HistoScanning
Prostate HistoScanning (HS) (spelling of the manufacturer) is an ultrasound-based diagnostic method or the corresponding device that has been used to detect prostate cancer since 2008 . It is based on analyzing the image noise , which is normally filtered out from ultrasound images as interference. Frequency mixing and the strength of the noise are influenced by tissue properties such as water content, cell size, and blood vessel density. You can therefore draw conclusions about differences in the tissue that cannot be seen in the ultrasound image.
The target group are men with suspected prostate cancer, which is usually caused by an increase in PSA in the blood. Since this is extremely common in older people, and the operation or irradiation of the prostate has severe side effects, the patient to be treated must be carefully selected. The goal of HS is to locate clinically significant prostate cancer sites (i.e., those with malignant behavior) with sufficient accuracy that a needle can reach them. The currently common, untargeted 12-quadrant biopsy of the entire prostate could then be replaced by a targeted needle biopsy.
Since the noise data are recorded with a slightly modified, modern ultrasound device anyway, the HS method could be used anywhere on an outpatient basis. HistoScanning thus competes with methods such as computer-aided transrectal sonography (C-TRUS), contrast -enhanced sonography , and multiparametric MRI , all of which are relatively expensive and are not offered nationwide.
HS is not yet an established procedure, in Germany the statutory health insurance does not bear the costs. Patents, naming rights and exclusive distribution are held by the Swiss company R-Action Distribution Sàrl .
Working principle
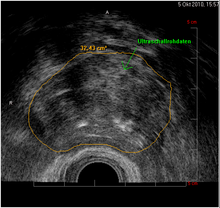
In the case of ultrasound imaging processes, the ultrasound data obtained are converted into gray tones in order to generate an image and visualize existing structures. HistoScanning is not an ultrasound imaging process, but ultrasound is only used as a kind of "tool". The developers' idea was to train an AI to detect prostate cancer by feeding it sonography data and the corresponding tissue sections. The training data set consisted of the data of 14 patients whose prostates had been surgically removed and completely histologically processed. The transducer is located in the rectum and completely scans the prostate. Three algorithms calculate cell density, heterogeneity and vascularization, and superimpose these parameters in color on the ultrasound image.
This tissue differentiation is intended to provide the user with a visual aid to decision-making, both for the diagnosis and for planning a possibly necessary treatment. Only a subsequent biopsy can determine whether the marked areas are actually tumor tissue.
A further development is the so-called "TT = True-Targeting" software, which allows, after the diagnosis / evaluation has been completed, areas categorized as suspicious to be targeted histo-scanning-controlled "real-time" during the biopsy, in order to also hit the suspicious areas more reliably . The latest technical development is aimed at enabling a fusion of the HistoScanning results with MRT images or other diagnostic methods in order to be able to make even more precise predictions in comparison. A fusion with treatment software (e.g. HIFU, cryo or brachytherapy) should then be possible in order to control the procedure in a targeted manner. These technologies are currently still in development.
Study situation
The excellent first results (Braeckman et al. Reported 100% sensitivity and 100% NPV for tumors larger than 5 mm in size) were not confirmed in the following years. Some authors only achieved sensitivities below 30% and NPV 50%, with the larger studies tending to have worse results. Wysock et al. came to the conclusion in 2017 that the study situation does not give the method any significant role in the diagnosis of prostate cancer. Other methods, in particular the mpMRI, are clearly more suitable. The S3 guideline of the scientific and medical societies explicitly advises against its use. The costs of the procedure (approx. 590 euros) are not covered by the German statutory health insurance . However, both private funds and grants usually reimburse their members for this expense.
literature
- J. Braeckman, P. Autier, C. Garbar, MP Marichal, C. Soviany, R. Nir, D. Nir, D. Michielsen, H. Bleiberg, L. Egevad, M. Emberton: Computer-aided ultrasonography (HistoScanning) : a novel technology for locating and characterizing prostate cancer. In: BJU Int . 101, 2008, pp. 293-298.
- J. Braeckman, P. Autier, C. Soviany, R. Nir, D. Nir, D. Michielsen, K. Treurnicht, M. Jarmulowicz, H. Bleiberg, S. Govindaraju, M. Emberton: The accuracy of transrectal ultrasonography supplemented with computer-aided ultrasonography for detecting small prostate cancers. In: BJU Int. 102, 2008, pp. 1560-1565.
- LAM Simmons, P. Autier, F. Zát'ura, J. Braeckman, A. Peltier, I. Romic, A. Stenzl, K. Treurnicht, T. Walker, D. Nir, CM Moore, M. Emberton: Detection, Localization and characterization of prostate cancer by Prostate HistoScanning. In: BJU Int.
- J. Schiffmann et al .: Does HistoScanning ™ predict positive results in prostate biopsy? A retrospective analysis of 1,188 sextants of the prostate. In: World J Urol. 32 (4), 2014 Aug, pp. 925-930. doi: 10.1007 / s00345-014-1330-5
- Wysock, JS, Xu, A., Orczyk, C. et al .: HistoScanning ™ to Detect and Characterize Prostate Cancer - a Review of Existing Literature. Curr Urol Rep 18, 97 (2017). doi: 10.1007 / s11934-017-0747-y
Individual evidence
- ^ Prostate Cancer Diagnostics / HistoScanning ™ TT. In: manufacturer website. R-Action Distribution Sàrl, accessed on May 21, 2020 .
- ↑ Guideline Program Oncology: Recommendation 5.12. In: S3 guideline for prostate cancer. May 2019, p. 51 (long version) , accessed on May 21, 2020 .