Pancreatitis
| Classification according to ICD-10 | |
|---|---|
| K85.- | Acute pancreatitis |
| K86.0 | Alcohol-induced chronic pancreatitis |
| K86.1 | Other chronic pancreatitis |
| K87.1 | Diseases of the pancreas in diseases classified elsewhere |
| ICD-10 online (WHO version 2019) | |
The pancreatitis (from ancient Greek πάγκρεας pancreas , German , pancreas ' , this turn of πᾶν pán , German , everything ' and κρέας kreas , German , meat' and itis ) or pancreatitis is a gastrointestinal disease and can in principle two progressive forms divide, in the acute and chronic . Acute pancreatitis is characterized by severe pain in the upper abdomen, nausea, vomiting, constipation, and fever. It is mainly treated with intensive intravenous fluids and pain medication. Chronic pancreatitis manifests itself in repeated upper abdominal pain, nausea, vomiting, poor digestion, fatty stools and weight loss.
Acute pancreatitis
This disease is based on self-digestion, sometimes also referred to as autolysis . Here, digestive enzymes such as B. the trypsinogen , phospholipase A u. a. activated too early in the pancreas (intrapancreatic). A major role is assigned to the early activation of trypsinogen, since the successor, trypsin , in turn activates other proteolytic and lipolytic enzymes, i.e. lipase and phospholipase . Since it is the job of these enzymes to digest proteins , fats and carbohydrates, the organ begins to digest itself. What is certain is that the local trypsin inhibitors α-antitrypsin and α-macroglobulin cannot prevent autodigestion. Some patients have acute pancreatitis multiple times, but can make full recovery each time. Acute pancreatitis can be a life-threatening condition that causes numerous complications, but patients usually recover from acute pancreatitis. The incidence is around 20-30 cases per 100,000 people per year.
causes
The acute pancreatitis can have several causes. In 75–80% of cases, the cause is biliary (caused by the gall bladder) or alcohol-toxic. The most common are gallstones ( choledocholithiasis ), which temporarily or for a longer period get stuck in the mouth of the bile duct in the duodenum , which is also the mouth of the pancreatic duct ( papilla Vateri ) (around 45% of acute pancreatitis). This allows duodenal juice to flow back into the pancreatic ducts. As a result, bile acid damages the epithelium of the pancreatic duct and triggers an increase in permeability , including for phospholipase , which converts phosphatides into cytotoxic lysophosphatides .
Another trigger for acute pancreatitis can be excessive alcohol consumption (about 35% of cases); however, the exact relationship between alcohol consumption and the etiologist is unclear. The risk increases with the amount of alcohol consumed, which suggests a direct toxic effect. However, only 5% of all alcoholics develop pancreatitis, so that other factors, possibly also a genetic predisposition, play a role. As in acute biliary pancreatitis, there is an increase in the permeability of the duct system, changes in the secretion and composition of the bile and duct sclerosis . In addition, alcohol directly damages the acini and adversely affects the motility of the Sphincter Oddi .
In about 15% of those affected, no specific trigger can be determined, in these cases one speaks of idiopathic genesis.
In addition, there are also rarer causes such as:
- Infections , e.g. B. mumps , Coxsackie virus , hepatitis , HIV , cytomegalovirus virus
- increased blood calcium levels , e.g. B. in overactive parathyroid glands
- very high blood lipids ( hypertriglyceridaemia )
- Papillary or pancreatic tumor as obstructive neoplasms obstructing the drainage ducts
- iatrogenic according to ERCP
- genetic: cystic fibrosis
- autoimmune pancreatitis
- Abdominal injuries and trauma
- Pancreas divisum
- as a side effect of drugs (e.g. asparaginase , azathioprine , furosemide , glucocorticoids , antibiotics ( fluoroquinolones , tetracyclines , sulfamethoxazole , trimethoprim ), anticonvulsants ( valproate , carbamazepine ), propofol , omeprazole and others)
Symptoms
Acute pancreatitis is initially noticeable as an acute, violent pain in the upper abdomen ( epigastrium ), which often radiates into the back in a belt shape. Characteristic of the physical examination are an abdomen that is painful on pressure and a so-called rubber belly , which is caused by meteorism and (moderate) defensive tension. Pain in the lower thoracic spine can also occur. This pain is initially similar to a slight lumbago , but subsequently develops more into a "being pierced" from the back to the area of the pancreatic head on the abdomen. The pain is accompanied by nausea and vomiting as a consequence of the passage disruption.
Other symptoms include constipation and fever ; in severe cases, jaundice (occur jaundice ) (biliary tract during installation), ascites ( ascites , sympathetic stimulus effusions by toxins, enzymes and kinins) (When extending the portal system ), by exudate (medicine) caused pleural effusions and shock - and sepsis signs added. With a severe course, bluish-greenish spots ( ecchymosis ) around the navel ( Cullen's sign ) or in the flank area ( Gray-Turner's sign ) can also be observed .
Laboratory diagnostics reveal an increased serum concentration of the pancreatic enzymes trypsin , amylase and pancreatic lipase , but there is no correlation between the extent of the enzyme derailment and the severity of the disease. The magnesium , sodium , potassium , hydrogen carbonate , sugar or fat levels in the blood can also be increased, as can the white blood cell count ( leukocytosis ). Serum calcium is occasionally decreased, which is an unfavorable prognostic factor. About 20% of acute pancreatitis cases are serious.
Complications
In addition to local complications such as tryptic digestion of neighboring organ structures, the formation of pseudocysts and thrombosis in the portal venous flow area, there are mainly systemic effects of the inflammation on the circulatory system, the patient can become dehydrated and develop low blood pressure , or even shock. Sometimes heart , lung or kidney failure occurs . The severe course is characterized by hemorrhagic- necrotizing inflammation with high mortality .
Degrees of severity
According to the current Atlanta classification (2013), a distinction is made between mild, moderate and severe acute pancreatitis. A mild (also serous or edematous) self-limiting acute pancreatitis is found in 80%, a severe necrotizing in 20% of the cases.
An outdated classification differentiated an edematous form (early stage), a hemorrhagic form with local or generalized bleeding, and an acute necrotizing form.
Several scores can be used to estimate the severity of pancreatitis, such as the APACHE II and the Balthazar score. In medical treatment, the so-called Ranson score is used to estimate the prognosis for acute pancreatitis:
| At recording: | after 48 hours: | ||
|---|---|---|---|
| Age> 55 years | 1 point | Hematocrit drop> 10% | 1 point |
| Leukocytes> 16,000 / mm 3 | 1 point | Urea increase> 1.8 mmol / l (> 5 mg / dl) | 1 point |
| LDH> 350 U / l | 1 point | Calcium <2 mmol / l | 1 point |
| AST (GOT)> 250 U / l | 1 point | PaO 2 <8 kPa (<60 mm Hg) | 1 point |
| Glucose> 10 mmol / l (approx. 200 mg / dl) | 1 point | Base deficit > 4 mEq / l | 1 point |
| Fluid balance> 6 l / 48 h | 1 point | ||
| Lethality in acute pancreatitis | evaluation | ||
|---|---|---|---|
| 0–2 points: | Mortality <5% | 0–2 points: | mild pancreatitis |
| 3–4 points: | Mortality 15-20% | ≥ 3 points: | severe pancreatitis |
| 5–6 points: | Mortality 40% | ||
| > 6 points: | Mortality> 99% | ||
therapy
In acute pancreatitis, generous intravenous fluids (i.e., infusions) should be started immediately to prevent impending volume shock.
For a long time it was believed that a zero diet could prevent the pancreas from producing decomposing enzymes , but it is now known that a diseased pancreas produces hardly any enzymes. Therefore, nutritional therapy is now of little importance. In the case of mild forms, normal food can be taken, which may be supported with proton pump inhibitors or orally substituted pancreatic enzymes ; in severe forms with intestinal paralysis, early nutrition via the intestine is currently recommended, for which a special nasal and small intestinal tube is inserted if necessary. This significantly lowers the complications caused, for example, by bacteria passing through the intestinal barrier.
To prevent a stress ulcer and to avoid acid secretion in the pancreas, the administration of a proton pump blocker such as omeprazole is recommended.
Oral or intravenous pain therapy with opioids ( pethidine , buprenorphine , tramadol ) or NSAIDs ( pethidine , buprenorphine , tramadol ) or NSAIDs , which have as little influence as possible, is also important , since pancreatitis is associated with considerable pain. Pain therapy with bupivacaine or ropivacaine via an epidural catheter is also useful with a simultaneous positive effect on intestinal peristalsis.
If the pancreatitis was triggered by a pinched gallstone, which leads to a build-up of bile, this must be removed using ERCP . Any changes in blood values are compensated for with infusions .
Therapy with antibiotics (meropenem, ciprofloxacin and metronidazole or piperacillin / Combactam are possible) is only considered sensible if there are pronounced signs of infection or a severe necrotizing course, since the majority of pancreatitis are primarily sterile and there is a risk of superinfection or selection resistant germs. Attention should also be paid to the blood sugar level, as pancreatitis can lead to a lack of insulin , which, as with type I diabetes mellitus , leads to hyperglycemia . If complications such as infections, cysts or bleeding occur, surgical or endoscopic intervention to remove necrotic (dead) tissue or to drain it with the help of drainage from cysts may be indicated.
If high triglyceride concentrations in the blood of more than 1000 mg / dl (severe hypertriglyceridaemia ) are the cause of acute and severe pancreatitis, a rapid lowering of the triglycerides through apheresis treatment can significantly improve the patient's prognosis. This is possible, for example, with the help of double filtration plasmapheresis (DFPP). In rare cases, patients with recurrent inflammation of the pancreas may require regular apheresis treatment. This can also reduce the likelihood of a relapse .
Chronic pancreatitis
causes
A chronic pancreatitis is defined as a persistent inflammatory disease of the pancreas. It manifests itself in the form of abdominal pain and / or in a permanent functional failure of the exocrine and / or endocrine pancreas. The incidence is directly related to the alcohol consumption of the population and averages 10 / 100,000 / year. Mostly men between the ages of 30 and 60 are affected (gender ratio 9: 1).
About 80% of the most important cause of chronic pancreatitis in adults is alcohol abuse. The necessary daily alcohol consumption averages more than 80 g over six to twelve years. However, alcohol itself should only be viewed as a cofactor for the development of chronic pancreatitis, as only about ten percent of heavy drinkers develop chronic pancreatitis. Smoking is considered an independent risk factor for the pathogenesis of chronic pancreatitis.
The hereditary autosomal dominant pancreatitis is the most common pancreatitis in childhood. Repeated attacks of acute pancreatitis with self- digesting necrosis lead to chronic pancreatitis. The cause is a mutation in the gene for the cationic trypsinogen (PRSS1) or in the gene for the serine protease inhibitor SPINK1. These two mutations seem to favor the auto-activation of trypsinogen to trypsin in the pancreas and thus repeatedly lead to the development of acute pancreatitis.
The autoimmune pancreatitis (AIP) Type 1 affects men twice as often as women, and is associated with other autoimmune diseases such as Sjogren's syndrome or primary biliary cholangitis connected. It is a rare, steroid-sensitive IgG systemic disease that occurs mainly in Asia. The diagnosis is based on an increase in IgG4. AIP type 2, which is associated with inflammatory bowel disease in about 30% of cases, has no IgG4 increase.
Other causes:
- Idiopathic (no apparent cause) in 15% of the cases
- Medicines: diuretics , beta blockers , ACE inhibitors , cytostatics , antibiotics , anti-epileptics, etc. a.
- Hypercalcemia in hyperparathyroidism
- Hyperlipidemia
- Chronic renal failure
- Genetic factors (see above)
- Tumor , papillary stenosis (closure of the main pancreatic duct, pancreas divisum )
Pathogenesis
There are several explanatory models for the pathogenesis of chronic pancreatitis. According to the current status, chronic alcohol abuse is not the sole cause of pancreatitis. In addition to permanently increased alcohol consumption, other factors such as B. a genetic predisposition. The exact pathogenesis has not yet been conclusively clarified.
Alcohol and its breakdown products are suspected of directly damaging the acinar cells of the pancreas. Digestive enzymes, which normally occur in an inactive form in the pancreas, could be activated prematurely in the pancreas and destroy pancreatic tissue. Animal experiments on rats showed that administration of ethanol increased the release of digestive and lysosomal enzymes from the acinar cells. In addition, it was also observed in rats that the zymogen granules , which contain the inactive precursors of the digestive enzymes, became more fragile after administration of ethanol. This could play a role in the early stages of the disease as it could allow lysosomal enzymes and digestive enzymes to come into contact in the pancreas. Fatty acid ethyl esters and oxidative stress are discussed as triggers for this. In addition, after administration of alcohol to rats, vacuolization of the acinar cells, edema and increased levels of extracellular matrix proteins were observed, which could indicate direct damage to the pancreatic tissue.
The current main hypothesis is based on the concept of the necrosis-fibrosis sequence . This assumes that the chronic pancreatitis develops from a recurrent acute pancreatitis. The immigration of inflammatory cells stimulates periductal stellate cells (located in the vicinity of the excretory ducts) to synthesize collagen , which ultimately leads to scarring around the small pancreatic ducts.
The now outdated pancreatic stone hypothesis postulates that massive and long-term alcohol abuse increases the protein concentration in the pancreatic secretion, which leads to protein precipitation (protein precipitates) in the ducts. Since the gland cells also secrete less pancreatic stone protein , which in normal concentrations prevents calcium precipitation in the duct system, the protein precipitates calcify and become calcium carbonate stones. These relocate the small passages and thus not only lead to their relocation, but also to direct damage to the passage with fibrosis . In the end, this leads to a complete relocation of the small passages, which leads to atrophy of the glandular tissue behind the constriction with replacement of connective tissue. Even if this theory is now considered out of date to explain the origin of the disease, these transfers in the late stages of the disease could contribute to pain and an increase in the frequency of relapses.
Symptoms
The main symptom is recurrent pain, which is not colicky and can last for hours to days. The pain lies deep in the upper abdomen and can radiate to both sides, even down to the back (belt-shaped). The late stage of chronic pancreatitis is often painless again.
In addition, food intolerance can appear, as the food can no longer be completely digested and thus more allergens are absorbed into the intestinal epithelial cells. After prolonged exposure, a type IV allergy to those random allergens can occur, where mast cells bind these allergens non-specifically without the presence of antibodies. In addition, there is nausea and vomiting, the patient loses weight.
The reduced function of the exocrine pancreas means that fewer digestive enzymes are released into the small intestine . This leads to maldigestion . Fat stools , meteorism and diarrhea are the result.
Endocrine pancreatic insufficiency occurs in up to 70% of patients as the inflammation progresses. Insulin deficiency diabetes (secondary diabetes mellitus ) manifests itself .
Complications
- Pancreatic pseudocysts with abscesses
- Spleen and portal vein thrombosis with portal hypertension
- Stenosis of the bile duct with jaundice
- Pancreatic cancer as a late complication (especially in hereditary pancreatitis)
diagnosis
Affected patients show cachexia (emaciation). The stomach is bloated and elastic ("rubber belly") with weakened bowel sounds .
There is also pain on the palpation between the last rib on the left and the spine at the so-called pancreatic pressure point .
The pancreatic enzymes amylase and lipase are determined in the blood and are usually elevated in chronic pancreatitis. Chymotrypsin and elastase are measured in the stool . As a result of the inflammation, the stool concentrations of the two enzymes are reduced.
The secretin-pancreozymin test is used to detect exocrine pancreatic insufficiency: the patient is given the hormone secretin intravenously and the duodenal secretion is obtained through a small intestinal probe. Then the concentrations of hydrogen carbonate , chymotrypsin , amylase and lipase are determined.
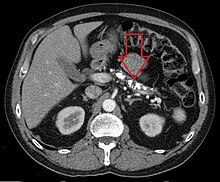
Pancreatic calcifications are detected by ultrasound , X-rays of the upper abdomen, computed tomography or magnetic resonance imaging and prove chronic pancreatitis. Pancreatic duct stones are visualized with endoscopic retrograde cholangiopancreatography .
therapy
The only causal therapy is abstinence from alcohol, and smoking should also be given up.
- Pain therapy
-
- Alcohol abstinence leads to pain reduction in 50% of cases.
- Painkillers : non-steroidal anti-inflammatory drugs (NSAIDs) , butylscopolamine , tramadol , buprenorphine , pethidine , other opioids
- Antidepressants
- Celiac ganglion blockade
- Epidural anesthesia
- Therapy of exocrine pancreatic insufficiency
-
- Pancreatic enzyme substitution with acid-protected preparations that cannot be inactivated by gastric juice . Rizoenzymes are also suitable as an acid-stable alternative of non-animal origin. The dose must be adapted to the fat content of the meals.
- Histamine H-2 blockers or a proton pump inhibitor to reduce the production of gastric juice.
- Diet with <70 g / d dietary fat
- Sufficient protein intake (100–150 g / d), possibly also the substitution of fat-soluble vitamins (vitamins A, D, E and K)
- Therapy of endocrine pancreatic insufficiency
- In the case of diabetes mellitus caused by the inflammation, blood sugar control by means of diet and adequate insulin administration .
- Endoscopic or surgical intervention
- Endoscopic treatment of pancreatic duct stones, pancreatic duct stenosis and pancreatic pseudocysts. Surgical drainage operations , partial resections of the pancreas.
literature
Guidelines and current presentations
- S3- guideline for chronic pancreatitis of the German Society for Digestive and Metabolic Diseases (DGVS). In: AWMF online (as of 2012)
- Karsten Schwarting: Liver and Pancreas. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 389-400, here: pp. 396-399 ( acute pancreatitis ).
- Apheresis standard of the German Society for Nephrology eV, DGfN (status: 2019)
Textbooks
- Jürgen F. Riemann , Wolfgang Fischbach, Peter R. Galle, Joachim Mössner (eds.): Gastroenterology. The reference work for clinics and practices. Volume 2: Liver, Bile, Pancreas. Thieme, Stuttgart et al. 2008, ISBN 978-3-13-141201-0 , pp. 1803-1871.
- Hans-Konrad Biesalski, Peter Fürst, Heinrich Kasper, Reinhold Kluthe, Wolfgang Pölert, Christoph Puchstein, Hannes B. Stähelin: Nutritional medicine. According to the nutritional medicine curriculum of the German Medical Association . 3rd, expanded edition. Thieme, Stuttgart et al. 2004, ISBN 3-13-100293-X .
Review articles
- Joan M. Braganza, Stephen H. Lee, Rory F. McCloy, Michael J. McMahon: Chronic pancreatitis. In: Lancet. Volume 377, No. 9772, April 2011, ISSN 1474-547X , pp. 1184-1197, doi: 10.1016 / S0140-6736 (10) 61852-1 , PMID 21397320 (review).
- Jean-Louis Frossard, Michael L. Steer, Catherine M. Pastor: Acute pancreatitis. In: Lancet. Volume 371, No. 9607, January 2008, pp. 143-152, doi: 10.1016 / S0140-6736 (08) 60107-5 , PMID 18191686 (review).
- Wolfgang Huber, Roland M. Schmid: Acute pancreatitis: Evidence-based diagnostics and therapy (PDF; 291 kB). In: Deutsches Ärzteblatt . Vol. 104, No. 25, June 22, 2007, pp. A-1832-A-1841.
- Julia Mayerle, Albrecht Hoffmeister, Heiko Witt, Markus M. Lerch, Joachim Mössner: Chronic pancreatitis: definition, etiology, diagnosis and therapy . In: Dtsch Arztebl Int . No. 110 (22) , 2013, p. 387-393 ( review ).
Web links
- Markus M. Lerch: Acute Pancreatitis - Clinic, Pathogenesis and Diagnostics. Internal therapy (Clinic of the Ernst-Moritz-Arndt University Greifswald)
- Erich Mayer-Fally: Inflammation of the pancreas. NetDoktor.at
- MedicoConsult: Chronic Pancreatitis
- European Pancreas Center Heidelberg : Patient information on the subject of pancreatic diseases PDF file (2.5 MB)
Individual evidence
- ^ Medical-scientific department of Fresenius AG (ed.): Infusion therapy and clinical nutrition . 15th, revised edition. Fresenius AG, Bad Homburg vd H. 1987.
- ↑ a b Hans-Konrad Biesalski, Peter Fürst, Heinrich Kasper, Reinhold Kluthe, Wolfgang Pölert, Christoph Puchstein, Hannes B. Stähelin: Nutritional medicine. According to the nutritional medicine curriculum of the German Medical Association . 3rd, expanded edition. Thieme, Stuttgart et al. 2004, ISBN 3-13-100293-X , p. 372 .
- ↑ a b c d e f g h i j Jörg R. Siewert 1940-, Martin Allgöwer 1917-, Robert Bernhard Brauer, Hubert J. Stein: Surgery with integrated case quiz; with 159 tables . Springer Medicine, 2012, ISBN 978-3-642-11330-7 .
- ↑ https://medicalforum.ch/article/doi/smf.2018.03369
- ↑ https://www.der-arzneimittelbrief.de/de/Artikel.aspx?J=2011&S=09
- Jump up ↑ Hye Young Sung, Jin Il Kim, Hyun Jeong Lee, Hyung Jun Cho, Dae Young Cheung: Acute Pancreatitis Secondary to Ciprofloxacin Therapy in Patients with Infectious Colitis . In: Gut and Liver . tape 8 , no. 3 , May 2014, p. 265–270 , doi : 10.5009 / gnl.2014.8.3.265 , PMID 24827622 , PMC 4026643 (free full text).
- ↑ Ayse Kefeli, Adem Akturk, Abdullah Yeniova, Sebahat Basyigit: Ciprofloxacin induced pancreatitis: Has this condition been overlooked? tape 79 , March 1, 2016 ( researchgate.net [accessed March 18, 2018]).
- ↑ José Luis Domínguez Jiménez, Enrique Bernal Blanco, Miguel Alonso Marín Moreno, Juan Jesús Puente Gutiérrez: [Acute pancreatitis associated with levofloxacin] . In: Gastroenterologia Y Hepatologia . tape 32 , no. 4 , April 2009, p. 323-324 , doi : 10.1016 / j.gastrohep.2008.09.027 , PMID 19371975 .
- ↑ a b Gerd Herold : Internal Medicine . Herold, Cologne 2007, p. 450 .
- ^ John H. Ranson: Etiological and Prognostic Factors in Human Acute Pancreatitis: A Review . In: American Journal of Gastroenterology . tape 77 , no. 9 , 1982, ISSN 0002-9270 , pp. 633-638 , PMID 7051819 .
- ↑ Karsten Schwarting: Liver and Pancreas. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 389-400, here: pp. 396-399 ( acute pancreatitis ).
- ↑ Karsten Schwarting: Liver and Pancreas. 2016, p. 398 ( pain relief and accompanying therapy ).
- ↑ Karsten Schwarting: Liver and Pancreas. 2016, p. 398 ( pain relief and accompanying therapy ).
- ↑ Karsten Schwarting: Liver and Pancreas. 2016, p. 398 ( pain relief and accompanying therapy ).
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 124 f.
- ↑ Padmanabhan A, Connelly-Smith L, Aqui N, Balogun RA, Klingel R, Meyer E, Pham HP, Schneiderman J, Witt V, Wu Y, Zantek ND, Dunbar NM, Schwartz GEJ: Guidelines on the Use of Therapeutic Apheresis in Clinical Practice - Evidence-Based Approach from the Writing Committee of the American Society for Apheresis: The Eighth Special Issue . In: J Clin Apher. tape 34 , no. 3 , June 2019, p. 171-354 , PMID 31180581 .
- ↑ Chiz-Tzung Chang, Tsung-Yu Tsai, Hsin-Yi Liao, Chia-Ming Chang, Jyun-Shan Jheng, Wen-Hsin Huang, Che-Yi Chou, Chao-Jung Chen: Double filtration plasma apheresis shortens hospital admission duration of patients with severe hypertriglyceridemia-associated acute pancreatitis . In: pancreas . tape 45 , no. 4 , April 2016, p. 606-612 , PMID 26491906 .
- ↑ Grupp C, Beckermann J, Köster E, Zewinger S, Knittel M, Walek T, Hohenstein B, Jaeger B, Spitthöver R, Klingel R, Fassbender CM, Tyczynski B: Relapsing and Progressive Complications of Severe Hypertriglyceridemia: Effective Long-Term Treatment with double filtration plasmapheresis . In: Blood Purification . March 2020, p. 1-11 , PMID 32191938 .
- ↑ S3-Guideline Chronic Pancreatitis ( Memento of the original of 23 September 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. , P. 14.
- ↑ Werner Böcker, Helmut Denk, Philipp U. Heitz (Ed.): Pathology . 3rd, completely revised edition. Urban & Fischer, Munich et al. 2004, ISBN 3-437-42381-9 , pp. 812-815 .
- ↑ a b c d e f g H. Witt: Pathogenesis of chronic pancreatitis. In: Pathogenesis of Chronic Pancreatitis. Volume 9, Issue 1, January 2014, ISSN 1861-9681 , pp. 6-13.
- ↑ MV Apte, JS Wilson, GW McCaughan, MA Korsten, PS Haber, ID Norton, RC Pirola: Ethanol-induced alterations in messenger RNA levels correlate with glandular content of pancreatic enzymes. In: J Lab Clin Med. 1995 May; 125 (5), pp. 634-640.
- ^ PS Haber, JS Wilson, MV Apte, MA Korsten, RC Pirola: Chronic ethanol consumption increases the fragility of rat pancreatic zymogen granules. In: Good. 1994 Oct; 35 (10), pp. 1474-1478.
- ^ Ernst-Albert Meyer: Digestive complaints: Plant enzymes as a therapy option. In: PTA-Forum , issue 04/2008.