.): Total prostheses. 4th edition. 2005, pp. 95–151, here p. 117.
- ↑ Jürgen Setz, Eva Engel: The total denture. Clinical Guide. ( Memento of the original from August 24, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Ivoclar Vivadent, Ellwangen (Jagst) 2003, ISBN 3-00-022411-4 .
- ↑ Peter Pospiech: The prophylactically oriented supply with partial dentures. Thieme, Stuttgart et al. 2002, ISBN 3-13-126941-3 , p. 134.
- ^ Konrad Bork, Walter Burgdorf, Nikolaus Hoede: Oral mucous membrane and lip diseases. Clinic, diagnostics and therapy. Atlas and manual. 3. Edition. Schattauer, Stuttgart a. a. 2008, ISBN 978-3-7945-2486-0 , p. 188, ( limited preview on Google Books ).
- ↑ Carl Partsch : Diseases of the Hartbegilde of the mouth. The shape deviations of the teeth. Changes in the shape of the teeth. In: Carl Partsch (Ed.): The surgical diseases of the oral cavity of the teeth and jaw (= Handbook of Dentistry. Vol. 1). 4th, revised and revised edition. Bergmann, Munich 1932, pp. 62–63, here p. 63, ( limited preview at Google Books ).
- ↑ Individual diver mouthpieces. ADT. Retrieved January 15, 2017.
- ^ Paul Wustrow: The plate prosthesis. Immediate prostheses. In: Christian Bruhn (Hrsg.): Zahnärztliche Prothetik (= Handbook of Dentistry. Vol. 3). 3rd, revised edition. Bergmann, Munich 1930, pp. 436–438, here p. 437, ( limited preview on Google Books ).
- ↑ Peter Pospiech: The prophylactically oriented supply with partial dentures. Thieme, Stuttgart a. a. 2002, ISBN 3-13-126941-3 , p. 160, ( limited preview on Google Books ).
- ↑ Replacement prosthesis / second prosthesis . DocMedicus. Retrieved December 12, 2016.
- ↑ Eliyah Havemann: How do I become a Jew? And if so, why? Ludwig Verlag, Munich 2014, ISBN 978-3-453-28059-5 , p. 71, ( limited preview on Google Books ).
- ↑ Yehuda Spitz: Kashering Teeth ?! Ohr Somayach, March 31, 2012. Retrieved January 18, 2017.
- ↑ Michael Frohne: Teeth - diagnosis and therapy in brass musicians. Jazz realities. Retrieved January 18, 2017.
- ^ Ernst-Jürgen Richter: Implant prosthetics. Overdenture. In: Wolfgang Gernet, Reiner Biffar, Norbert Schwenzer, Michael Ehrenfeld (eds.): Dental prosthetics. 4th, unchanged edition. Thieme, Stuttgart a. a. 2011, ISBN 978-3-13-593604-8 , pp. 84–131, here p. 117, ( limited preview on Google Books ).
- ^ Hermann Böttger: Dental prosthetic treatments in the context of plastic surgery. In: Erwin Gohrbandt , Joachim Gabka, Alfred Berndorfer (eds.): Manual of plastic surgery. Volume 2, Part 1: Special Plastic Surgery. Walter de Gruyter, Berlin a. a. 1973, ISBN 3-11-004649-0 , pp. 31 / 4–31 / 22, ( limited preview on Google Books ).
- ↑ Lukasz Jablonowski, Rutger Matthes, Kathrin Duske, Thomas Kocher: Plasma applications in dentistry, oral medicine and maxillofacial medicine. Use of plasma for cleaning and disinfecting dental prostheses. In: Hans-Robert Metelmann, Thomas von Woedtke, Klaus-Dieter Weltmann (eds.): Plasma medicine. Cold plasma in medical applications. Springer, Berlin a. a. 2016, ISBN 978-3-662-52644-6 , pp. 127–130, here pp. 127–128, ( limited preview on Google Books ).
- ↑ Andreas Schwarzkopf: Hygiene Management in Nursing. In: Christian Jassoy, Andreas Schwarzkopf (Ed.): Hygiene, Infectiology, Microbiology. 2nd, completely revised edition. Thieme, Stuttgart a. a. 2013, ISBN 978-3-13-136132-5 , pp. 176–200, here p. 193, ( limited preview on Google Books ).
- ↑ Low- noise denture cleaning device for the practice. In: Bayerisches Zahnärzteblatt. Vol. 39, No. 7/8, 2004, ISSN 1618-3584 , p. 27.
- ^ Mortality and Burden of Disease Estimates for WHO Member States in 2002. World Health Organization, 2002. Retrieved January 15, 2017.
- ↑ Dental prosthesis services 2015 of diagnosis classes 4.2 and 4.4, as well as 4.6 and 4.8 in: National Association of Statutory Health Insurance Dentists (KZBV). Yearbook. Basic statistical data on contract dental care. Including GOZ analysis. 2016, ZDB -ID 1313467-x , p. 102, ( digitized ).
- ↑ German oral health study (DMS V). National Association of Statutory Health Insurance Dentists. Retrieved January 16, 2017.
- ^ Theo Vos, Abraham D. Flaxman et al.: Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. In: The Lancet . Vol. 380, No. 9859, 2012, pp. 2163-2196, Table 1, PMID 23245607 , doi: 10.1016 / S0140-6736 (12) 61729-2 .
- ↑ Tariffs. Salzburg Regional Health Insurance Fund. Retrieved January 13, 2017.
- ↑ Prices / costs of removable dentures. Retrieved January 13, 2017.
- ^ Norinaga Moriyama, M. Hasegawa: The history of the characteristic Japanese wooden denture. In: Bulletin of the History of Dentistry. Vol. 35, No. 1, 1987, ISSN 1089-6287 , pp. 9-16, PMID 3552092 .
- ↑ Malvin E. Ring: John Greenwood, Dentist to President Washington. In: Journal of the California Dental Association. Vol. 38, No. 12, December 2010, pp. 846-851, PMID 21261186 , ( digital version (PDF; 4.48 MB) ).
- ^ Toothless history. German museum. Retrieved January 18, 2017.
- ↑ John Woodforde: The Strange History of False Teeth. With a foreword and appendix by Annemarie Leibbrand-Wettley . Moos-Verlag, Munich 1968, p. 96.
- ↑ Stephanie Pain: The great tooth robbery. In: New Scientist . Vol. 120, No. 2295, 2001, p. 46, ( online ). Retrieved January 18, 2017.
- ↑ Jan N. Lorenzen: 1813 - The Battle of Nations near Leipzig. In: Jan N. Lorenzen: The great battles. Myths, people, fates. Campus, Frankfurt am Main u. a. 2006, ISBN 3-593-38122-2 , pp. 101–140, here p. 103, ( limited preview on Google Books ).
- ↑ Jan N. Lorenzen: 1813 - The Battle of Nations near Leipzig. In: Jan N. Lorenzen: The great battles. Myths, people, fates. Campus, Frankfurt am Main u. a. 2006, ISBN 3-593-38122-2 , pp. 101–140, here p. 133, ( limited preview on Google Books ).
- ^ Paul O'Keeffe: Waterloo. The aftermath. The Bodley Head, London 2014, ISBN 978-1-84792-182-6 , p. 57, ( limited preview on Google Books ).
- ^ Nicolas Dubois de Chémant (1753-1824): A dissertation on artificial teeth: evincing the advantages of teeth made of mineral paste ... Printed by John Haines, London 1816. The Henry J. McKellops Collection in Dental Medicine. In: The Rare Books section of the Bernard Becker Medical Library. Digitized.
- ↑ Bernard Kurdvk: Giuseppangelo Fonzi. In: Journal of the History of Dentistry. Vol. 47, No. 2, 1999, ISSN 0007-5132 , pp. 79-82, ( digitized version ).
- ↑ Peter Force: A National Calendar ... Davis and Force, Washington 1823 (English), Volume 4, p. 168, accessed March 11, 2017.
- ↑ a b Heinrich Schnettelker: The history of the rubber prosthesis. Freiburg (Breisgau) 2001, dissertation; ( online ).
- ^ Henry W. Noble: Tooth transplantation: a controversial story. A shortened version of a lecture given to the Scottish Society for the History of Medicine on June 15, 2002. ( Online (PDF; 42 KB) ). Retrieved January 18, 2017.
- ↑ Terry Wilwerding: History of Dentistry 2001. (PDF; 158 kB). Retrieved January 18, 2017.
- ^ Horton D. Kimball: Modern denture base materials, and what to expect of them. In: The Journal of the American Dental Association. Vol. 25, No. 2, 1938, ISSN 0002-8177 , pp. 243-252, doi: 10.14219 / jada.archive.1938.0042 .
- ↑ A. Schmidt: The history of methacrylates in stomatology. In: Dental Technology. Vol. 19, 1978, ISSN 0513-7926 , pp. 436-444.
- ↑ Christian Bruhn, F. Gutowski, A. Gysi, F. Hauptmeyer, Stephan Loewe, Karl Kukulies, Paul Wustrow: Zahnärztliche Proothetik. Springer, Heidelberg 2013, ISBN 978-3-642-99582-8 , p. 116, ( limited preview in Google Books ).
- ^ JB Mulliken, RM Goldwyn: Impressions of Charles Stent. In: Plastic and reconstructive surgery. Vol. 62, No. 2, August 1978, ISSN 0032-1052 , pp. 173-176, PMID 353841 .
- ↑ S. Sterioff: Etymology of the word "stent". In: Mayo Clinic proceedings. Vol. 72, No. 4 April 1997, ISSN 0025-6196 , pp. 377-379, PMID 9121189 .
- ↑ Rainer Habekost: Impression with alginate: Perfect images with alginate. epubli, Berlin. January 3, 2012. ISBN 978-3-8442-1539-7 . P. 20, ( limited preview in Google Books ).
- ^ Heinrich F. Kappert, Karl Eichner: Dental materials and their processing. 1. Basics and processing. Thieme Stuttgart 2005, ISBN 978-3-13-127148-8 , pp. 274-302, ( limited preview in Google Books ).
- ↑ The impression taking in dentistry. 3M. Retrieved January 21, 2017.
- ^ Kerstin Godau: The historical, prosthetic collection of the Center for Dentistry, Oral and Maxillofacial Medicine of the Martin Luther University Halle-Wittenberg. Dissertation, Martin Luther University Halle-Wittenberg 2005, pp. 225–238, digitized. Retrieved January 23, 2017.
- ↑ András Szentpétery: Three-dimensional mathematical movement simulation of articulators and their application in the development of a "software articulator". University and State Library of Saxony-Anhalt, habilitation thesis (2000), pp. 6–37, digitized. Retrieved January 21, 2017.
- ^ Kerstin Godau: The historical, prosthetic collection of the Center for Dentistry, Oral and Maxillofacial Medicine of the Martin Luther University Halle-Wittenberg. Dissertation, Martin Luther University Halle-Wittenberg 2005, pp. 6–48, digitized. Retrieved January 23, 2017.
- ↑ Albert Gerber 1907-1990. ( Memento from June 30, 2017 in the Internet Archive ) Gerber Condylator Service.
- ↑ Max Bosshart: Function & Aesthetics. Rehabilitation of the edentulous using the original Gerber method. Quintessenz, Berlin et al. 2014, ISBN 978-3-86867-170-4 , ( online. Accessed January 27, 2017).
- ↑ Exemplary: Ulrike Schulte-Kramer: reproducibility and comparability of the orienting jaw relation determination in the context of anatomical impressions in edentulous patients using the Ivotray and Centric Tray system. Dissertation (2006), Westfälische Wilhelms-Universität, Münster, ( digitized version ). Retrieved January 19, 2017.
- ↑ Joachim Bredenstein: Implant-supported full denture. In: Almut Rech (Hrsg.): Implantatprothetik. 2. Neuer Merkur, Munich 2004, ISBN 3-929360-97-7 , pp. 229-235, ( limited preview in Google Books ).