AIDS
AIDS [ɛɪ̯t͡s] ( acronym of the English acquired immune deficiency syndrome "acquired immunodeficiency syndrome", also called "Acquired immune deficiency syndrome") refers to a specific combination of symptoms that caused in humans by an HIV -induced infection destruction of the immune system occur. The sick develop life-threatening opportunistic infections and tumors .
AIDS was recognized as a disease in its own right by the US Centers for Disease Control and Prevention (CDC) on December 1, 1981 , after defining the coincidence of certain symptoms as AIDS . AIDS is one of the sexually transmitted diseases . According to the United Nations Joint Program on HIV / AIDS(UNAIDS) there were around 37.9 million HIV-positive people worldwide in 2019. In 2019 there were around 1.7 million new HIV infections (4,650 per day) and around 0.77 million people died as a result of HIV / AIDS. 35 million people have died of AIDS since the epidemic began. The proportion of people infected with HIV is on average around 0.8% of 15 to 49 year olds worldwide, but in some African countries it is around 25%. No vaccination is available. The more effective treatment of HIV-infected people with new drugs has made AIDS less common in Central Europe .

Definition and classification
Classification in the ICD-10
| Classification according to ICD-10 | |
|---|---|
| B20 | Infectious and parasitic diseases as a result of HIV disease |
| B20.0 | Mycobacterial infections due to HIV disease (e.g. tuberculosis due to HIV disease) |
| B20.1 | Other bacterial infections due to HIV disease |
| B20.2 | Cytomegaly due to HIV disease |
| B20.3 | Other viral infections due to HIV disease |
| B20.4 | Candidiasis due to HIV disease |
| B20.5 | Other mycoses due to HIV disease |
| B20.6 | Pneumocystis pneumonia due to HIV disease |
| B20.7 | Multiple infections as a result of HIV disease |
| B20.8 | Other infectious and parasitic diseases resulting from HIV disease |
| B20.9 | Unspecified infectious or parasitic disease resulting from HIV disease |
| B21 | Malignant neoplasms as a result of HIV disease |
| B21.0 | Kaposi's sarcoma as a result of HIV disease |
| B21.1 | Burkitt's lymphoma as a result of HIV disease |
| B21.2 | Other types of non-Hodgkin lymphoma due to HIV disease |
| B21.3 | Other malignant neoplasms of the lymphatic, hematopoietic and related tissue as a result of HIV disease |
| B21.7 | Multiple malignant neoplasms as a result of HIV disease |
| B21.8 | Other malignant neoplasms due to HIV disease |
| B21.9 | Unspecified malignant neoplasms as a result of HIV disease |
| B22 | Other specified diseases resulting from HIV disease |
| B22.0 | Encephalopathy due to HIV disease |
| B22.1 | Interstitial lymphoid pneumonia due to HIV disease |
| B22.2 | Cachexia syndrome as a result of HIV disease |
| B22.7 | Several diseases classified elsewhere due to HIV disease |
| B23 | Other disease conditions as a result of HIV disease |
| B23.0 | Acute HIV infection syndrome |
| B23.1 | (Persistent) generalized lymphadenopathy as a result of HIV disease |
| B23.2 | HIV disease blood and immune abnormalities, not elsewhere classified |
| B23.8 | Other specified conditions resulting from HIV disease |
| B24 | Unspecified HIV disease |
| ICD-10 online (WHO version 2019) | |
In the world-wide recognized medical diagnosis classification system ICD-10 of the WHO , both the HIV infection and numerous diseases as a consequence of an HIV infection can be coded. The exact type of secondary illness is encoded in a fourth digit in the version of the ICD-10 last updated by the World Health Organization for 2013, for example: B20.6 Pneumocystis pneumonia as a result of HIV disease .
Classification of HIV infection and definition of AIDS
CDC definition
According to the case definitions of the US Centers for Disease Control and Prevention (CDC), a confirmed positive HIV test is considered evidence of HIV infection. The rating of HIV infection by severity including AIDS was changed significantly in 2008. Until then, clinical findings and laboratory values were classified separately and presented as letter-number coding. Asymptomatic and HIV-related but not AIDS-defining diseases were also included. Since 2008 only AIDS-defining diseases have been taken into account. The classification according to the number of CD4-positive T lymphocytes ( T helper cells ) and the list of AIDS-defining diseases, however, remained unchanged.
The letter-digit coding, which is still widely used in practice, is therefore out of date. It should be noted that the case definition is primarily used for epidemiological monitoring of HIV and AIDS and not as a guide for clinical diagnosis. A case classification cannot be downgraded again; therefore it may not say anything about the current status of a patient.
| HIV rating in adults and adolescents * | |||
|---|---|---|---|
| stage | CD4 + cell count per µl |
as a percentage of all lymphocytes |
|
| 1 | ≥ 500 | > 29% | and not an AIDS-defining disease |
| 2 | 200-499 | 14-28% | and not an AIDS-defining disease |
| 3 (AIDS) | <200 | <14% | or at least one AIDS-defining disease |
| Unknown | No values | and no finding of AIDS-defining disease available | |
| * Proof of HIV infection is required | |||
AIDS includes evidence of HIV infection and an AIDS-defining disease (stage 3) or evidence of HIV infection and a CD4 cell count of <200 cells or <14%. The CDC defined AIDS-defining diseases / symptoms as follows:
- Candidiasis (fungal infection) of the bronchi , windpipe, or lungs
- Oesophageal candidiasis (fungal infection of the esophagus )
- CMV infections (except liver, spleen, lymph nodes)
- CMV retinitis ( inflammation of the retina with loss of vision )
- Encephalopathy , related to HIV
- Herpes simplex infections: chronic ulcers ( lasting > one month; or bronchitis, pneumonia, esophagitis)
- Histoplasmosis , disseminated or extrapulmonary
- Isosporiasis , chronic, intestinal, lasting more than a month
- Kaposi's sarcoma
- Coccidioidomycosis , disseminated or extrapulmonary
- Cryptococcosis , extrapulmonary
- Cryptosporidiosis , chronic, intestinal, lasting> one month
- Burkitt lymphoma
- Lymphoma , immunoblastic
- Lymphoma, primarily cerebral
- " Mycobacterium avium complex" or M. kansasii , disseminated or extrapulmonary
- Mycobacteriosis, other or unidentified species disseminated or extrapulmonary
- Pneumocystis pneumonia
- Recurrent bacterial pneumonia (> two within a year)
- Progressive multifocal leukoencephalopathy
- Salmonella - septicemia , recurrent
- tuberculosis
- Toxoplasmosis , cerebral
- Wasting syndrome (caused by HIV)
- Cervical cancer , invasive
European definition
According to the case definition of the European Commission , a confirmed positive HIV test is considered evidence of HIV infection. An assessment of the HIV infection according to the degree of severity is not carried out.
AIDS is considered to be evidence of HIV infection and one of the diseases specified in the European case definition for AIDS. These are identical to those of the CDC list (see there). An AIDS diagnosis based solely on laboratory values without any clinical findings (CDC stage 3) was rejected.
The European case definition is used for epidemiological surveillance of HIV and AIDS.
WHO definition
According to the WHO case definition, a confirmed positive HIV test is considered evidence of HIV infection.
| Immunological and Clinical HIV Assessment in Adults and Adolescents * | |||
|---|---|---|---|
| stage | Symptoms | CD4 + cell count per µl % of all lymphocytes |
|
| 1 | Asymptomatic | ≥ 500 | Asymptomatic illness (s) |
| 2 | Mild symptoms | 350-499 | Disease defined for this stage, e.g. B. Herpes zoster |
| 3 | Advanced symptoms | <350 | Disease defined for this stage, e.g. B. Oral hairy cell leukoplakia |
| 4 (AIDS) | Serious symptoms | <200 <15% |
or at least one of the AIDS-defining diseases |
| * Proof of HIV infection is required | |||
For epidemiological surveillance, advanced HIV infection in adults and adolescents is defined as evidence of HIV infection and disease in clinical stages 3 or 4.
In adults and adolescents, AIDS is the proof of HIV infection and an AIDS-defining disease (stage 4) or proof of HIV infection and a CD4 cell count of <200 cells or <15%.
The AIDS-defining diseases / symptoms are largely identical to those in the CDC list.
transmission


The HIV virus is transmitted with the body fluids blood , semen , vaginal secretions , liquor and breast milk . Potential entry points are fresh, still bleeding wounds in the mucous membranes (conjunctiva, mouth, nose, vaginal and anal mucosa) or insufficiently horny, easily vulnerable areas of the outer skin ( glans , inside of the penile foreskin ). The most common routes of infection are unprotected vaginal or anal intercourse , the use of contaminated syringes with intravenous drug consumption and oral intercourse (when mucous membrane contact with semen or menstrual blood). During oral intercourse with uninjured oral mucosa, contact with pre-ejaculate or vaginal secretions represents a negligible risk of infection, as does passive oral intercourse. Men who have sex with men are considered a risk group. How high the risk is during sexual intercourse depends primarily on the viral load in the semen , in the vaginal secretions and in the blood. This is particularly high in the first few weeks after infection, before antibodies have formed, then decreases and increases again in the later stages of the disease.
HIV is not transmitted through saliva , sweat , tear fluid , droplet infection, or through insect bites. Likewise, contamination of intact skin with virus-containing (body) fluids does not lead to infection. Body contact in everyday social interaction, the shared use of dishes, cutlery, etc., and the shared use of sanitary facilities also do not pose a risk of infection.
Patients with full AIDS disease are at risk of infection with the typical opportunistic pathogens: viruses of the herpes group, candida, streptococci, pneumococci. Partners of patients with full-blown AIDS should also find out about these pathogens and their routes of infection.
| Route of infection | Risk per 10,000 contacts with an infectious source |
In percent |
|---|---|---|
| Parenteral | ||
| Blood transfusion | 9 250 | 92.5 |
| Drug injection with a used needle | 63 | 0.63 |
| Needle stick through the skin | 23 | 0.23 |
| Sexual (unprotected intercourse) | ||
| Anal intercourse, receiving partner | 138 | 1.38 |
| Vaginal intercourse, receiving partner | 8th | 0.08 |
| Anal intercourse, introductory partner | 11 | 0.11 |
| Vaginal intercourse, introductory partner | 4th | 0.04 |
| Oral sex | low 1 | - |
|
1 Cases of HIV transmission through oral sex have been scientifically documented but are rare. A precise estimate of the risk is not available due to the poor data situation. |
||
Transfer mother / child
The risk of infection to a child by an HIV-infected mother during pregnancy or childbirth is estimated to be 10 to 30%. If the mother is known to be infected with HIV, the risk of transmission to the child can be reduced to less than one percent by giving antiretroviral drugs (to the mother before and after the birth), giving birth by caesarean section and not breastfeeding the child become.
However, breastfeeding is recommended in developing countries despite the mother's HIV infection, provided that antiretroviral drugs are used that reduce the risk of infection. This is because breastfeeding has important advantages over industrially produced ready-to-eat foods, especially if these are prepared under poor hygienic conditions or with unclean water, as is often the case in developing countries. Breast milk also improves the chances of survival for HIV-infected infants who, for example, have been infected before or during birth. The WHO therefore recommends exclusive breastfeeding for a period of six months also for HIV-positive mothers.
Transmission through blood transfusions
Blood transfusions also carry the risk of HIV infection. However, routine monitoring of blood donations , as is carried out in Germany, greatly reduces this, so that nowadays the risk of getting an HIV infection by transfusing a blood product is negligible.
In the first few years after the discovery of HIV (1981), the risk of infection via contaminated blood products was very high, as there were no reliable laboratory tests for the detection of the HI virus to test blood donors. In addition, the risk of infection is particularly high when infected blood products are transfused (approx. 90 percent). People suffering from haemophilia , the blood disease, who had to receive regular transfusion of coagulation factor concentrates, were particularly affected . These coagulation factor concentrates have been prepared from numerous donated plasma. As a result, by the late 1980s approximately 50% of the approximately 15,000 hemophilia sufferers in the United States had become infected with HIV. In Germany, too, around 1,800 of the approximately 3,000 haemophilia sufferers and a further 460 people were infected by blood product transfusions, although even then there was the (albeit very expensive) possibility of virus inactivation of the plasma preparations. The "blood scandal" that then developed among the German public ultimately led to the dissolution of the Federal Health Office , which was the supervisory authority for the safety of blood products, by the then Federal Minister of Health Horst Seehofer . As a result of the scandals surrounding blood products infected with HIV or the hepatitis C virus , the blood transfusion system in Germany and other countries was subjected to rigorous and strict legal controls. Testing of all blood products for HIV antibodies has been a legal requirement in the USA and Germany since 1985 , which reduced the risk of infection to significantly less than 1: 100,000 (almost all transfusion-related infections occurred before 1985). However, there was still a small residual risk, as antibodies can only be detected a few weeks after the virus infection (“ diagnostic gap ”). Since May 1, 2004, testing of every blood donation has been required by law in Germany not only for antibodies, but also directly for the presence of HIV- RNA . This means that fresh infections can also be detected. The risk of acquiring an HIV infection through an infected blood product is estimated today in Germany at 1: 4.3 million or less.
Transmission through needles / cannulas / needle sticks
In the early days of the epidemic in particular, many intravenous drug addicts became infected by sharing hypodermic needles. Doctors and nursing staff also have a certain risk of infection from needlestick injuries in the operating theater or after punctures on infected patients. The risk of infection from needle sticks depends very much on the circumstances. The risk of infection is given on average with 0.3% and increases with the following factors: very deep injuries (16-fold increased), visible traces of blood on the needle or needle was previously in a vein or artery of the carrier (each increased five-fold), with high Viral load of the carrier (increased six-fold). The risk with hollow needles is higher than with closed needles.
The risk of sharing a cannula , e.g. B. when injecting heroin , is around 0.7% and decreases with the time interval between injections , but only slowly, since blood trapped in the cannula can remain infectious for days. It is generally possible to boil the needles, but commercially available needles are often not suitable because the plastics used are not adequately heat-resistant. Chemical disinfection with bleach or other disinfectants can significantly reduce the risk, but is not sufficient to reliably rule out transmission.
- Special case - use of non-sterile, re-used cutting tools for female genital mutilation
The multiple use of razor blades or other tools in genital mutilation, also known as female circumcision, of girls and women, which often occurs in large numbers within a limited period of time, can lead to the transmission of bacteria and viruses, including HIV. AIDS rates of sometimes more than 20% in the younger population of South African regions indicate the extent of the problem.
Transmission through sexual intercourse
The individual risk of becoming infected with HIV through sexual intercourse is very variable and depends on many factors. An infection is possible after a single sexual intercourse, but there are also known cases in which, despite several years of unprotected sexual contact with an infected partner, no infection occurred. A concomitant sexually transmitted disease increases the risk of infection by a factor of 5 to 10, a high viral load of the carrier even increases by a factor of 10 to 30. Freshly infected people have a high viral load in the first few weeks, as the body does not have any specific antibodies against the HI virus at this stage. Sexual intercourse during a woman's menstrual period is associated with an increased risk of infection for both partners; circumcised men have a lower risk of infection. Overall, the risk of infection does not seem to be constant over the number of contacts, so that the risk of individual contacts is possibly significantly too low. With antiretroviral therapy, the risk of transmission decreases significantly due to the falling viral load in blood and secretions.
- Vaginal intercourse: Unprotected vaginal intercourse is associated with a comparatively high risk (0.05–0.1% per sex act).
- Dry sex : The risk of infection is significantly increased here, as tears and bleeding of the vaginal mucosa often occur due to the painful friction and condoms (if used) remain functional in the dry environment less often.
- Small cracks in the mucous membrane often occur during anal intercourse, which is why the risk is significantly increased compared to vaginal intercourse.
- Fellatio , oral sex with sperm ingestion through the mouth: The risk of infection is very low, but infection cannot be ruled out.
- The risk of infection through pre-ejaculate is very small and negligible during oral sex.
- Cunnilingus , oral sex in women: The risk is also rated as extremely low as long as there is no contact with menstrual blood.
- Anilingus : The risk is estimated to be extremely low.
- Other sexual practices that do not involve contact with mucous membranes, blood, semen or vaginal secretions have an extremely low risk of infection.
Post-exposure prophylaxis
Sometimes there is an option to counter a possible HIV infection after a risk situation. Such measures include washing the penis after intercourse, squeezing the stab wounds, and treating it with disinfectant . There is also the option of post-exposure prophylaxis (PEP). This offers the best possible protection if treatment is started within two hours of exposure, but can still be effective through the mucous membranes for up to 24 hours after intravenous exposure and up to 72 hours after other exposure. Therefore, after a well-founded suspicion of infection, a doctor should always be consulted immediately, who will inform about possible measures and who can also initiate them. The medication for PEP essentially corresponds to the antiretroviral therapy of an HIV-positive patient and usually lasts four weeks.
HIV tests
HIV tests are divided into addiction tests and confirmatory tests. The aim of a search test ( e.g. ELISA search test ) is to identify as many infected people as possible - at the price that some non-infected people will also test positive by mistake. If a person tests positive in the addiction test, a confirmatory test (in Germany and the USA: Western blot confirmation test ) is required in many countries to prevent a false positive diagnosis. Most HIV tests are done in a laboratory. However, there are also quick tests , some of which can show a result after a few minutes without technical aids.
An HIV test may only be carried out with the express consent of the person concerned, testing without the knowledge of the patient is legally inadmissible and can be punished accordingly.
Anonymized reporting requirements
In Germany, direct or indirect evidence of HIV does not have to be reported by name according to Section 7 (3) of the Infection Protection Act (IfSG). So a positive HIV test from the laboratory must be reported anonymously to the Robert Koch Institute in Berlin ( Section 8 (1) numbers 2, 3 or 4, Section 10 (2) and (4) IfSG).
In Austria only AIDS, not just HIV infection, is notifiable . Because an AIDS disease is defined according to the AIDS law if there is evidence of an infection with the HI virus as well as at least one indicator disease ( § 1 AIDS law). Such an illness and any death caused by it must be reported ( Section 2 of the AIDS Act). The report must be submitted to the Ministry of Health in Vienna within one week of the diagnosis. However, only the initials (first letter of the first name and family name), gender and date of birth and relevant anamnestic and clinical information are to be transmitted ( Section 3 AIDS Act).
In Switzerland met clinical criteria for the disease are AIDS and the positive laboratory analysis findings for HIV notifiable and that after the Epidemics Act (EpG) in connection with the epidemic Regulation and Annex 1 and Annex 3 of the Regulation of EDI on the reporting of observations of communicable Diseases of man . The doctor, hospital, etc. (only) have to report the first name code, place of residence, date of birth, gender, nationality and country of origin, the laboratory (only) have to report the first name code, place of residence, date of birth and gender of the person.
Course of disease
An HIV infection has four phases:
Acute phase
Flu-like symptoms such as fever , night sweats , swollen lymph nodes, and nausea can occur two to six weeks after infection .
The most common symptoms of acute HIV infection are (according to the likelihood of occurrence):
- 80% fever
- 78% exhaustion , tiredness
- 68% malaise , feeling sick
- 54% headache
- 54% loss of appetite
- 54% arthralgia (joint pain)
- 51% rash
- 51% night sweats
- 49% myalgia (muscle pain)
- 49% nausea
- 46% diarrhea (diarrhea)
- 46% fever and rash (as a combination)
- 44% pharyngitis or swallowing pain
- 37% oral ulceration (ulcer in the mouth)
- 34% stiff neck (probably due to the swollen lymph nodes that are also located there)
- 32% weight loss greater than 2.5 kg
- 24% photophobia
However, some patients do not notice or have none of the above symptoms. Since the symptoms are very unspecific and can have many other causes, HIV infections often go undetected at first. An HIV-positive diagnosis cannot be made based on symptoms of the acute phase alone, but only with an HIV test.
A positive HIV-RNA test by RT-PCR and a negative or "borderline" confirmatory test are used to diagnose an acute HIV infection . HIV infections six weeks or more ago are usually diagnosed with an antibody / antigen screening test instead of PCR.
Latency phase
During this time, the virus multiplies in the body. Those affected, if they know of their infection, suffer psychologically at best, but physical symptoms often do not occur. The latency period lasts an average of nine to eleven years. There are both patients who develop AIDS within months of being infected and those who, despite being infected in the 1980s and without antiretroviral therapy, have not progressed to AIDS to this day.
AIDS Related Complex (ARC)
This expression was previously used for clinical stage B of the CDC classification (i.e. the occurrence of clinical symptoms that are not, however, AIDS-defining diseases). If left untreated, the transition to the full AIDS picture follows.
Illness phase
The diagnosis of AIDS is made when certain infections or malignant tumors, the so-called AIDS-defining diseases, are diagnosed in an HIV-positive person. The infections are known as opportunistic infections . They are often harmless to the (intact) immune system of a healthy person. However, due to the compromised immune system of an HIV-positive person, the organism cannot defend itself adequately; the infections mentioned above occur. The number of T-helper cells in the blood of an HIV-infected person serves as a measure of the destruction of the immune system .
therapy
The indication for the treatment of an HIV infection results from the clinical findings (HIV-associated symptoms and diseases, opportunistic infections), immune status (CD4-positive T helper lymphocytes) and virus dynamics (HI viral load) in the infected patients.
Highly Active Antiretroviral Therapy (HAART)
With Highly active antiretroviral therapy (HAART) drug combination therapy of at least three antiretroviral agents called. The aim of HAART is to reconstitute the immune system and prevent the onset of AIDS. A successful HAART pushes the viral load (concentration of the HI virus) in the blood below the detection limit, whereupon the number of CD4 + cells increases again and thus the immune system is strengthened against opportunistic infections and other AIDS-defining diseases. Since the virus quickly develops resistance to individual active substances, the therapy using three antiretroviral active substances has established itself. In current drugs, these three active ingredients are combined in one tablet that is taken once a day.
Antiretroviral therapy can significantly extend the life expectancy of HIV-infected people, but cannot completely eradicate the virus - and thus cause a cure. In addition, serious side effects can sometimes occur, which can usually be countered by changing the combination of active ingredients. Once ART has been started, it should not be discontinued to prevent the development of resistance. Regular tablet intake is essential for the same reason (see Adherence ).
Basic combinations (nucleoside / nucleotide combinations such as tenofovir / emtricitabine or abacsavir / lamivudine) were (2009) combined with an NNRTI (such as efavirenz or nevirapine) or a PI (such as atazanavir, fosamprenavir, lopinavir or saquinavir) for initial therapy.
Due to new medical study results as well as the development and approval of new antiretroviral drugs and substance classes, HAART is in a continuous development process. Nevertheless, there are clear guidelines at national, European and international level on the various aspects of antiretroviral therapy. Several classes of active ingredients are currently used: nucleoside and nucleotide analogs (NRTIs), non- nucleoside reverse transcriptase inhibitors (NNRTIs), HIV protease inhibitors (PI), entry and fusion inhibitors and integrase inhibitors .
The criteria for the best time to start a HAART are defined in the respective national guidelines. These weigh the risk of developing AIDS against the risk of possible long-term toxicity and the development of resistance.
The European recommendation for starting therapy takes three factors into account: the clinical picture of the patient, his CD4 + level and the viral load.
HAART is strongly recommended for patients who already have AIDS-defining diseases (CDC C). HAART is also recommended if diseases that indicate a weakened immune system but are not AIDS-defining (CDC B) occur. This also applies to patients who are symptom-free, but whose number of CD4 + cells is below 350. According to the recommendation, starting HAART is also advisable in patients with a CD4 + value between 350 and 500 if there is a high viral load (> 100,000).
Due to the far-reaching consequences for the patient, the decision is made individually so that the patient is adequately informed beforehand about risks and side effects and is mentally prepared for the therapy.
Active ingredients
Nucleoside Reverse Transcriptase Inhibitors (NRTIs)
Nucleoside analogs , also called nucleoside reverse transcriptase inhibitors (NRTI, colloquially known as “nukes”), target the reverse transcriptase , an enzyme of the HI virus that “translates” the viral RNA genome into double-stranded DNA. Another viral enzyme, the integrase , then builds this viral DNA into the DNA of the human host cell. The NRTIs represent an alternative substrate and compete with the physiological (“endogenous”) nucleosides , but differ from these through a modified sugar molecule . The incorporation of the NRTI hinders the structure of the double-strand bond and therefore leads to chain breaks in the virus DNA.
The active ingredients zidovudine (azidothymidine, AZT) and stavudine (d4T) correspond to the DNA building block thymidine , lamivudine (3TC) correspond to cytidine , while didanosine (ddl), analogous to inosine and abacavir, is a guanosine analogue. A combination of analogues with the same starting point (e.g. AZT and d4T) does not make sense.
Numerous side effects can occur during therapy with NRTIs. Often headaches , gastrointestinal distress, bloating or nausea, vomiting and diarrhea, and general fatigue. Prolonged use can lead to lactic acidosis (accumulation of lactic acid in the blood), myelotoxicity (bone marrow damage), damage to peripheral nerves and inflammation of the pancreas . Also, lipodystrophy , one even with therapy with HIV protease inhibitors observed rearrangement of body fat may occur with prolonged use of NRTIs.
Many of these side effects are a result of mitochondrial toxicity : Mitochondria , which are responsible for the supply of energy in the cells, also need nucleosides. The incorporation of NRTIs instead of nucleosides leads to metabolic disorders and degeneration of the mitochondria. There are considerable differences in the toxicity of the individual substrates.
NRTIs are taken up unchanged into the cell and activated there by phosphorylation . They are mainly eliminated via the kidneys (renally) and therefore have little interaction with drugs that are metabolized in the liver.
Next NRTIs are emtricitabine and tenofovir .
Non-nucleoside reverse transcriptase inhibitors (NNRTIs)
While NRTIs, as “wrong” building blocks, inhibit reverse transcriptase, non-nucleoside reverse transcriptase inhibitors (NNRTIs) bind directly to this enzyme, close to the substrate binding site for nucleosides. There are currently three NNRTIs on the market: nevirapine (NVP), delavirdine (DLV) and efavirenz (EFV). While nevirapine and efavirenz are about equally effective, delavirdine hardly plays a role in therapy and is not (yet) approved in Germany. Another NNRTI is etravirine .
As a single substance, NNRTIs only show a limited effect; in combination therapy with two NRTIs, they are equivalent to HIV protease inhibitors from an immunological and virological point of view. So far, no study has shown that survival time has improved and the disease progresses more slowly than with HAART. However, an improvement in the quality of life has been described. Only studies on improved CD4 + cell counts and on lower viral load were used for approval ( surrogate marker studies). Due to their good tolerance and the lower number of pills, they are often preferred to HIV protease inhibitors. NNRTIs are quite sensitive: a point mutation is enough to make the virus resistant to the active substance. There are also cross-resistances: If a virus shows resistance to an NNRTI, all NNRTIs are usually ineffective. NNRTIs are metabolized in the liver ( cytochrome P450 system).
The side effect profiles of the individual active ingredients differ considerably. In therapy with nevirapine, the main focus is on allergic reactions and liver toxicity. A rash occurs in up to 20% of patients and 7% stop taking nevirapine. To reduce the risk of allergies, nevirapine is given in low doses at the start of therapy. Then the dose is gradually increased. Liver toxicity is a rare but potentially life-threatening side effect of nevirapine. The liver values (especially the transaminases ) should therefore be monitored closely at the start of therapy .
The side effects of efavirenz, however, mainly affect the central nervous system . They usually appear at the beginning of therapy and then weaken. During the first four weeks of a study, two-thirds of the patients experienced dizziness , nearly half had nightmares, and about one-third of the patients experienced drowsiness and insomnia. However, these usually decreased after a while. While nevirapine is used to prevent mother-to-child transmission ( PMTCT ), efavirenz is contraindicated in pregnancy . In view of the effect on the central nervous system, roadworthiness is questionable. One advantage of efavirenz over nevirapine is its lower liver toxicity.
Delavirdine is inferior to the other active ingredients because of the high number of pills and the three times daily intake. In addition, it is currently not approved for the German market.
Protease inhibitors (PI)
If the HIV enzyme HIV protease cannot cleave the viral macromolecule gag-pol polyprotein, non -infectious virus particles are produced. HIV protease inhibitors (such as atazanavir , darunavir , fosamprenavir , indinavir , nelfinavir , saquinavir and tipranavir ) were modeled with knowledge of the molecular structure of the enzyme so that they can bind directly to the active site of the protease. The effectiveness of HIV protease inhibitors has been demonstrated using clinical endpoints. They have contributed to a significant improvement in therapy. In long-term treatment, however, there are some problems that lead to disorders in lipid metabolism and as a result can trigger lipodystrophy (fat distribution disorders ) and dyslipidemia (increased blood lipid levels). The reason is probably mitochondrial toxicity, since HIV protease inhibitors appear to damage the mitochondria similar to NRTIs. Other side effects are gastrointestinal complaints.
The breakdown of the HIV protease inhibitors takes place in the liver by the cytochrome P450 enzyme system. The HIV protease inhibitor ritonavir (RTV) blocks this system. The use of other protease inhibitors with ritonavir was therefore adopted in order to slow down the breakdown and increase the plasma half-life. This is known as a "booster". The HIV protease inhibitor lopinavir (LPV / r) combined with a booster dose of ritonavir is now available . This leads to an almost 100-fold higher plasma concentration of lopinavir and a higher barrier to resistance. Therefore, Lopinavir / Ritonavir (trade name Kaletra ) is mostly used after therapy failure of other drugs ("salvage area").
Another problem is the interaction of HIV protease inhibitors with many other substances: on the one hand via the cytochrome P450 enzyme system with ingredients of grapefruit, on the other hand there is a mutual interaction (both mutual weakening and mutual reinforcement) to estrogen, which at the same time Use of HIV protease inhibitors and hormonal contraceptives prevented.
Entry inhibitors
Entry inhibitors interrupt the entry of the virus into the host cell.
Fusion Inhibitors (FI)
At the beginning of 2003 the first fusion inhibitor enfuvirtide (ENF, developed under the name T-20 ) was brought onto the market. T-20 binds to the transmembrane protein gp41, which is important for the fusion of the virus with the cell membrane of the T helper cells, and thus blocks the entry of the virus into the cell. The substance is particularly interesting because it does not trigger any mitochondrial toxicity and thus no lipodystrophy syndrome.
With its 36 amino acids, T-20 is too large to be taken orally. In its current form, T-20 must be injected subcutaneously or administered via an infusion pump daily. As a side effect, skin irritation at the puncture site often occurs.
Initial studies have shown that simply adding T-20 to classic antiretroviral therapy has only limited success. However, two large studies comparing T-20 to an optimized HAART versus an optimized HAART without T-20 showed significantly better values in the T-20 arm of the study. This suggests that T-20 will particularly benefit those patients who have other drug options.
T-20 can apparently lead to interactions with granulocytes that lead to increased infections in some patients.
It is also very likely that the virus will develop resistance quickly. However, the viral adaptability to the human host of the resistant strains appears to be reduced.
Nevertheless, T-20 gives patients who have to change their therapy due to side effects or resistance an option. However, T-20 is not the first choice at the start of therapy, and not only because of the study situation. According to the manufacturer F. Hoffmann-La Roche AG, T-20 is one of the most complex substances in the company's history to produce. This is reflected in the price, which at over 24,000 euros per year is higher than a few triple combinations of conventional antiretroviral drugs.
Furthermore, since spring 2007 there has been Maraviroc (MVC) in the Expanded Access program for the final treatment of HIV patients who otherwise no longer have any treatment options.
Research is being conducted into other fusion inhibitors and a weekly T-20 injection.
Integrase inhibitors (II)
After many failures and difficulties in the 1990s, the development of integrase inhibitors began to pick up speed in 2000 . It was then that the principle of strand transfer inhibition was revealed. Clinical studies have been making rapid progress since 2005, and integrase inhibitors are the next new group of substances in HIV therapy at the latest after the first data from the phase III studies on raltegravir (MK-0518). MK-0518 is now approved in the Expanded Access program, i.e. for the final treatment of HIV patients who otherwise no longer have any treatment options.
CCR5 coreceptor inhibitors (CCR5I)
- Maraviroc (see above)
Monoclonal antibody
In March 2018, the FDA approved the first HIV-1 inhibitor and long-acting monoclonal antibody Ibalizumab-uiyk ( Trogarzo ; manufacturer TaiMed Biologics , Taiwan and Theratechnologies , Canada) for the treatment of patients who are "multi-resistant" to treatment with all of the above treatment regimens are. The FDA approved the filing for “ Fast Track ”, “ Priority Review ” and “ Breakthrough Therapy ”. Trogarzo also received Orphan Drug Status, which provides incentives to support and encourage the development of drugs against rare diseases.
Experimental therapies
Maturation inhibitors
Maturation inhibitors ("maturation inhibitors ") inhibit the budding of new virions . As with the integrase inhibitors, an antiretroviral effect was demonstrated in vivo for the first time in 2005. Bevirimat (PA-457) is a derivative of betulinic acid , as triterpene - carboxylic acid from birch or - plane bark is isolatable and as cytostatic to melanoma is used. PA-457 inhibits the budding or maturation of new virions. Phase IIa studies have already been published. Phase IIb studies are slow due to unexpected difficulties in finding the dose.
Tre recombinase
Researchers at the Hamburg Heinrich Pette Institute, Leibniz Institute for Experimental Virology and the Max Planck Institute for Molecular Cell Biology and Genetics in Dresden are working with the promising approach of specifically cutting the HIV genome out of the DNA of infected host cells and thus the infection to undo these cells. To do this, they have developed a special enzyme - Tre recombinase - that acts as a “gene scissors”. The enzyme is only activated in the presence of the proviral DNA, i.e. only in infected cells. After several promising experiments in vitro , the scientists succeeded in 2013 in freeing HIV-infected “humanized” mice from HIV and thereby “healing” them. However, these transgenic mice carried the gene for the Tre recombinase in their genome from the start. Whether an efficient therapy for HIV infections or a cure can be developed with the help of Tre recombinase cannot yet be assessed. The researchers hope to be able to investigate the effectiveness of Tre recombinase in humans as part of a clinical study in the near future .
Monoclonal antibodies
A single dose of a cocktail with multiple antibodies was effective for an average of 56 days in infected rhesus monkeys. Some animals stayed healthy afterwards.
Stem cell transplant
In early 2013, a paper gave hope for a cure, which showed that long-term virus reduction followed by haematopoietic stem cell therapy could perhaps completely remove the HIV virus. This seemed to work for the time being, but both patients treated in this way in Boston suffered a relapse after a few weeks of being virus-free and now have to be treated again with antiretroviral. While the American Timothy Ray Brown , who also received a stem cell transplant, is still the first cured AIDS patient to this day.
Gene therapy
By partially removing the coreceptor CCR5 from the genome of CD4-positive T-cells with an adoptive cell transfer and genome editing , the decrease in the concentration of CD4-positive T-cells can be slowed down.
prevention
Prevention is the most effective measure against HIV. In general, contact with foreign blood and semen should be avoided. Through the use of condoms (also Femidomen and leak towels ), sterile needles when taking drugs , the piercing piercings , tattoos and other bloody methods of body modification as well as in the medical field as well as strict control of blood as part of donated blood can be a Avoid infection very safely. Caution is also advised with methods that cause sores in the field of BDSM . In 2004, UNESCO launched EDUCAIDS, a global public education program. Pre-exposure prophylaxis (PrEP) is also used successfully as a preventive measure in which HIV-negative people take preventive medication from antiretroviral HIV therapy to protect themselves from possible HIV infection. After an event with a risk of infection, the probability of infection can be reduced if so-called post - exposure prophylaxis is carried out.
A sufficiently effective HIV vaccine does not yet exist. Many years of research into vaccines that should promote the formation of protective antibodies against the surface protein gp120 have so far failed because of the high mutation rate of the HI virus. When the agent was successfully tested against the very similar SIV (SI virus, simian immunodeficiency virus) in monkeys, the HI virus had changed the structure of its gp120 surface protein in the wild.
Prophylaxis of opportunistic infections
The indication for primary prophylaxis of opportunistic infections is dependent on the extent of immunosuppression . CD4 thresholds above which certain HIV-associated diseases are unlikely:
- below 50 / µl: CMV retinitis, cryptosporidiosis and atypical mycobacteriosis ( MOTT )
- below 100 / µl cerebral toxoplasmopsis, HIV encephalopathy, cryptococcosis and miliary tuberculosis
- below 250 / µl Pneumocystis jiroveci pneumon, thrush esophagitis and progressive multifocal leukoencephalopathy
- below 350 / µl zoster due to herpes zoster virus, ulcers due to herpes simplex virus (HSV) and oral thrush
- without limit of threshold: Kaposi's sarcoma, pulmonary tuberculosis and bacterial pneumonia.
In contrast to the CD4 cell count dependent primary prophylaxis a done Sekundärprophyaxe or post-exposure prophylaxis (see also post-exposure prophylaxis ) as maintenance therapy after already made this disease:
- Administration of cotrimoxazole to the lungs (pneumonia) by Pneumocystis jirovecii (PCP) and toxoplasmosis
- Isoniazid (INH) in patients at risk after tuberculosis
- Azithromycin after atypical mycobacteriosis
- Pneumococcal vaccination after bacterial pneumonia
- Exposure prophylaxis after illness due to cryptosporidia (avoiding drinking tap water)
- No primary prophylaxis recommended (status: 2009) after CMV retinitis, candidiasis, HSV , varicella-zoster virus and cryptococci
Epidemiology
The prevalence worldwide is 0.0059, in Germany 0.0007, in Austria 0.0011 (as of 2006).
Generally
| year | People living with HIV | New infections | Deaths | People under therapy | source |
|---|---|---|---|---|---|
| 2000 | 28.9 million | 3.2 million | 1.5 million | 0.8 million | |
| 2005 | 31.8 million | 2.5 million | 2.0 million | 2.2 million | |
| 2010 | 33.3 million | 2.2 million | 1.5 million | 7.5 million | |
| 2011 | 33.9 million | 2.2 million | 1.4 million | 9.1 million | |
| 2012 | 34.5 million | 2.2 million | 1.4 million | 11 million | |
| 2013 | 35.2 million | 2.1 million | 1.3 million | 13 million | |
| 2014 | 35.9 million | 2.1 million | 1.2 million | 15 million | |
| 2015 | 36.7 million | 2.1 million | 1.1 million | 17 million | |
| 2016 | 36.7 million | 1.8 million | 1.0 million | 20.9 million | |
| 2017 | 36.9 million | 1.8 million | 0.9 million | 20.9 million | |
| 2018 | 37.9 million | 1.7 million | 0.77 million | 23.3 million | |
| 2019 | 38.0 million | 1.7 million | 0.69 million | 25.4 million |
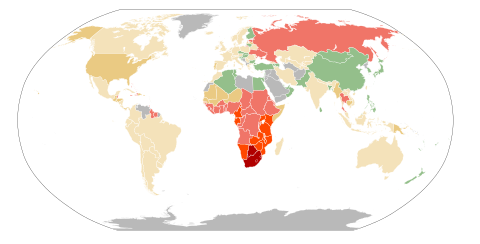
From an epidemiological point of view, the worldwide distribution pattern of HIV and its uneven spread was unusual in contrast to most other viruses.
The first HIV virus discovered was HIV-1, subtype B from the main group M. This virus first appeared in Central Africa around 1925. After genetic analyzes of numerous HIV subtypes from around the world, an international team of researchers came to the conclusion that this virus reached Haiti from Africa around 1966 . The studies also show that there is a high probability that the virus first spread within Haiti and then from there across the world. It reached the USA from Haiti in 1969, which could be traced back to virus samples from the first known AIDS patients from Haiti. In the USA, the virus initially spread very slowly in the heterosexual population, before it spread a little later within the high-risk group of homosexual men.
While the HIV epidemic began in the US as early as the 1980s, there were a few countries that seemed spared from HIV, but were quickly taken over by the virus. This is what happened particularly in Eastern Europe and Asia in the mid-1990s. In other countries, for example Cameroon , the prevalence of HIV remained stable for years and then skyrocketed. There also does not seem to be an upper limit for HIV prevalence. After 1997 , the rate of pregnant women with HIV in urban centers in Botswana rose from 38.5 to 55.6% in four years.
A sustainable and successful fight against HIV / AIDS in African high-prevalence countries must include the reduction of both AIDS-related deaths and new infections. Data from some countries hard hit by the HIV epidemic, such as Kenya, Rwanda, Uganda and Zimbabwe, show that various measures can reduce the rate of new infections. The foundations of this success are the nationwide introduction of sex education classes, the increasing introduction of antiretroviral therapy, nationwide campaigns to increase the acceptance of condoms, HIV tests, the results of which are announced on the same day, and self-help kits for sexually transmitted diseases . However, these successes can only be achieved with financial means that many of the high-endemic countries in Africa cannot raise on their own. Political will to actively combat this epidemic is also essential.
According to data from Uganda, the prevalence of HIV among pregnant women was reduced from almost 30% in 1992 to 5.4% in 2007. Uganda's success story is not without controversy: Improved data collection and the dramatic mortality rate among people with HIV / AIDS have also contributed to the reduction in HIV prevalence. In Zimbabwe, the prevalence decreased from 29% (1997) to 16% (2007). An interdisciplinary UNAIDS study concluded that the main causal factor was a change in sexual behavior, which led to a significant reduction in the number of sexual partners through a reduction in extramarital, commercial and occasional sex.
Worldwide
As before, this is southern Africa most affected by the epidemic. In 2012, 70% of all new HIV infections among adults took place here. However, it turns out that the education and prevention programs are successful. Between 2001 and 2012, the annual new HIV infections in southern Africa decreased by 34%. Worldwide, new HIV infections fell by 50% or more in the period 2001 to 2012 in 26 countries, including Ethiopia, Ghana, India, Thailand and the Ukraine. On the other hand, an increase in new infections has been recorded in Eastern Europe and Central Asia as well as the Middle East and North Africa. The country with the highest HIV rate in the world is Swaziland , where 26.5% of adults (15 to 49 years old) were infected with HIV in 2012.
Germany
| Statistical size | number |
|---|---|
| HIV-infected people | 87,900 |
| Including men | 70,600 (80%) |
| Including women | 17,300 (20%) |
| Distribution according to risk of infection | |
| Men who have sex with men | 54,200 (73.5%) |
| Heterosexually infected people | 10,900 (14.8%) |
| Intravenous drug users | 8,200 (11.1%) |
| Infected by blood products | 450 (0.6%) |
| New infections in 2018 | |
| total | 2,400 |
| Including men | 2,000 (80%) |
| Including women | 400 (20%) |
| AIDS deaths | |
| Since the epidemic began | 29,200 |
| In 2018 | 440 |
| Medical care 2018 | |
| Estimated number of people who are not aware of their HIV infection |
10,600 (5%) |
| HIV-infected people on antiretroviral therapy | 87,900 (93%) |
| Source: Epidemiological Bulletin Robert Koch Institute 2019 | |
In 1986 the number of new HIV infections peaked at just under 6,000.
In 1987, for example, in the fight against the spread of the HI virus , the Bavarian state government considered a legislative initiative to tighten the Federal Disease Act with compulsory tests for applicants for the public service and prisoners, the expulsion of HIV-positive foreigners and the quarantine of infected people “In special homes”.
In the 1990s there were around 2,000 new HIV infections per year. From 2000 to 2005, the number of new infections rose steadily every year, especially in men who have sex with men (MSM). Since 2005, the annual new infections seem to have stabilized at a value of around 3000. In Germany, AIDS is one of the insignificant causes of death in comparison with other causes of death with around 460 deaths per year . According to data from the Robert Koch Institute (RKI), a total of around 28,100 people in Germany succumbed to the consequences of immune deficiency by the end of 2015. In 2015, an estimated 84,700 people in Germany (approx. One person in 1,000) were infected with HIV. The incidence of new infections varies greatly from region to region. In large cities (Berlin, Cologne, Hamburg, Stuttgart, Frankfurt am Main) it was between 10 and 13 / 100,000 inhabitants in 2012, while it was significantly lower in rural areas. However, an analysis of the number of reports since 2000 shows that, especially under MSM, the number of reports outside of the big cities has increased more than reports from the big cities and that the numbers are slowly converging. According to the RKI, 10 to 12 percent of MSM in large cities are HIV-positive.
According to estimates by the RKI, around 82% of the approximately 3,200 newly infected people in 2015 were men. 64% of those newly infected are men who have sex with men; About 13% of the transmissions came from heterosexual intercourse (and the trend is rising), 9% of the infections from infected syringes during intravenous drug use and less than 1% from mother to child during pregnancy and childbirth. According to estimates, the number of as yet undiagnosed HIV-positive people in Germany is around 12,600. The risk of infection for men who have sex with men is significantly higher than with unprotected intercourse in heterosexual couples. The disease affects all social groups and social classes.
The data on the spread of HIV and AIDS determined by the RKI can only be compared to a limited extent with previously published estimates, as additional data and information as well as the adaptation of the survey methodology change the calculations from year to year. The RKI therefore adapts the annual evaluation of the changing data situation and interpolates, for example, data from the early days of the HIV epidemic in order to make an overall trend visible.
The continued rise in other sexually transmitted diseases remains a cause for concern . Not only does this increase the risk of HIV infection, it also shows that the acceptance of condoms is declining and that the preventive measures of the past decades are obviously losing their effectiveness.
Austria
At the beginning of 2008 there were around 12,000 to 15,000 HIV-infected people in Austria, around half of them in Vienna . The number of new infections has been around 450 per year since 2003 (2015: 428). The lowest rate was in 1997 with 297, the highest in 1993 with 561 new infections. The number of new infections has now remained relatively constant. Between 1983 and May 5, 2008, 2608 people in Austria fell ill with AIDS and 1,468 died. From 2003, with 50 new diseases, they rose to 65 in 2004.
In 2006 almost 42% of new infections occurred through heterosexual contact (in 1998 it was 27%), 28.6% through homosexual contact and 20.5% through intravenous drug use.
Around one million HIV antibody tests are carried out in Austria every year (500,000 of which are financed by donations). One problem is that the tests are often carried out in the wrong target group (retirees). On the one hand, a lot of tests are carried out, on the other hand, many of those affected only become aware of the HIV infection in the course of the actual illness.
Switzerland
In 2014, 519 positive HIV tests were reported in Switzerland. Since 2008 there has been a continuous, slightly decreasing trend in the number of HIV diagnoses. The cantons of Zurich , Vaud and Geneva are particularly hard hit .
In 2014, 50% of infections occurred in men who have sex with men. The number of infections after heterosexual intercourse follows with 39.1%. Infections after drug use are falling continuously and are at 1.6%.
In men (both homosexual and heterosexual), HIV infection occurred more often during casual sex than during sex with a steady partner. In contrast, women were mostly infected in a steady partnership. Accordingly, a stable partnership does not necessarily protect against HIV.
Africa
The HIV / AIDS pandemic is at its worst south of the Sahara . 24.7 million people live here with HIV infection (around one in twenty adults is infected). The main modes of transmission of HIV differ fundamentally from those in Europe and North America: Heterosexual intercourse is by far the most common mode of transmission in Africa, accounting for around 50% of HIV infections. Another 5 to 10% of infections come from infected blood transfusions. The transmission of the virus from HIV-positive, pregnant women to their newborns during pregnancy, childbirth and breastfeeding is another route of infection. In some countries, the immune deficiency had reduced life expectancy by more than ten years. The situation has since improved. In 2013, around half of those infected south of the Sahara knew their HIV status. Of these, 87% received antiretroviral therapy.
There seem to be some factors that favor the spread of the HIV virus: While in Europe and North America shortly after the discovery of the HIV virus, the mass media informed large parts of the population with information campaigns about the deadly dangers of HIV infection and prevention, AIDS remained a taboo subject in many parts of Africa. This gave the HI virus almost twenty years more time to spread unhindered.
Successor states to the Soviet Union
The first HIV infections in the Soviet Union were not registered until the late 1980s. An epidemic spread began in the early 1990s, initially almost exclusively among injectable drug users. The main route of infection was the common use of syringes. With drug addiction spreading after the collapse of the Soviet Union, so did the number of HIV infections.
To this day, when, depending on the region, up to 60% of new infections occur sexually, their emergence in the drug environment has shaped the appearance of the HIV epidemic in the successor states of the Soviet Union. The Ukraine is the worst affected and, in terms of the characteristics of the epidemic, exemplary for many regions of the former Soviet Union .
history
Theories of origin
The simian immunodeficiency virus (SIV) , which occurs in monkey species, is almost identical to the human HI virus . It is believed to have existed for at least 32,000 to 75,000 years, as was determined by comparing samples taken from the island of Bioko in the Gulf of Guinea off Africa and from mainland Africa . A distinction is mainly made between the African SIVcpz (from chimpanzee ), from which HIV-1 is derived, and the Asian SIVmac (from macaque ), from which the rarer HIV-2 is derived.
Genetic analyzes by virologists at the University of Alabama at Birmingham in 2003 show that SIVcpz is a combination of two strains of the virus found in monkeys and collared monkeys. Because these species of chimpanzees are hunted and eaten, the chimpanzees may have become infected with the two strains of the virus that could then have formed the SI virus in their bodies.
According to the researchers, this SI virus was transmitted to humans as early as the 1930s through injuries caused by hunting or eating by chimpanzees, although there are indications that this happened earlier in isolated cases. Further scientific investigations showed that the HI virus first appeared in West Africa, but it has not been established with absolute certainty whether there were several virus foci. New phylogenetic studies, i.e. comparisons between the different subtypes of HIV and between HIV and SIV, suggest that several independent transmissions from chimpanzees to humans took place in Cameroon and / or its neighboring countries.
The oldest blood sample known to contain HIV antibodies was taken from an adult man in the Congo in 1959 . However, the authenticity of this sample has not been clarified with certainty. HIV genes were found in old paraffin DNA samples in a woman who died in the Congo (1960, lymph node tissue), an American adolescent (1969) and a Norwegian sailor (1976).
Conspiracy theory
In addition to the currently accepted theory, in the context of the disinformation campaign “ Infection ” directed against the USA, the KGB spread the claim that a new type of virus had been discovered by US researchers looking for suitable pathogens for biological warfare in Africa, in the US military laboratory Fort Detrick increased and examined, and eventually escaped.
From 1985 onwards, Jakob Segal developed a scientifically based hypothesis of an artificial HIV origin .
First infections
The earliest documented infection with HIV-1 was found in blood samples taken in 1959 from a man from Léopoldville ( Belgian Congo ). A comparison with later samples from a family of a Norwegian sailor who died of AIDS in 1976 suggests divergence from a common ancestor from the 1940s to the early 1950s. It is believed that HIV-1 leaked to humans a few years earlier. However, the genetic difference between HIV-1 and HIV-2 also suggests that these subtypes diverged much earlier. The geneticist Bette Korber of Los Alamos National Laboratory dated the first transmission to around 1931 in 2000 using the sample from 1959. The evolutionary biologist Michael Worobey of the University of Arizona dated the in 2008 using an additional sample from 1960 first transmission to the period between 1884 and 1924. He suspects that the establishment of the colonial cities helped the virus to gain a foothold.
First descriptions of diseases
In 1981 Michael S. Gottlieb described an accumulation of a rare form of pneumonia in the June 5 issue of the Morbidity and Mortality Weekly Report , a weekly bulletin for the CDC . This form, triggered by the fungus Pneumocystis jirovecii , almost exclusively affects patients with severe immunodeficiency, but was found by Gottlieb in five previously healthy, homosexual men in Los Angeles. Similar reports from other US cities followed. In addition, other opportunistic diseases - such as Kaposi's sarcomas - were increasingly found, which predominantly affect patients with a weakened immune system.
Acquired immunodeficiency disease that can be sexually transmitted was considered a likely cause early on. Initially there was no official name and the names of the diseases were often referred to, such as lymphadenopathy or Kaposi's sarcoma , sometimes with a reference to homosexual men; the CDC 's task force was named Kaposi's Sarcoma and Opportunistic Infections , which was also used for reporting. From May 1981, the general press wrote about Gay Related Immune Deficiency (GRID) or Gay People's Immuno Deficiency Syndrome (GIDS) , among others . However, further epidemiological studies in the USA showed that the disease also occurred among haemophiles , recipients of blood (for example through blood transfusions ) and heterosexual drug addicts, which suggests parenteral transmission as well as sexual . Looking for a name, the CDC also created the "the 4H disease" name, referring to the alleged main affected groups: H aitianer , H omosexuelle, H ämophile and H eroin addicts. On July 27, 1982 a conference agreed on the descriptive name Acquired Immune Deficiency Syndrome and the abbreviation AIDS, which was used from August 1982 and from September 1982 at the CDC and in the French-speaking area as "Syndrome d'Immuno-Déficience" Acquise ”(SIDA) appears.
In Germany, the Spiegel reported for the first time on May 31, 1982 under the title The shock from over there , and the disease was first diagnosed in July 1982 in a patient from Frankfurt am Main. In Austria, the first two cases were reported in April 1983, and the Austrian daily newspapers reported for the first time in the spring of 1983 on the occasion of the first death. Many media reported in lurid tones; the mirror characterized the disease as a "gay disease" or "Schwulenpest". As a result, HOSI Vienna, together with Klaus Wolff and Christian Kunz, created an information sheet aimed at gay men and published it together with the “Vienna Working Group for Public Health”. It was the first AIDS information brochure in Europe.
Isolation of the virus and first therapies
In 1983, a French research group led by Françoise Barré-Sinoussi and Luc Montagnier isolated a previously unknown retrovirus , the lymphadenopathy virus (LAV), which they suspected to be the cause of AIDS. A causal relationship between the virus and the immunodeficiency disease was alleged a short time later. In 1984 a virus discovered in AIDS patients was named Human T-cell Lymphotropic Virus-III (HTLV-III) at the US Cancer Institute . In March 1985, based on further reports on LAV and HTLV-III, it turned out that these are identical. In 1985, Robert Gallo received the US patent for the first ELISA antibody test, which was approved by the US regulatory authority. In 1986 the name Human Immunodeficiency Virus (HIV) was established for the virus . A year later, in 1987, AZT (Retrovir), the first therapeutic agent, was approved. In 1989, pentamidine inhalation was introduced for the prophylaxis of Pneumocystis pneumonia in HIV patients .
In January 1982, Gay Men's Health Crisis (GMHC) was founded, the oldest organization to help people with AIDS in New York City . In 1983 the AIDS-Hilfe was founded in Berlin , followed by the one in Vienna and the AIDS-Hilfe Schweiz in 1985 . In the same year the first world AIDS conference took place in Atlanta (USA) , and with Rock Hudson the first world star died as a result of immunodeficiency. The activist political initiative Act Up split off from the GMHC in March 1987 .
When a question about AIDS was asked at a routine press conference at the White House on October 15, 1982 , the subject was ridiculed. The then US President Ronald Reagan found official words for the first time in May 1987 at the 3rd International AIDS Conference in Washington. Elizabeth Taylor had previously written him a pleading letter to help break the archaic stigma ("disease of homosexuals"). By then, 36,058 US citizens had been diagnosed, 20,849 had died from the consequences, and the infection had been found in 113 countries.
In 1985, Norman L. Letvin established the first non-human primate model for research into HIV, after he had succeeded in isolating the simian immunodeficiency virus (SIV) and demonstrating that there was AIDS-like damage to the immune system and in Indian rhesus monkeys Causes deaths.
The WHO Global Program on HIV / AIDS has been active since 1987 , from which UNAIDS emerged in 1996 . In 1988, December 1st was declared World AIDS Day by the WHO . The successor US President Bill Clinton declared AIDS an "enemy of the state" in 2000 because the epidemic could topple governments, cause chaos in the global economy and spark ethnic conflicts.
Social development
In the beginning, the disease was seen by the public as a problem of “fringe groups” like homosexuals and drug addicts. However, this changed dramatically with the advent of HIV testing. Because even people without clinical symptoms had antibodies, which indicated a symptom-free latency period of several years, during which the virus may also have been passed on. In 1984, research found that AIDS was equally prevalent among men and women in Kinshasa , regardless of drug use and blood transfusions.
In the USA it was reported in 1985 that the infection rate of the wives was 70% in the case of hemophilia patients ("hemophiliacs") examined who were infected by stored blood. The realization that the risk of infection in heterosexual intercourse seemed to be significantly higher than initially assumed, led to a great deal of public interest. The combination of the now known infection routes and the long latency period allowed epidemiological projections to paint a pessimistic picture.
In 1987, the Federal Office for Health Education launched a large-scale media awareness campaign in Germany with the slogan Don't give AIDS a chance . The best known was a commercial from 1989 with Hella von Sinnen as the cashier, who shouted loudly across the shop: “Tina, what do the condoms cost?” When the customer embodied by Ingolf Lück wanted to buy them.
The annual doubling of new cases in Germany only lasted from 1984 to 1987, after which the increase in the number of sick people was less steep until the numbers leveled off at around 2000 in 1993. This quickly changed public interest in HIV / AIDS. In 2015, around 2.1 million people worldwide were newly infected with the virus, and around 1.1 million people died of it in the same year.
Red ribbon becomes symbol of fight against AIDS
In 1990 the Red Ribbon was established at the AIDS conference in San Francisco to protest against discrimination against HIV-infected people. A year later, the red ribbon became an international symbol for the fight against AIDS. In 1992 the World AIDS Congress was relocated from Boston to Amsterdam due to US entry requirements. In addition, the remaining Queen members established the Mercury Phoenix Trust in memory of Freddie Mercury .
Changes after introducing the PCR test for HIV
In 1994 the HIV- PCR was established as an important diagnostic test for the therapy control of the course of the infection. The following year, 1995, the first HIV protease inhibitor, saquinavir, was launched in the United States. The following year, nevirapine was approved as the first non-nucleoside reverse transcriptase inhibitor. Because of the intensive combination therapy, the death rate in the USA dropped dramatically in 1997. In 2003, enfuvirtide (Fuzeon), the first fusion inhibitor, was approved in the USA. In 2004, the WHO started the 3 by 5 initiative: In 2005, three million infected people were to be provided with medication.
Different theses
Despite reliable scientific knowledge, a very small number of scientists deny either the existence of HIV or the connection between HIV and AIDS. These include in particular the German-American retrovirologist Peter Duesberg and the chemist Kary Mullis . Her theses influenced the former President of South Africa , Thabo Mbeki , who appointed Duesberg to the South African AIDS Advisory Commission in 2001. In South Africa in 2001 about 15.3% of the population was infected with HIV / AIDS and about 200,000 people died of AIDS in the same year. Kary Mullis is known for the discovery of the PCR process, for which he received the Nobel Prize in Chemistry and which, among other things, is used to detect HI viruses in the body of those affected. However, he has never researched HIV or AIDS himself. But after he described himself as a possible victim of alien abduction and expressed his fondness for astrology , his reputation as a scientist suffered greatly.
The position of the AIDS deniers is categorized and sharply criticized by the overwhelming majority of medical professionals and scientists as a dangerous conspiracy theory. The Robert Koch Institute also commented on these positions. In South Africa , the introduction of HIV therapy was delayed until 2004 because of a health policy characterized by the denial of the link between HIV and AIDS. It is believed that at least 330,000 people died prematurely from AIDS between 2000 and 2005 as a result of this policy and that due to a lack of HIV infection prevention, 35,000 newborns were infected with HIV.
Socio-ethical assessment
The disease syndrome AIDS has developed into a serious challenge worldwide for those directly affected, medicine, science, but also for all those who care for or live with sick people.
Far from any stigmatization of AIDS-ill patients (see: Discrimination against people with HIV / AIDS ), it is important to find ways and means to help them more effectively: be it through therapeutic measures that are still not available , be it in the sense of symptomatic therapy and palliative medicine . Comprehensive and effective prevention is also required .
The search for an ethically justifiable strategy to combat HIV / AIDS leads to partially contrary results: some emphasize the absolute necessity of an exclusively or primarily "technical" protection against the spread of the disease. Others see this answer as inadequate or reject it for reasons of religious ethics. They re-emphasize the value of permanent marital fidelity or, in specific cases, also demand temporary or complete abstinence . The propagation of condoms as protection against AIDS is questionable from a religious-Christian point of view. It has been argued that this promotes an irresponsible lifestyle associated with promiscuity and certain sexual practices, which puts you and others at risk. These demands are, however, to be seen in the context of the moral teaching that is widespread, particularly in the Catholic Church, which has negative connotations for promiscuity. Since the Catholic Church had considerable social influence during the spread of AIDS in Africa, numerous new infections have been accepted due to the years of hindrance to education and prevention (such as sex education in schools and the distribution of condoms). In the interview book Licht der Welt , published in 2010, the head of the Roman Catholic Church Pope Benedict XVI. that he sees the use of condoms "of course not as a real and moral solution". A justified individual case for an exception to this attitude could be that male prostitutes use a condom. This could then be “a first step towards a moralization” and help to develop an awareness that “everything is not permitted and you cannot do everything you want”. In principle, however, the Pope continued to reject the use of condoms in the fight against the global epidemic.
HIV-positive and AIDS-infected people are often exposed to stigmatization and discrimination. A study by Deutsche AIDS-Hilfe 2012 came to the result that 77% of the more than 1,100 HIV-positive people questioned were discriminated against in the year before the survey - from gossip to insults to physical attacks. More positive people lost their jobs because of discrimination than for health reasons. Dismissals were related to discrimination in 84% of the cases. Around 20% of those questioned were refused medical treatment due to HIV in the year before the survey (for example at the dentist). Apart from open rejection, HIV patients repeatedly report delayed appointments, separate treatment times or discrimination e.g. B. with reference to labor-intensive hygiene guidelines. However, the German AIDS Society (DAIG e.V.) and the German Association of Resident Doctors in the Care of HIV-Infected Persons (DAGNÄ) emphasize that the dental treatment of HIV-infected persons does not require any hygienic requirements that go beyond the standard measures. are necessary to prevent transmission of HIV.
In Austria in particular, the term “social AIDS” has been used to describe the discrimination against HIV-positive people. Even doctors who are principally obliged to treat refuse treatment in individual cases (“[…] I have no desire to expose myself to such a danger […]”). In Hanau and the Main-Kinzig district , a survey with telephone contact and questionnaire was started, but with little response. Practice employees didn't know what to do with the terms HIV and AIDS. The main reason for rejection was the alleged higher hygiene requirements in the treatment of people with HIV. In a practice, it is generally necessary to work so hygienically that there is no risk of transmission there. About 16% of HIV-positive people in Germany are not yet aware of their infection. The AIDS organizations and other organizations want to raise awareness of the issue throughout the year . Even the World AIDS Day on December 1, is used to and the now internationally acclaimed Life Ball in Vienna will not only raise funds but to fight on the media coverage with positive slogans against stigmatization.
See also
literature
Guidelines
- S2k guidelines for antiretroviral therapy of HIV infection by the German AIDS Society (DAIG). In: AWMF online (as of 2014)
- S2k guideline for antiretroviral therapy of HIV infection in children and adolescents of the German AIDS Society (DAIG). In: AWMF online (as of 2019)
- S2 guideline HIV pre-exposure prophylaxis (PrEP) of the German AIDS Society (DAIG). In: AWMF online (as of 2018)
- S2k guideline for antiretroviral therapy of HIV infection in children and adolescents of the German AIDS Society (DAIG). In: AWMF online (as of 2019)
- S2k guidelines for HIV therapy in pregnancy and in newborns exposed to HIV from the German AIDS Society (DAIG). In: AWMF online (as of 2020)
magazine
- The scientific journal AIDS Reviews appears quarterly and publishes reviews that deal with the various aspects of HIV and AIDS.
miscellaneous
chronologically
- Peter Lichtenberg and Michael Malm (editor): Aids: facts and consequences. Interim report of the study commission of the 11th German Bundestag 'Dangers of AIDS and effective ways to contain them'. Ed .: German Bundestag, Public Relations Department. Down to business. Issues of parliamentary deliberation. Vol. 3/88. Bonn 1988. ISBN 3-924521-22-0 . 283 pp.
- Birgit Adam : The punishment of Venus. A cultural history of venereal diseases. Orbis, Munich 2001, ISBN 3-572-01268-6 , here: pp. 23-25 (HIV infection / AIDS) and 205-233 (AIDS - today's epidemic of lust ?)
- Hansjoerg Dilger: Living with AIDS. Illness, Death, and Social Relations in Africa . An ethnography. Campus, Frankfurt am Main 2005, ISBN 3-593-37716-0
- Bärbel Häcker: AIDS. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 20-22.
- Allan Stratton: Which nobody talks about. Novel. , Deutscher Taschenbuch Verlag, Munich 2005, ISBN 3-423-78204-8 .
- Bartholomäus Grill, Stefan Hippler: God, Aids, Africa. The deadly silence of the Catholic Church . With a foreword by Henning Mankell. Bastei Lübbe, Bergisch Gladbach 2009, ISBN 978-3-404-60615-3
- James Chin: The AIDS Myth. Medical facts versus political correctness , translated by Cathrine Hornung, Ares Verlag , Graz 2009 ISBN 3-902475-50-1
- Susanne Roeßiger: Safe sex and solidarity. The collection of international AIDS posters in the German Hygiene Museum , in: Zeithistorische Forschungen / Studies in Contemporary History 10 (2013), pp. 502-514.
- Henning Tümmers: "GIVE AIDS NO CHANCE". A message of prevention in two German states , in: Zeithistorische Forschungen / Studies in Contemporary History 10 (2013), pp. 491–501.
- Henning Tümmers: AIDS. Autopsy of a threat in divided Germany. Wallstein Verlag, Göttingen 2017, ISBN 978-3-8353-3005-4 .
- W. David Hardy: Fundamentals of HIV Medicine 2019. Oxford 2019, [email protected] (engl.)
Web links
- German AIDS Help
- German AIDS Foundation
- Austrian AIDS Help
- AIDS Education Switzerland Information material to download
- AIDS Help Switzerland (many brochures can be downloaded)
- UNAIDS - Joint United Nations Program on HIV / AIDS (English, French, Russian, Spanish)
- German Association of Resident Doctors in the Care of HIV-Infected People (DAGNÄ e.V.) - Information, current developments and a list of established HIV specialist practices
- www.hivbuch.de - Detailed and up-to-date information on the subject of HIV and AIDS
- HIV / AIDS: key data and trends for Germany and the federal states. In: rki.de .
- Johannes Georg Gostomzyk: Acquired Immune Deficiency Syndrome (AIDS). In: Historical Lexicon of Bavaria . May 28, 2013.
- Sine Maier-Bode, Hildegard Kriwet: Aids. In: planet-wissen.de . ARD
Individual evidence
- ^ "HIV", made available by the digital dictionary of the German language , <https://www.dwds.de/wb/HIV> , accessed on March 12, 2021.
- ^ A b J. L. Marx: New disease baffles medical community . In: Science . 217, No. 4560, 1982, pp. 618-621. PMID 7089584 .
- ↑ Fact Sheet - World Aids Day 2019. (PDF; 216 kB) In: unaids.org. 2019, accessed on May 22, 2020 .
- ↑ a b c UNAIDS : UNAIDS Report on the global AIDS epidemic 2013 . ( PDF; 1.4 MB [accessed January 30, 2014]).
- ↑ a b UNAIDS : 2008 Report on the global AIDS epidemic . ( PDF; 2.2 MB [accessed December 22, 2008]).
- ↑ a b Revised Surveillance Case Definitions for HIV Infection Among Adults, Adolescents, and Children Aged <18 Months and for HIV Infection and AIDS Among Children Aged 18 Months to <13 Years. CDC , December 5, 2008, accessed February 17, 2014 .
- ↑ 1993 Revised Classification System for HIV Infection and Expanded Surveillance Case Definition for AIDS Among Adolescents and Adults. In: cdc.gov . 1993, accessed January 14, 2020 .
- ^ AIDS-Defining Conditions. CDC , December 5, 2008, accessed February 17, 2014 .
- ↑ Decision of the Commission of March 19, 2002 amending Decision 2002/253 / EC establishing case definitions for the reporting of communicable diseases to the Community network in accordance with Decision No. 2119/98 / EC of the European Parliament and of the Council. , accessed February 17, 2014
- ^ Case definition. (No longer available online.) In: ecdc.europa.eu. Archived from the original on February 22, 2014 ; accessed on May 10, 2018 .
- ^ AIDS Surveillance in Europe, Quarterly Report 1993; No. 37. (PDF; 219 kB) WHO-EC Collaborating Center on AIDS, March 31, 1993, accessed on February 17, 2014 (English).
- ↑ a b c WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. (PDF; 1.12 MB) WHO , 2007, accessed on February 17, 2014 (English).
- ↑ a b RKI guide for doctors: HIV / AIDS. Robert Koch Institute , March 2011, accessed on January 31, 2014 .
- ↑ HIV transmission. CDC , December 14, 2015, accessed March 2, 2016 .
- ↑ CDC : Figures on the mean transmittability of HIV, per file. Accessed November 17, 2016 (English).
- ↑ a b A. Plettenberg et al .: "HIV-PEP State of the Art" . In: Federal Health Gazette - Health Research - Health Protection . 43, No. 13, 2000, pp. 18-25. doi : 10.1007 / s001030070006 .
- ↑ Study in Africa: Long Breastfeeding Reduces Risk of HIV Transmission. Spiegel Online, accessed July 1, 2014 .
- ↑ Breast milk - breastfeeding despite HIV infection. In: Focus Online . June 5, 2008, accessed July 25, 2020 .
- ↑ Breast is always best, even for HIV-positive mothers. Bulletin of the World Health Organization, pp. 1-80, Volume 88, Number 1, January 2010 , accessed July 1, 2014 .
- ↑ Gina Kolata: Hemophilia and AIDS: Silent Suffering. The New York Times, May 16, 1988, accessed November 11, 2012 .
- ↑ The history of the blood AIDS scandal in Germany. Interest group haemophiles e. V., April 4, 2011, accessed November 11, 2012 .
- ↑ Hans Harald Bräutigam, Kuno Kruse: Federal Minister of Health Horst Seehofer has caused great confusion. Is there a new AIDS threat ?: On the trail of the blood scandal. In: zeit.de . October 29, 1993. Retrieved December 26, 2014 .
- ↑ Michael K. Hourfar, Christine Jork et al .: Experience of German Red Cross blood donor services with nucleic acid testing: results of screening more than 30 million blood donations for human immunodeficiency virus-1, hepatitis C virus, and hepatitis B virus. In: transfusion. 48, 2008, p. 1558, doi: 10.1111 / j.1537-2995.2008.01718.x .
- ↑ Tips for cleaning the syringes. Aidshilfe NRW, accessed on February 2, 2014 .
- ^ Syringe Disinfection for Injection Drug Users. (PDF) CDC , July 2004, accessed February 2, 2014 .
- ↑ Female Genital Mutilation and HIV. (PDF; 177 kB) In: giz.de. January 2011, accessed July 2, 2018 .
- ↑ Country Factsheet Lesotho 2016 - HIV and AIDS Estimates. In: unaids.org. Accessed July 2, 2018 .
- ↑ Traditional Practices. In: bbc.co.uk. Retrieved July 3, 2018 .
- ↑ Prudence Phiri: Zambian Women Practice Dry Sex to Avoid Accusations of Infidelity. In: globalpressjournal.com. April 7, 2016, accessed July 5, 2018 .
- ↑ The drop of pleasure. (PDF; 424 kB) In: HIVreport 2/2011. April 28, 2011, accessed July 12, 2020 .
- ↑ Elizabeth Boskey: How HIV Is Diagnosed. In: about.com . April 21, 2020, accessed on May 13, 2020.
- ↑ Entire legal provision of the AIDS Act in the current version.
- ↑ § 2 Proof of infection and disease indicators for AIDS.
- ↑ a b F. M. Hecht et al .: Use of laboratory tests and clinical symptoms for identification of primary HIV infection. . In: AIDS . 16, No. 8, 2002, pp. 1119-1129. PMID 12004270 .
- ↑ iht.com
- ↑ Dermatology and Venereology, Fritsch, P., Springerverlag 2004, p. 913
- ↑ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , pp. 302-305 (HIV infection) , here: pp. 302 f.
- ↑ By reducing the viral load by 1–2 log10 , morbidity and mortality can be reduced. However, the incomplete lowering of the viral load leads to the selection of resistant virus mutants and there is a risk of therapy failure, which is why the initial antiretroviral therapy should lower the viral load below the detection limit (as of 2009: 20–50 HIV-RNA copies / mL). Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 302 f.
- ↑ Marianne Abele-Horn (2009), p. 304.
- ↑ Guidelines for diagnosis and treatment of HIV infection - Deutsche AIDS Gesellschaft e. V . Daignet.de. Retrieved September 9, 2010.
- ↑ German-Austrian guidelines for antiretroviral therapy of HIV-1 infection . Rki.de. March 4, 2010. Archived from the original on March 9, 2014. Retrieved on August 14, 2012.
- ↑ [email protected]: EACS - European AIDS Clinical Society . Web.archive.org. Archived from the original on May 26, 2008. Retrieved September 9, 2010.
- ↑ Guidelines: HIV. World Health Organization , March 2014, accessed March 3, 2014 .
- ↑ a b K. Brinkman et al .: Mitochondrial toxicity induced by nucleoside-analogue reverse-transcriptase inhibitors is a key factor in the pathogenesis of antiretroviral-therapy-related lipodystrophy. . In: The Lancet . 354, No. 9184, 1999, pp. 1112-1115. PMID 10509516 .
- ↑ Marianne Abele-Horn (2009), p. 303.
- ^ D. Torre et al .: Nevirapine or efavirenz combined with two nucleoside reverse transcriptase inhibitors compared to HAART: a meta-analysis of randomized clinical trials. . In: HIV Clinical Trials . 2, No. 2, 2001, pp. 113-121. PMID 11590519 .
- ↑ CR Fumaz et al .: Quality of life, emotional status, and adherence of HIV-1 infected patients treated with efavirenz versus protease inhibitor-containing regimens . In: Journal of Acquired Immune Deficiency Syndromes . 29, No. 3, 2002, pp. 244-253. PMID 11873073 .
- ↑ Marianna Abele-Horn (2009), p. 303.
- ↑ B. Duration: Protease inhibitors: the current status . In: Journal of HIV Therapy . 10, No. 4, 2005, pp. 72-74. PMID 16519246 .
- ↑ V. Oldfield, GL Plosker: Lopinavir / ritonavir: a review of its use in the management of HIV infection. . In: Drugs . 66, No. 9, 2006, pp. 1275-1299. PMID 16827606 .
- ↑ Hormones and Contraception. (No longer available online.) In: hiv-wechselektiven.de. Archived from the original on December 30, 2014 ; Retrieved September 9, 2010 .
- ↑ JP Lalezari et al .: "Enfuvirtide, an HIV-1 Fusion Inhibitor, for Drug-Resistant HIV Infection in North and South America" . In: New England Journal of Medicine . 348, No. 22, 2003, pp. 2175-2185. PMID 12637625 .
- ↑ DJ Hazuda, P. Felock, M. Witmer et al .: Inhibitors of strand transfer that prevent integration and inhibit HIV-1 replication in cells. In: Science , 2000, 287, pp. 646-650, PMID 10649997 .
- ↑ D Cooper, J Gatell, J Rockstroh et al .: Results of BENCHMRK-1, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus . Abstract 105aLB, 14th CROI 2007, Los Angeles. Abstract ( Memento from March 30, 2007 in the Internet Archive )
- ↑ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 303.
- ↑ FDA approves new HIV treatment for patients who have limited treatment options. In: fda.gov. March 6, 2018, accessed May 21, 2019 .
- ↑ Theratechnologies Announces FDA Approval of Breakthrough Therapy, Trogarzo ™ (ibalizumab-uiyk) Injection, the First HIV-1 Inhibitor and Long-Acting Monoclonal Antibody for Multidrug Resistant HIV-1. Theratechnologies press release. In: prnewswire . March 6, 2018, accessed May 4, 2020.
- ↑ FDA approves new HIV treatment for patients who have limited treatment options , PM TaiMed, March 7, 2018, accessed March 15, 2018.
- ↑ F. Li, R. Goila-Gaur et al .:. PA-457: a potent HIV inhibitor did disrupts core condensation by targeting a late step in Gag processing. In: Proceedings of the National Academy of Sciences . Volume 100, number 23, November 2003, pp. 13555-13560, doi: 10.1073 / pnas.2234683100 . PMID 14573704 . PMC 263852 (free full text).
- ↑ G. Beatty, J. Jacobson, J. Lalezari et al. Safety and Antiviral Activity of PA-457, the First-In-Class Maturation Inhibitor, in a 10-Day Monotherapy Study in HIV-1 Infected Patients. Abstract H-416D, 45th ICAAC 2005, Washington.
- ^ Report on phase IIb at Berivimat
- ↑ Indrani Sarkar, Ilona Hauber, Joachim Hauber, Frank Buchholz; HIV-1 Proviral DNA Excision Using an Evolved Recombinase; Science, 316, No. 5833, 2007, pp. 1912-1915 . Sciencemag.org. June 29, 2007. Retrieved September 9, 2010.
- ↑ Humanized mice are mice of certain breed lines with defects in the immune system, which is then completely destroyed by irradiation. The mice are then equipped with a human immune system by transplanting human blood stem cells.
- ↑ Highly Significant Antiviral Activity of HIV-1 LTR-Specific Tre-Recombinase in Humanized Mice . Plospathogens.org. September 26, 2013. Retrieved October 20, 2013.
- ↑ DH Barouch, JB Whitney et al .: Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal antibodies in SHIV-infected rhesus monkeys. In: Nature. Volume 503, number 7475, November 2013, pp. 224-228, doi: 10.1038 / nature12744 . PMID 24172905 . PMC 4017780 (free full text).
- ^ TJ Henrich, Z. Hu et al .: Long-term reduction in peripheral blood HIV type 1 reservoirs following reduced-intensity conditioning allogeneic stem cell transplantation. In: The Journal of Infectious Diseases. Volume 207, number 11, June 2013, pp. 1694–1702, doi: 10.1093 / infdis / jit086 . PMID 23460751 . PMC 3636784 (free full text).
- ↑ rme / aerzteblatt.de: HIV: "Healed" Boston patients suffer relapse. In: aerzteblatt.de . December 9, 2013, accessed December 26, 2014 .
- ↑ Kerstin Decker: AIDS healing: anatomy of a miracle. Der Tagesspiegel , June 6, 2011, accessed on November 25, 2018 .
- ^ Clare Wilson: Immune war with donor cells after transplant may wipe out HIV. In: newscientist.com . May 3, 2017, accessed November 25, 2018.
- ↑ P. Tebas, D. Stein, WW Tang, I. Frank, SQ Wang, G. Lee, SK Spratt, RT Surosky, MA Giedlin, G. Nichol, MC Holmes, PD Gregory, DG Ando, M. Kalos, RG Collman, G. Binder-Scholl, G. Plesa, WT Hwang, BL Levine, CH June: Gene editing of CCR5 in autologous CD4 T cells of persons infected with HIV. In: The New England Journal of Medicine . Volume 370, number 10, March 2014, pp. 901-910, doi: 10.1056 / NEJMoa1300662 , PMID 24597865 , PMC 4084652 (free full text).
- ↑ HIV-PrEP. May 13, 2019, accessed January 30, 2021 .
- ↑ Marianne Abele-Horn (2009), p. 304 f.
- ↑ a b UNAIDS 2016 GLOBAL FACT SHEET (PDF; 342 kB) unaids.org. 2016. Retrieved November 17, 2016.
- ↑ UNAIDS DATA 2018 (PDF; 11.9 MB) unaids.org. 2018. Accessed December 1, 2018.
- ↑ UNAIDS DATA 2019 (PDF; 13.1 MB) unaids.org. 2019. Retrieved August 2, 2019.
- ↑ UNAIDS DATA 2020 (PDF; 12.0 MB) unaids.org. 2020. Accessed July 6, 2020.
- ↑ W. David Hardy: Fundamentals of HIV Medicine 2019. Oxford 2019, p. 15
- ↑ Genetic analysis: AIDS went undetected in the USA for a decade. In: Spiegel Online . October 30, 2007, accessed December 26, 2014 .
- ^ Daniel T. Halperin et al .: A Surprising Prevention Success: Why Did the HIV Epidemic Decline in Zimbabwe? In: PLOS Medicine . No. 8 (2) , February 2011, doi : 10.1371 / journal.pmed.1000414 (English).
- ↑ Bavaria: Thinning out degeneracy. Der Spiegel , March 16, 1987
- ↑ Johann Osel: When Bavaria Aids declared war. Süddeutsche Zeitung, February 25, 2017.
- ↑ a b HIV / AIDS in Germany - key data of the estimate. (PDF) (No longer available online.) December 2015, archived from the original on November 17, 2016 ; accessed on November 17, 2016 .
- ↑ Robert Koch Institute (Ed.): Epidemiological Bulletin 24/2013 . June 17, 2013 ( rki.de [PDF; accessed on February 4, 2014] Table 5).
- ↑ Holger Wicht: Berlin researchers develop estimation methods: 10 percent of gay city dwellers are HIV-positive. In: magazin.hiv. German AIDS Help, July 11, 2009, accessed October 30, 2019 .
- ↑ prevention initiative HIV-Symptome.de: HIV statistics 2009/2010 . Retrieved April 19, 2011.
- ↑ "Virus Epidemiological Information" No. 3/16. (PDF; 634 kB) In: virologie.meduniwien.ac.at. 2016, accessed August 4, 2019 .
- ↑ HIV and STI case numbers 2014: reporting, analyzes and trends ( Memento from March 4, 2016 in the Internet Archive ) (PDF; 3.1 MB)
- ↑ UNAIDS : UNAIDS The GAP Report (2014) . ( PDF; 2.5 MB [accessed June 13, 2015]).
- ↑ Study - Original virus of HIV older than expected. In: orf.at. September 17, 2010, accessed March 6, 2019 .
- ↑ Donald G. McNeil Jr .: Researchers Have New Theory on Origin of AIDS Virus. In: nytimes.com . June 13, 2003, accessed June 21, 2020.
- ↑ A. J. Nahmias, J. Weiss et al .: Evidence for human infection with an HTLV III / LAV-like virus in Central Africa, 1959. In: Lancet. Volume 1, Number 8492, May 1986, pp. 1279-1280, PMID 2872424 .
- ↑ Jack Z. Bratich: AIDS. In: Peter Knight (Ed.): Conspiracy Theories in American History. To Encyclopedia. Vol. 1. ABC Clio, Santa Barbara / Denver / London 2003, pp. 42-48.
- ↑ T. Zhu, BT Korber, AJ Nahmias, E. Hooper, PM Sharp, DD Ho: "An African HIV-1 sequence from 1959 and implications for the origin of the epidemic" . In: Nature . 391, No. 1998-02-05, 1998, pp. 594-597. PMID 9468138 .
- ↑ M. Worobey, M. Gemmel, DE Teuwen, T. Haselkorn, K. Kunstman, M. Bunce, J.-J. Muyembe, J.-MM Kabongo, RM Kalengayi, E. Van Marck, MTP Gilbert, SM Wolinsky: "Direct evidence of extensive diversity of HIV-1 in Kinshasa by 1960" . In: Nature . 455, No. 2008-10-02, 2008, pp. 661-664. PMID 18833279 .
- ^ "Epidemiologic Notes and Reports: Pneumocystis Pneumonia --- Los Angeles." , Morbidity and Mortality Weekly Report , June 5, 1981/30 (21); 1-3
- ^ Epidemiologic Notes and Reports Update on Kaposi's Sarcoma and Opportunistic Infections in Previously Healthy Persons - United States . In: Morbidity and Mortality Weekly Report , June 11, 1982, 31 (22), 294, pp. 300-301
- ↑ Centers for Disease Control (CDC): Persistent, generalized lymphadenopathy among homosexual males . In: MMWR Morb Mortal Wkly Rep. . 31, No. 19, 1982, pp. 249-251. PMID 6808340 .
- ^ "A Cluster of Kaposi's Sarcoma and Pneumocystis carinii Pneumonia among Homosexual Male Residents of Los Angeles and range Counties, California" , Morbidity and Mortality Weekly Report , June 18, 1982/31 (23); 305-7
- ↑ Centers for Disease Control (CDC): Opportunistic infections and Kaposi's sarcoma among Haitians in the United States . In: MMWR Morb Mortal Wkly Rep. . 31, No. 26, 1982, pp. 353-354; 360-361. PMID 6811853 .
- ↑ F Barré-Sinoussi, JC Chermann, F Rey et al .: Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS) . (PDF) In: Science . 220, No. 4599, 1983, pp. 868-871. doi : 10.1126 / science.6189183 . PMID 6189183 . ("References and Notes")
- ^ LK Altman: New homosexual disorder worries officials . In: The New York Times . June.
- ↑ Epidemiologic Notes and Reports Pneumocystis carinii Pneumonia Among Persons with Hemophilia A . In: Morbidity and Mortality Weekly Report . No. 1982/31 (27) , July 16, 1982, pp. 365-367 ( cdc.gov [accessed July 15, 2020]).
- ↑ CDC: Possible transfusion-associated acquired immune deficiency syndrome (AIDS) - California . In: MMWR Morb Mortal Wkly Rep . 31, No. 48, 1982, pp. 652-654. PMID 6819440 .
- ↑ Making Headway Under Hellacious Circumstances (PDF; 556 kB) American Association for the Advancement of Science . July 28, 2006. Retrieved June 3, 2011.
- ↑ U. Kher: A Name for the Plague - 80 Days That Changed the World . In: Time , March 31, 2003. Retrieved March 10, 2008.
- ↑ Centers for Disease Control (CDC): Update on acquired immune deficiency syndrome (AIDS) —United States. . In: MMWR Morb Mortal Wkly Rep. . 31, No. 37, 1982, pp. 507-508; 513-514. PMID 6815471 .
- ↑ A shock from over there . In: Der Spiegel . No. 22 , 1982, pp. 187-189 ( online ).
- ↑ Lars-Broder Keil: An epidemic is becoming commonplace. In: welt.de . December 1, 2006, accessed December 26, 2014 .
- ↑ AIDS: an epidemic that is only just beginning . In: Der Spiegel . No. 23 , 1983 ( online ).
- ↑ See also entry Schwulenpest at Wiktionary .
- ↑ Margit Mennert: The history of AIDS support of Austria , p.8 and Frank M. Amort: consulting , 52. In: Common goals obligation - 20 years AIDS support in Austria . AIDS Aid Salzburg, 2005 ( Online [PDF; 906 kB ; accessed on September 30, 2018]).
- ↑ F. Barre-Sinoussi et al .: "Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS)" . In: Science . 220, No. 4599, 1983, pp. 868-871. PMID 6189183 .
- ↑ Popovic et al .: "Detection, isolation, and continuous production of cytopathic retroviruses (HTLV-III) from patients with AIDS and pre-AIDS" . In: Science . 224, No. 4648, 1984, pp. 497-500. PMID 6200935 .
- ↑ On the term “human” see Gundolf Keil : Dealing with AIDS sufferers as a challenge to a humane society. “Statement” on the acquired immune deficiency syndrome from a specialist historical perspective. In: Johannes Gründel (Ed.): AIDS. Challenge to society and morals. 2nd Edition. Düsseldorf 1988 (= writings of the Catholic Academy in Bavaria. Volume 125), p. 31–41, here: p. 32 f.
- ^ Ronald Reagan Remembered - First Public Discussion of HIV / AIDS. Transcript of the October 15, 1982 press conference. In: thebody.com. June 12, 2004, accessed December 9, 2019 .
- ↑ a b How Reagan "made Aids possible". In: orf.at. June 5, 2011, accessed December 3, 2018 .
- ↑ Andrew James McMichael: Norman Letvin 1949–2012. In: Nature Immunology . Volume 13, 2012, p. 801, doi: 10.1038 / ni.2399 .
- ↑ Ingolf Lück is buying condoms again. In: n-tv.de . May 4, 2016, accessed March 15, 2020.
- ↑ J. Cohen: The Duesberg phenomenon. ( Memento of January 6, 2004 in the Internet Archive ) In: Science. Volume 266, Number 5191, December 1994, pp. 1642-1644, PMID 7992043 .
- ^ Final report of the South African AIDS expert commission 2001 (PDF; 1.1 MB) p. 10 (English).
- ↑ N. Nattrass: AIDS Denialism vs. Science . In: Skeptical Inquirer . 31, No. 5, 2007.
- ↑ Mark Strauss: Nobel Laureates Who Were Not Always Noble. In: nationalgeographic.com.au. October 4, 2017, accessed July 18, 2018 .
- ^ Opinion on hypotheses of the so-called Perth Group (V. Turner, E. Papadopoulos-Eleopulos, S. Lanka, etc.) on the isolation and detection of HIV, the connection between HIV and AIDS and the effect and effectiveness of nucleoside analogues in antiretroviral therapy. (PDF, 42.5 kB) In: rki.de . Retrieved January 17, 2020 .
- ↑ Pride Chigwedere, M. Essex: AIDS Denialism and Public Health Practice. In: AIDS and Behavior. 14, 2010, p. 237, doi: 10.1007 / s10461-009-9654-7 .
- ↑ AIDS poster in Africa. (File: Reuters): The denial of AIDS kills (Wissenschaft, NZZ Online) . Nzz.ch. January 27, 2010. Retrieved January 30, 2014.
- ^ J. Watson: Scientists, activists sue South Africa's AIDS 'denialists'. In: Nature medicine. Volume 12, Number 1, January 2006, p. 6, doi: 10.1038 / nm0106-6a . PMID 16397537 .
- ^ The Durban Declaration . In: Nature . 406, No. 6791, 2000, pp. 15-16. PMID 10894520 . nature.com .
- ^ TC Smith, SP Novella: HIV Denial in the Internet Era . In: PLoS Med. . 4, No. 8, 2007, p. E256. doi : 10.1371 / journal.pmed.0040256 . PMID 17713982 .
- ^ Scott Burris, Edwin Cameron, Michaela Clayton: The Criminalization of HIV: Time for an Unambiguous Rejection of the Use of Criminal Law to Regulate the Sexual Behavior of Those with and at Risk of HIV . Shorter in: S. Burris, E. Cameron: The Case Against Criminalization of HIV Transmission . In: JAMA , Vol. 300, Issue 6, August 6, 2008, pp. 578-581.
- ↑ Jan van Lunzen, Helmut Albrecht: treatment of opportunistic diseases. In: Eberhard Aulbert, Friedemann Nauck, Lukas Radbruch (eds.): Textbook of Palliative Medicine. Schattauer, Stuttgart (1997) 3rd, updated edition 2012, ISBN 978-3-7945-2666-6 , pp. 710-737.
- ↑ Michael Ewers: Points of contact for psychosocial support Support for seriously ill and dying people with HIV / AIDS In: Eberhard Aulbert, Friedemann Nauck, Lukas Radbruch (eds.): Textbook of Palliative Medicine. Schattauer, Stuttgart (1997) 3rd, updated edition 2012, ISBN 978-3-7945-2666-6 , pp. 738-750.
- ↑ Bartholomäus Grill, Stefan Hippler: God Aids Africa: The deadly silence of the Catholic Church . Bastei Lübbe, 2009, ISBN 978-3-404-60615-3 . Catholic Church crisis . Mirror online. April 8, 2010. Retrieved September 9, 2010.
- ↑ Male prostitutes are allowed to use condoms - says the Pope. In: sueddeutsche.de . November 21, 2010, accessed July 8, 2020 .
- ↑ Deutsche AIDS-Hilfe publishes data on discrimination against people with HIV for the first time. Deutsche AIDS-Hilfe , August 22, 2012, accessed on February 17, 2014 .
- ↑ Dental care for people infected with HIV. DAIG e. V., October 2010, accessed July 8, 2014 .
- ^ Fight against “social” AIDS. Der Standard , December 1, 2009, accessed February 18, 2014 .
- ↑ Food: Dentist refuses treatment for HIV-positive patients. In: Ondamaris.de. February 4, 2010, accessed December 26, 2014 .
- ↑ Ute Vetter: Survey in Hanau and Main-Kinzig: Doctors are afraid of AIDS. In: fr-online.de . March 20, 2010, accessed December 26, 2014 .