Histoplasmosis
| Classification according to ICD-10 | |
|---|---|
| B39 | Histoplasmosis |
| ICD-10 online (WHO version 2019) | |
The histoplasmosis (also reticuloendothelial Zytomykose or Darling's disease ) is a conditional fungal systemic infectious disease and is Histoplasma species, especially the sprouting Histoplasma capsulatum causes. Depending on the occurrence of the pathogen, histoplasmosis is widespread in South, Central and parts of North America, Indonesia and Africa. Cases in Western Europe are the exception.
In the majority of cases, this mycosis only or predominantly affects the lungs .
pathology
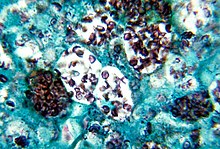
Infection with the dimorphic fungus living in the ground occurs through inhalation of the spores . These are phagocytosed in the lungs by macrophages . They develop into a yeast form within the macrophages , which multiplies through sprouting . Small, initially epitheloid-cell granulomas develop, some of which later show a “caseating” necrosis in the center. The healing takes place under calcification. Histoplasms can be carried over the bloodstream and secondary to lymph nodes , liver and spleen . The reticuloendothelial system is particularly involved in the infestation.
Mainly two varieties are pathogenic to humans , of which the variety caspulatum is smaller with a diameter of 2-4 µm and the variety duboisii is slightly larger with 6-12 µm - and only occurs in Africa.
clinic
Most infections are asymptomatic and silent; that is, they are not noticed by the sick. The infectious dose and the immune system of the host are decisive for any symptoms . After an incubation period of 3 to 17 days, they can manifest as a general feeling of malaise, fever, and dry cough . In AIDS -Erkrankten and immunosuppressed patients Histoplasmosen are more frequent and more severe. Here severe disseminated to (widely distributed), ulcerated tissue damage. Deaths are also described.
diagnosis
The disease presents itself clinically in a variety of ways. The pathogen can be detected in blood, biopsies or bronchoalveolar lavage. Using ELISA or PCR, it is also possible to detect histoplasmosis antigen in blood or urine. Due to the long half-life of the fungal antigens, the antigen level only drops slowly during treatment, which is why the test can be positive for a longer period of time even after successful treatment. An antibody test is also available. The fungus can be cultivated on Sabouraud dextrose agar for detection.
therapy
In immunocompetent people, the disease is usually self-limiting and does not require treatment.
Only in severe disseminated courses of treatment is necessary in severe cases intravenously with liposomal amphotericin B is performed. Then, in severe cases, itraconazole is given orally for one year, which is also an alternative primary therapy in less severe cases. In pulmonary histoplasmosis, 6–12 weeks of therapy are usually sufficient.
Web links
Individual evidence
- ↑ a b Katrina A. Armstrong, Justine V. Cohen, Jo-Anne O. Shepard, Erik E. Folch, Michael K. Mansour, Jonathan A. Stefely: Case 16-2020: A 47-Year-Old Woman with Recurrent Melanoma and Pulmonary Nodules . New England Journal of Medicine 2020, Issue 21 May 21, 2020, pages 2034-2043, DOI: 10.1056 / NEJMcpc1916258
- ^ Karen M. Frank, D. Kyle Hogarth, Jonathan L. Miller, Saptarshi Mandal, Philip J. Mease, R. Jude Samulski, Glen A. Weisgerber, John Hart: Investigation of the cause of death in a gene-therapy trial. In: The New England Journal of Medicine. Vol. 361, No. 2, 2009, pp. 161-169, PMID 19587341 , doi : 10.1056 / NEJMoa0801066 .
