Small intestine
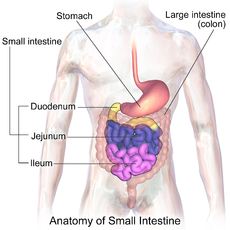
The small intestine ( Latin: intestinum tenue ) is part of the digestive tract and is used to absorb nutrients from food. For this purpose, it is lined with numerous villi (elevations) and crypts (depressions), so that the surface is greatly enlarged and reaches a multiple of the body surface. With a length of three to five meters, the small intestine is the longest part of the digestive tract. It reaches from the gatekeeper of the stomach to the ileocecal valve at the transition to the large intestine and is in the duodenum ( duodenum ), the jejunum ( jejunum ) and ileum ( ileal divided). In addition to its function of absorbing nutrients, the small intestine is also the main place of water absorption in humans. Diarrhea therefore quickly leads to dehydration.
anatomy
Location and structure
The location and structure of the small intestine differ depending on its sections: It begins as a duodenum (Latin: duodenum ) with an enlarged section ( ampulla duodeni or bulbus duodeni ) at the gastric gate . This is a sphincter muscle, the sphincter pylori muscle , which has the task of controlling the flow of food into the duodenum. If the muscle is in a tense state, the opening between the stomach and the duodenum, the pyloric ostium, is closed and no stomach contents can get into the duodenum. Stomach contents ( chyme ) can only penetrate through brief relaxation and thus opening the ostium pyloricum .
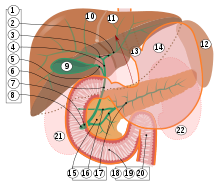
The duodenum is roughly C-shaped and twelve finger widths long (hence the name), which corresponds to about 25 to 30 cm. The chyme therefore first reaches an upper horizontal part ( pars superior ) at the level of the first lumbar vertebra . This part is covered by the right lobe of the liver , to which it is connected by a hepatoduodenal ligament . In addition, the affected superior part of the quadrate lobe of the liver and gallbladder .

If you follow the chyme further in the duodenum, you come to its descending part ( pars descendens ), which reaches down to the third lumbar vertebra. There both ducts of the pancreas ( ductus pancreaticus and ductus pancreaticus accessorius ) and the bile duct open into the duodenum. It is through these passages that bile and the digestive enzymes of the pancreas, which are necessary to digest and absorb food, enter the intestines. When they enter the intestine, the ducts open papillae, the papilla duodeni minor and the papilla duodeni major ("Father's papilla"). In addition to its particular proximity to the pancreas, the descending part has a topographical relationship with the kidneys and adrenal glands.
Following the duodenum further, one arrives at its second horizontal part ( pars horizontalis ) and a last ascending part ( pars ascendens ). At a curve (the flexura duodenojejunalis ) it finally passes into the jejunum . This also marks the end of the upper gastrointestinal tract. Two peritoneum niches ( recessus duodenalis superior and inferior ) are also formed here, in which parts of the small intestine can become trapped. This entrapment , known as Treitz's hernia , results in a life-threatening intestinal obstruction .

The lower gastrointestinal tract begins with the jejunum. There is no sharp boundary in the ileum ( ileal over). Both lie in loops between the sections of the large intestine - the jejunum and ileum are, so to speak, framed by the large intestine. Together they make up the largest section of the small intestine at 3 to 5 meters, with about 2/5 of the length being accounted for by the jejunum and 3/5 by the ileum. Their length, like the length of the entire intestine, varies from person to person and also depends on the tension of the intestinal muscles. In surgery, only these two sections are usually included in the small intestine. The ileum finally opens end-to-side with the ostium ileale , also called the ileocecal valve or Bauhin valve , into the large intestine.
In addition to the proximity to other organs, the peritoneal relationships are decisive for the positional relationships of the small intestine. Except for a small section at the beginning, the duodenum is secondary retroperitoneal . Retroperitoneal i.e. the duodenum is not of peritoneum ( peritoneum surrounded); secondary means that this was not the case from the beginning, but that it came about in the course of development. The jejunum and ileum, on the other hand, are intraperitoneally , i.e. surrounded by peritoneum , over their entire length . The mesenteries are of particular importance : These are doubling of the peritoneum that pulls from the rear abdominal wall to the respective organ sections. In the area of the small intestine, the mesenteries arise at the level of the lumbar vertebrae three to five. This means that they are significantly longer on the intestine side than at their origin, which is why the individual loops of the small intestine can be moved relative to one another. The mesenteries also contain the conduction pathways (blood, nerve and lymph vessels) for the jejunum and ileum.
Feinbau

The small intestine basically has the typical wall structure of the gastrointestinal tract. The innermost layer is the mucous membrane ( mucosa ) with three subdivisions: A layer of single-layer cylinder epithelium ( lamina epithelialis ) represents the innermost barrier and rests on a layer of cellular connective tissue ( lamina propria ). This layer houses numerous blood vessels, nerves, lymph vessels and immune cells. The last sub-layer of the mucous membrane is composed of smooth muscle cells ( lamina muscularis mucosae ), which give the mucous membrane mobility. The mucous membrane is followed by a layer of loose connective tissue ( tela submucosa ), in which the larger blood and lymph vessels for the mucous membrane and a nerve plexus ( submucosal plexus ) are located. In addition, it enables the mucous membrane to move in relation to the subsequent muscle layer ( tunica muscularis ). This consists of smooth muscle cells, which are arranged as the inner circular muscle ( stratum circulare ) and as the outer longitudinal muscle layer ( stratum longitudinal ). This arrangement enables the organs of the gastrointestinal tract to perform pendulum and segmentation movements to mix the pulp, as well as peristaltic movements for further transport. The myenteric plexus (also called Auerbach plexus ), which, like the submucosal plexus, is part of the enteric nervous system, is located between the circular and longitudinal muscle layers . The outermost layer of the small intestine is the peritoneum, which is called the serosa here . Instead, there is a layer of loose connective tissue, the tunica adventitia, on the parts of the duodenum where the peritoneum is missing .
About this general structure of the gastrointestinal tract, the small intestine has some important features: Semicircular folds, the Kerckring folds, or Plicae circulares , are arranged across the course of the small intestine and protrude into its interior ( lumen ). These folds are formed by the mucous membrane and the underlying layer, the tela submucosa .
The system of villi and crypts is of greater importance. Villi are finger-shaped elevations on the mucous membrane of the small intestine that are primarily used to absorb food components. For this purpose, the epithelium of the villi consists mainly of enterocytes - specialized cells that carry numerous microvilli and special transporters on the side facing the lumen . The microvilli enlarge the intestinal surface extremely for better absorption ; the transporters transport food components directly into the cell. In order to remove the absorbed substances (except fats), the villi run through several arterioles in the longitudinal direction (i.e. inwards, towards the lumen) . At the top they merge into a flat system of capillaries under the epithelium. The substances can be transported away through this capillary system. To do this, they first enter the capillaries, which then enter a central venole . The venole forwards the blood and the substances from the food into the vascular systems under the mucous membrane and further via the veins of the small intestine to the portal vein (see also section on blood supply and lymphatic drainage ). The fats from food, on the other hand, are transported away via the lymph, so that one or more lymph capillaries also run in the villi. These transport the lymph to larger lymph vessels on the intestinal wall.
In contrast to villi, crypts are depressions in the epithelium in the mucous membrane. At the base of these crypts are multipotent stem cells that divide continuously. Their descendants rise up the crypt wall to the tip of the villi, differentiate during their migration and perform their specific tasks. Finally, at the tip of the sheath, the cells either die from cell death or are rejected. The epithelial cells of the villi are completely replaced about every five days, with cell renewal starting from the crypts. The crypts also contain Paneth cells . These cells are responsible for the immune system, for which they secrete antibacterial proteins. The villi and crypts enlarge the surface of the small intestine by about 7 to 14 times (approx. 4 m²). If you add the brush border (totality of the microvilli), you estimate the intestinal surface to be approx. 60 to 200 m² (depending on the textbook), which is much larger than the body surface.
Another special feature of the small intestine, which can only be found in the duodenum, are the Brunner glands ( glandulae duodenales ). These glands lie in large packages (which get smaller and smaller as the small intestine progresses) in the submucosa under the mucous membrane. They are involved in the build-up of the mucous layer that protects the epithelium against the acidic stomach contents and secrete hydrogen carbonate , which serves to neutralize the stomach contents.
Blood supply and lymph drainage
In the course of the gastrointestinal tract, the supply to the individual organs changes. The duodenum, as a transition structure between the upper and lower gastrointestinal tract, therefore has a special role: Branches from the abdominal cavity trunk ( celiac trunk ) of the aorta form a connection ( anastomosis ) with branches from the upper intestinal artery ( arteria mesenterica superior ) . The celiac trunk sends a common hepatic artery ( arteria hepatica communis ) from which an artery for the stomach and duodenum originates ( arteria gastroduodenalis ). From the gastroduodenal artery go again the upper pancreatic duodenal artery ( superior pancreaticoduodenal artery ) and the rear pancreatic duodenal artery ( arteria pancreaticoduodenalis posterior ), which (with direct branches duodenales Rami supply the upper and the descending part of the duodenum) . The upper pancreatic-duodenal artery connects ( anastomoses ) with the lower pancreatic-duodenal artery, which originates from the upper intestinal artery ( arteria mesenterica superior ) and which in turn provides branches for the other sections of the duodenum. The veins run like the arteries and are named like them, that is, there is also a lower and an upper pancreatic-duodenal vein that anastomose with each other. They open either directly into the portal vein ( vena portis hepatis ) or via the superior intestinal vein ( vena mesenterica superior ). However, variants are common.
The empty and ileum, on the other hand, are only supplied by branches of the upper intestinal artery ( arteria mesenterica superior ). Venom and ileum arteries ( arteriae jejunales and arteriae ileales ) emerge from it and form three superimposed vascular arcades (curved vascular sections). The end arteries , the arteriae rectae, branch off from the arcades and run straight to the intestinal wall. The veins are arranged in the same way as the arteries and all open into the superior visceral vein ( Vena mesenterica superior ), which opens into the portal vein of the liver.
The lymph of the small intestine has the special task of transporting fats ( lipids ) that have been absorbed by the intestinal villi. The lymph drainage from the duodenum and jejunum and ileum is different. The lymph of the duodenum first reaches the upper and lower pancreatic-duodenal lymph nodes ( Nodi lymphoidei pancreaticoduodenales superiores and inferiores ) and from there further into lymph nodes around the abdominal trunk, the Nodi lymphoidei celiaci . It then flows further into the intestinal trunk ( Truncus intestinalis ), into the lumbar cistern ( Cisterna chyli ) and finally into the milk breast duct ( Ductus thoracicus ), which finally ends in the left vein angle . The numerous lymph capillaries from the villi of the jejunum and ileum (see section Feinbau) unite to form larger lymph capillaries. These move with the blood vessels into the vascular arcades and reach 100 to 200 lymph nodes, the nodi lymphoidei juxtaintestinales . From there the lymph flows into the upper intestinal lymph nodes ( Nodi mesenterici superiores ), further into the intestinal trunk and then like the lymph of the duodenum to the left vein angle. From there it first reaches the lungs via the right half of the heart, which is useful there for the synthesis of surfactants .
Innervation
The entire small intestine is parasympathetically innervated by the posterior trunk of the vagus nerve ( Truncus vagalis posterior ). Sympathetic nerve fibers to the duodenum derived from the large intestine nerve ( thoracic splanchnic nerves ) from the spinal cord segments T5 to T9 and run to the aorta, where it together with other nerve fibers, a nerve plexus , the abdominal aortic plexus form. The celiac ganglion is embedded in this nerve plexus , where the nerve fibers for the duodenum are switched and from there continue to the duodenum. The empty and ileum are supplied by sympathetic fibers that run as a small visceral nerve ( nervus splanchnicus minor ) from the spinal cord segments Th10 and 11, also pull to the plexus aorticus abdominalis and are switched there in the ganglion mesentericum superius . From there they reach their successful organs, jejunum and ileum.
Development and developmental disorders
The individual parts of the small intestine develop in the embryo from different parts of the primitive intestinal tube: The upper horizontal part of the duodenum, the superior pars , still develops from the foregut , while all other parts of the duodenum, as well as the jejunum and ileum, come from the midgut . At the beginning, all parts of the intestine are covered with peritoneum, i.e. a mesentery that comes from the back wall of the abdominal cavity to the respective organs. In addition , like the stomach , the pars superior of the duodenum has another mesentery that comes from the front of the abdominal cavity. The pars superior of the duodenum is thus covered by an anterior and a posterior mesentery, the remaining sections of the intestine only by a posterior mesentery. The mesenteries of the respective organs in development are called as follows:
| anterior ( ventral ) mesentery | Organ (section) | posterior ( dorsal ) mesentery |
|---|---|---|
| Mesogastricum ventral | stomach | Mesogastricum dorsale |
| Mesoduodenum ventral | Duodenum, pars superior | Mesoduodenum dorsale |
| - | Duodenum, descending, horizontal and ascending parts | |
| - | Jejunum and ileum | Mesentery |
| - | appendix | Mesocaecum |
In addition, various organs develop from the epithelium of the duodenum into the mesenteries: the liver and biliary tract develop into the mesogastricum ventral and mesoduodenum ventral , the anterior pancreatic system into the mesoduodenum and the rear pancreatic system into the mesoduodenum dorsal .
For the further development of the duodenum, the rotation of the stomach is of crucial importance, which takes place from around the fifth week of development . When viewed from above, the stomach rotates clockwise by about 90 ° and finally tilts around a sagittal axis (axis from front to back). As a result, the duodenum first moves to the right and then a little upwards and develops its typical C-shape by the end of the stomach rotation. The duodenum also turns backwards towards the abdominal wall, and its covering with peritoneum ( peritoneum viscerale ) fuses with the peritoneum of the posterior abdominal cavity ( peritoneum parietale ) so that it is no longer covered by peritoneum (except for a small part of the pars superior ) , it is retroperitonealized secondary .
Simultaneously with the rotation of the stomach in the area of the foregut, another rotation takes place in the area of the middle and hindgut: that of the umbilical loop . The entire, loop-shaped intestinal tube rotates between the sixth and eleventh week of development in this area around an axis formed by the superior intestinal artery ( superior mesenteric artery ) and the yolk duct ( omphaloenteric duct ). Viewed from the front, the intestinal tube rotates a total of 270 ° counterclockwise. This moves the formerly upper part of the umbilical loop, the ( oral ) part facing the mouth , downwards, and the formerly lower part, the ( aboral ) part facing away from the mouth, upwards. Since the jejunum and ileum form from the part facing the mouth, and the appendix and large intestine arise from the part facing away from the mouth, this leads to the typical position of the jejunum and ileum in relation to the large intestine (the large intestine forms a frame around the ileum and jejunum). The intestinal tube grows significantly in length during this rotation, namely the mouth part of the umbilical loop significantly more than the part facing away from the mouth. The small intestine is much longer than the large intestine because of the different length growth of the part of the umbilical loop at the mouth and away from the mouth. This results in a lack of space, so that the jejunum and ileum have to lie in numerous loops between the frame of the large intestine. The first segment of the umbilical rotation (the first 90 °) takes place in the yolk sac, i.e. outside the embryo (physiological umbilical hernia). These relocated intestinal loops are only transferred back into the embryo in the tenth week of development. If this backward displacement does not take place, omphalocele occurs .
Another developmental disorder is malrotation , in which the rotation of the umbilical loop does not take place or is incomplete, with the result that parts of the intestine can come to rest in a completely atypical position. A malrotation can go completely unnoticed, but it can also lead to a volvulus or other forms of strangulation of sections of the intestine ( duodenal stenosis , superior mesenteric artery syndrome ). In addition, the lumen of the small intestine may not be continuous ( small intestinal atresia ), for example if it is closed by a membrane or is not formed along its entire length. In addition, the yolk duct cannot completely clog and form a Meckel's diverticulum .
function
Since the chyme from the stomach is extremely acidic (the pH value in the stomach is below 2), it must first be neutralized. This essentially happens in the duodenum, where a neutralizing secretion is given off (secretion).
The entire small intestine continues to be the main place of digestion and the absorption of food components ( carbohydrates , proteins , fats , vitamins , electrolytes and water ), while the ileum is also responsible for the immune defense (through Peyer's plaques ).
secretion
The acidic chyme is neutralized by means of hydrogen carbonate (bicarbonate), which is released in the small intestine by the Brunner glands of the duodenum, by the epithelial cells of the crypts and by enterocytes. In addition, alkaline, hydrogen carbonate-rich secretion from the pancreas reaches the small intestine through the two excretory ducts of the pancreas ( ductus pancreaticus and ductus pancreaticus accessoryius ) and thus contributes to the neutralization of the acid. The digestive enzymes can work optimally through the neutralization. The secretion is controlled by local reflexes that are mediated by the enteric nervous system and by various hormones such as CCK , secretin and gastrin .
In addition, the epithelial cells of the crypts secrete a liquid containing sodium chloride and the goblet cells secrete mucins , which cover the mucous membrane of the small intestine as an unstirred layer . This serves to protect the mucous membrane and as a sliding layer so that the pulp can slide past.
digestion
In principle, digestion includes the breakdown of food into its various components (more precisely: the breakdown into low-molecular compounds) and their absorption. This is done by the movements of the organs of the gastrointestinal tract, known as gastrointestinal motility , the various digestive secretions from the salivary glands, the stomach, the pancreas and the liver, and finally the digestive enzymes, which are in the digestive secretions and in the brush border of the Bowel.
Motility of the small intestine
The movements (motility) of the small intestine transport the food in the small intestine, break it up and mix it with the digestive secretions. The following describes the motility of the small intestine during the digestive phase and between the digestive phases, followed by the neural basis, which is much more complex.
In the digestive phase , segmentation and pendulum movements of the small intestine occur. This is understood to be contractions of the small intestine, which primarily serve to mix the food pulp and the contact of the food pulp with the intestinal wall and not so much to transport the food. More precisely, during segmentation movements, the circular muscles contract in neighboring areas of the small intestine, so that individual segments can be seen. Pendulum movements lead to a longitudinal displacement of the intestinal wall over the intestinal contents, triggered by contractions of the longitudinal muscles. These movements are triggered by pacemaker cells , the Cajal cells , and the frequency of the pacemaker cells in the duodenum is still 12 per minute and decreases to 8 per minute in the ileum.
The segmentation and pendulum movements are locally superimposed by a propulsive peristalsis . Propulsive peristalsis means contractions of the muscles, which lead to the fact that the food pulp is transported further, that is to the aboral (away from the mouth). To do this, the circular muscles contract orally (close to the mouth) from the food pulp and thus press it aborally. At the same time, the circular muscles relax aborally from the food pulp and the longitudinal muscles aborally contract. This leads to the intestinal lumen expanding aborally, so that space is created aborally for the food pulp and can thus be transported further. Depending on the composition of the food, the transport to the appendix takes about two to ten hours.
Several individual phases occur between the digestive phases ( interdigestive phase ): After a rest period of approx. One hour (phase 1), the small intestine contractions for about 30 minutes (phase 2). Afterwards, motor waves , MMC (Migrating Motor Complex) , migrate over the small intestine for about 15 minutes . These are powerful peristaltic waves, i.e. contractions that begin in the stomach or duodenum and end in front of the large intestine. The aim of these motor waves is to remove undigested residues from the small intestine and to prevent excessive bacterial growth. They are also triggered by the Cajal pacemaker cells and their rate is around three per minute. The motor waves are followed by a fourth phase in which the activity decreases again until finally the resting phase (phase 1) comes again. The transition from the second to the third phase seems to be controlled by the hormone motilin , while the transition from the interdigestive to the digestive phase is controlled by the vagus nerve .
At the transition from the small intestine to the large intestine is the ileocecal valve , through which about two liters of liquid small intestine content pass each day. In principle, the valve is closed and only opens when there is an increase in pressure in the ileum, the section of the small intestine in front of the valve. The contents of the small intestine then pass into the large intestine. If there is a drop in pressure in the ileum, however, it closes so that the contents of the large intestine cannot pass into the small intestine and the large intestine, which is rich in bacteria, is separated from the small intestine, which is poor in bacteria.
The following are the neural bases for small bowel motility:
Starting with the stomach, all organs have a slow basal electrical rhythm , which means that there are slow potential fluctuations in the muscles with a low frequency, so-called slow waves . In the small intestine, the frequency of these slow waves is around 12 per minute. These fluctuations in potential are triggered by pacemaker cells , the Cajal cells . They have connections to the neighboring muscle cells ( gap junctions ), via which the fluctuations in potential are passed on, and thus form a network between the circular and longitudinal muscles of the small intestine (for a description of the small intestine muscles, see Small intestine # Feinbau ). If the intestinal wall is stretched or if certain hormones or neurotransmitters are released, the potential fluctuations in the relevant section of the small intestine are much faster with greater amplitudes, the spike potentials . Depending on the frequency of these spike potentials , the wall muscles contract to different degrees.
In addition, the motility of the small intestine is controlled by nerves and hormones. There are many different hormones involved. They are released at certain times during digestion and regulate the overall process, e.g. B. when which digestive juices are released. The small intestine - like other parts of the digestive system - has its own nervous system, the enteric nervous system . It comprises two nerve plexuses : the Auerbach plexus and the Meissner plexus , which are connected to each other. The Auerbach plexus primarily regulates blood flow and motility, while the Meissner plexus controls secretion. The enteric nervous system can regulate motility completely autonomously. For example, if a section of the intestine is stretched by the contents of the intestine, this stretching is registered by sensors in the Meissner plexus and this information is passed on to the Auerbach plexus via other nerve cells, which causes the intestinal muscles to tense up from the mouth (orally) of the chyme, while the (aboral) muscles distant from the mouth relax. As a result, the food is pushed aborally, so to speak, transported further ( propulsive peristalsis ). This is also known as the peristaltic reflex .
The sympathetic and parasympathetic nervous system can intervene in the regulation of the enteric nervous system ( extrinsic innervation ). The sympathetic nervous system inhibits intestinal motility, whereas the parasympathetic nervous system promotes it. The sympathetic fibers come from the chest and lumbar sections of the spinal cord and are switched to other nerve fibers (so-called postganglionic fibers ) in ganglia (nerve cell clusters) near the spinal cord , which move to the target cells in the intestine. The transmitter for the transmission to the target cells is norepinephrine . The target cells are predominantly excitatory neurons of the enteric nervous system, but sometimes also directly muscle cells. The receptors of the muscles are α2-adrenoceptors in the longitudinal muscles (with G i as the signal-transducing G protein ) and in the circular muscles α1-adrenoceptors (with G q as the signal-transducing G protein). The parasympathetic fibers, on the other hand, come from the medulla oblongata and run with the vagus nerve to the small intestine.
Endings of some nerve fibers are exposed in the intestinal wall. These nerves act as sensors for mechanical, chemical and pain stimuli and pull with the fibers of the sympathetic and parasympathetic nervous system to the central nervous system . This can create vagovagal reflexes .
Enzymatic digestion
Food is digested enzymatically in the small intestine . This is done by digestive enzymes in the mouth (e.g. amylases ), stomach (the peptidases ) and later also in the pancreas (e.g. pancreatic lipase ). The digestive enzymes break down the carbohydrates, proteins and fats into their constituent parts, but proteins preferably not into individual amino acids , but into di- and tripeptides (molecules made up of two or three amino acids). Maltase-glucoamylase , lactase and saccharase-isomaltase act in the small intestine and break down α-1,4-glycosidic bonds in the carbohydrate chains. This means that the carbohydrates are broken down into their simple sugars ( monosaccharides ). These enzymes are located in the membranes of the small intestine cells of the brush border and are therefore part of membrane-associated digestion.
The pancreatic enzymes enter the duodenum through the pancreatic duct via the major duodenal papilla . The bile is used to emulsify the fats (see absorption of fats). In addition, bilirubin and other substances that are to be excreted are added to the bile and thus excreted. In contrast, around 95% of the bile acid is absorbed and made available to the liver again.
Absorption of food in the small intestine
The small intestine is primarily responsible for the absorption of carbohydrates , proteins and fats - water and electrolytes are also absorbed in the large intestine . The uptake of nutrients is facilitated by the large surface area of the small intestine and mainly takes place via transport processes into the enterocytes. To do this, the enterocytes create a difference in concentration, a gradient of sodium and potassium in relation to their surroundings. This gradient is the driving force to transport food components into the small intestine cells. A distinction is made between two forms of substance uptake: transcellular transport and paracellular transport . Transcellular transport means uptake via special transport proteins. This means that these special transport proteins transport the substances into the cell, possibly against their gradient (concentration gradient). Paracellular transport, on the other hand, takes place along a gradient between the cells.
Carbohydrate intake

Carbohydrates can only be consumed as simple sugars ( monosaccharides ). Most of it is absorbed in the duodenum and jejunum - a small part reaches the large intestine and is metabolized by local bacteria. There are two transport proteins for the absorption of the monosaccharides:
- Glucose and galactose are taken up in the enterocytes together with sodium (sodium symport) via the transporter SGLT1 ( sodium glucose transporter 1 ). Sodium follows its gradient into the cells and drives the transport of glucose / galactose.
- Fructose gets into the cell via facilitated diffusion through the transporter GLUT5 ( glucose transporter 5 ), that is, the transporter facilitates the "flow" of fructose, but does not take over active transport.
All three sugars then enter the blood through the GLUT2 ( glucose transporter 2 ) transporter . The driving force for the transport into the blood is the gradient: In the enterocyte the concentration of the three monosaccharides is comparatively high and in the blood comparatively low, so that the monosaccharides can easily diffuse into the blood.
Uptake of proteins
In principle, proteins also have to be split into their amino acids or into di- or tripeptides before they can be absorbed. While infants can still ingest undigested proteins in significant numbers via endocytosis , this mechanism is practically insignificant in adults. Overall, about 80 to 90% of the proteins are absorbed in the duodenum and the jejunum; only 10% reach the colon, where it is metabolized by bacteria. Ultimately, over 96% of the nitrogen contained in food (mainly in proteins) is absorbed.
- Individual amino acids reach the enterocytes via various sodium symporters and leave them again via facilitated diffusion and enter the blood.
- Di- and tripeptides are taken up into the cell by the transporter PepT1 together with a proton . In the cell, the di- and tri-peptides are then mainly split into individual amino acids and leave the cell via facilitated diffusion into the blood. A few di- and tri-peptides can also get into the blood without being split.
- The gradient of protons required for the PepT1 transporter is built up by the transporter NHE3 , which transports protons from the cell into the lumen of the small intestine and sodium ions from the lumen of the small intestine into the cell. Since the sodium gradient required for this is in turn built up by the sodium-potassium ATPase, the transport of di- and tripeptides is a tertiary active transport.
Absorption of fats
The majority (approx. 95%) of dietary fats are absorbed in the duodenum and jejunum, some short-chain fatty acids also in the colon. Only about five to seven grams of fat are excreted in the stool with an average diet. Enzymes in saliva ( tongue base lipase ), stomach ( gastric lipase ) and pancreas ( pancreatic lipase ) break down fats, fatty esters and cholesterol esters into cholesterol , monoglycerides , fatty acids and lysophospholipids (lipolysis), which can be absorbed by the small intestine. The above-mentioned cleavage products form so-called mixed micelles with the bile acids from the bile . The micelles also contain triacylglycerides and fat-soluble vitamins and phospholipids. However, all dietary fats are only effectively absorbed if they have been broken down into the lipolysis products mentioned above. Glycine as well as short and medium-chain fatty acids can also be absorbed without having formed micelles.
For absorption, the micelles come into contact with the enterocytes of the small intestine, disintegrate and release the split fats. These are then taken up in the enterocytes by mechanisms that have not yet been adequately clarified. Long-chain fatty acids, cholesterol, monoglycerides and lysophospholipids are probably mainly absorbed via transporters. Glycerine and short and medium-chain fatty acids, on the other hand, can diffuse freely into the enterocytes. In the cell plasma of the enterocytes, the fatty acids are activated by transferring them to coenzyme A and transported together with the other lipolysis products to the smooth ER , where the triacylglycerides are formed again, cholesterol is re-esterified and lysophospholipids are converted back into phospholipids. The triglycerides, cholesterol esters and phospholipids then combine with fat-soluble vitamins and apolipoproteins from the rough ER to form chylomicrons . These are then released to the lymph , from where they enter the breast duct and ultimately the blood in the left vein corner . Glycerine and the short- and medium-chain fatty acids get from the enterocytes directly into the blood and on to the liver.
Intake of vitamins
All fat-soluble vitamins ( vitamin A , vitamin D3 , vitamin E and vitamin K ) are absorbed together with the fats in the micelles (see absorption of fats). There are specific transport proteins for the water-soluble vitamins:
- Vitamin C , vitamin H (biotin) and vitamin B5 (pantothenic acid) get into the enterocytes together with sodium via a sodium symporter.
- Vitamin B3 (niacin) is absorbed through an H + symporter.
- Transport proteins also exist for vitamins B1 and B2 .
- Vitamin B6 enters the enterocytes through a channel (facilitated diffusion).
- Vitamin B9 (folic acid) is hydrolytically split off from folate polyglutamate as folate monoglutamate and absorbed by a folate monoglutamate / OH - antiporter. The hydrolysis of folate polyglutamate is catalyzed by the brush border peptidases.
- Vitamin B12 : In the ileum, the intrinsic factor vitamin B 12 ( cobalamine ) from the stomach is absorbed through receptor-mediated endocytosis . To do this, it is coupled to the intrinsic factor.
Absorption of water
Every day around six liters of fluid are absorbed in the small intestine (of the original eight liters that got into the small intestine). The large intestine absorbs about two liters of water again, so that only about 100 ml are excreted per day. The maximum possible water intake of the small intestine is around 15 to 20 liters of water per day. The absorption itself takes place paracellularly and transcellularly and is linked to the transport of water-soluble substances (such as sodium). The water basically follows the osmotic pressure gradient. The amount of water absorbed decreases continuously towards the large intestine. The reason is the increasing tightness of the cell connections with each other (the tight junctions ).
Absorption of minerals
-
Sodium : Of the approximately 30 g of sodium per day that enter the intestine (25 g from digestive juices and 5 g from food), around 75% is absorbed in the small intestine and 24% in the large intestine; only about 1% is lost. The absorption occurs both para- and transcellularly:
- Sodium is ingested with carbohydrates or amino acids (see sections above)
- In the duodenum and jejunum, there are Na + -H + - antiporter (such as NH3 transporter), the sodium into the cell and transport a proton into the small intestinal lumen. These transporters are stimulated by hydrogen carbonate (bicarbonate), which is particularly found in the secretions of the bile, pancreas and the small intestine itself.
- Between the digestive phases, the transport through parallel working Na + / H + and Cl - / HCO 3 - antiporters in the ileum becomes more important. These transport systems make up the largest proportion in quantitative terms.
- Paracellular transport: In the duodenum and jejunum, the connections between the cells are relatively weak and water can easily flow through between the cells. It pulls along smaller dissolved molecules (solvent drag)
- Chloride is transported paracellularly (like sodium) in the duodenum and jejunum. In the ileum, transport takes place mainly via the aforementioned Cl - / HCO 3 - antiporter.
- Potassium is paracellularly absorbed in the jejunum and ileum.
- Calcium : Approx. 1 g of calcium is absorbed daily, but at the same time about 325 mg are released with the digestive secretions. With an intake of around 500 mg calcium, the actual increase in calcium is only 175 mg per day and the majority is excreted in the stool. In the duodenum there is an active Ca 2+ transporter that pumps calcium into the cell, where it is bound to calbindin and then released into the blood via a 3Na + / Ca 2+ antiporter or a Ca 2+ -ATPase. This active form of absorption is stimulated by vitamin D3 . Most of the calcium is, however, absorbed passively, i.e. paracellularly, in the ileum and jejunum.
- Magnesium is passively absorbed in the duodenum and actively absorbed in the jejunum. Overall, about 30-40% of the 300–400 mg administered approximately daily is absorbed and the rest excreted. Some of the magnesium, like calcium, comes from digestive juices.
- Phosphate: Organic phosphates must first be hydrolyzed before they can be absorbed. Then they are absorbed like the approx. 1 g of inorganic phosphate via a Na + symporter. The absorption is also stimulated by vitamin D3.
- Sulphate is absorbed in the empty intestine and ileum as inorganic sulphate (SO 4 2− ) via a Na + symporter. There also seem to be other relevant sulfate transporters. Otherwise sulfur is absorbed as a component of the amino acids cysteine and methionine .
- Copper is absorbed in the stomach and duodenum. The total absorption is about 10% of the copper contained in food. The exact mechanism of absorption is not known. It is then released into the blood and bound to albumin and transcuprein and thus reaches the liver.
- Zinc is absorbed in the empty and ileum. The absorption is about 10–40%. Zinc is also bound to albumin in the blood.
- Manganese is also absorbed in the small intestine and then transported to β1- globulin in the blood.
- Cobalt : Although the absorption is 70–100%, it is quickly excreted in the urine.
- The absorption of fluoride is as effective as that of cobalt. It is almost exclusively built into bones and teeth and otherwise excreted with the urine.
- Also, selenium , molybdenum and chromium are needed by the body. Selenium is absorbed between 50 and 100%.
- Although they have no function and are toxic in higher doses, the body also takes in cadmium , lead and mercury , as these are found in food.
Absorption of iron
Iron absorption is relatively inefficient at around 10–20%. An average of 10–15 mg of iron is ingested with food every day, meaning that only 1 to 1.5 mg is absorbed. However, if there is an increased need (e.g. during pregnancy), the efficiency can increase up to 40%. There are two mechanisms:
- Free iron can only be absorbed as Fe 2+ . Therefore, Fe 3+ is first reduced to Fe 2+ by ferric reductase and by means of free SH groups and vitamin C. Some substances such as tannic acid (tea), phosphates (e.g. in egg yolk), etc. a. inhibit resorption. In the duodenum, the Fe 2+ then enters the cell via the DMT1 transporter together with a proton.
- Heme- bound iron is split off from the protein by the heme carrier protein 1 and transported into the cell. There it is reduced to Fe 2+ by the haem oxygenase and then Fe 2+ is released from the haem. Thus, as with free iron, there is now free Fe 2+ in the cell.
In both cases , the Fe 2+ is bound to mobilferrin , which transports it to the basolateral side of the cell. The cell is connected to the blood on this side. Fe 2+ is oxidized there again by Hephaestin to Fe 3+ , which is transferred to the blood by the IREG transporter . Hephaestin and IREG bind a common complex. In the blood, Fe 3+ binds to apotransferrin - the transport protein for iron in the blood.
Iron can also be stored in the mucosal cell as ferritin and is then excreted when the cell falls into the intestinal lumen ( desquamation ). The excretion is very low at 1–2 mg per day, however, and therefore excessive absorption can also lead to an iron overdose ; however, iron deficiency is much more common.
Examination options of the small intestine
- Anamnesis (ask about complaints)
- Auscultation (listening to the intestines), palpation (feeling the abdomen)
- Ultrasound of the small intestine, mesentery and its vessels
- Biopsy from the duodenum
-
Blood tests
- Signs of inflammation
- Absorption deficiency signs
- Stool exams
- on germs
- on chymotrypsin
- on stool fat content
- X-ray - abdomen overview (of the abdomen)
- X-ray with contrast medium passage (to better visualize the bowel)
- X-ray - double contrast examination of the small intestine according to Sellink
- CT or MRI of the abdomen (abdomen)
- Reflection of the duodenum
- Capsule endoscopy
- Terminal ileum colonoscopy (ileoscopy)
- oral push enteroscopy
- Double or single balloon enteroscopy of the small intestine (push-and-pull)
- Small bowel manometry
Diseases of the small intestine
- Crohn's disease
- Meckel's diverticulum
- Duodenal ulcer (duodenal ulcer)
- Small intestinal atresia
- bacterial overgrowth in the small intestine
- Whipple's disease
- Volvulus
- Intussusception
- Duodenal diverticulum
- Food intolerance (e.g. celiac disease , lactose intolerance , wheat allergy )
- Fungi (e.g. Candida albicans )
- Parasites
Signs of illness
There are several symptoms that can occur with diseases of the small intestine. Different diseases can cause diarrhea through different mechanisms . Even constipation can have various causes. Behind an ileus , called intestinal obstruction in German, either an actual mechanical obstacle (mechanical ileus) or a paralysis of the intestine (functional ileus) can be concealed. Bleeding of the small intestine most often arises on the bottom of inflammatory processes and from ulcers . Other non-specific signs of illness are abdominal pain , which as a rule cannot be localized to a specific section of the intestine, as well as unwanted weight loss and malnutrition .
Tumor diseases
Tumors of the small intestine are rare in humans, they only make up about 3% of all tumors of the digestive organs. There are no characteristic symptoms : the tumors can cause cramping abdominal pain, secrete blood or, as they grow, narrow the lumen of the small intestine. Most of these tumors are benign . They usually start from the glandular epithelium, making them adenomas that can also form polyps . There are also leiomyomas (tumors of smooth muscle cells), lipomas (tumors of fat cells) and angiomas . Malignant cancer is very rare, but is more common in people with Crohn's disease , celiac disease, or AIDS . The malignant tumors also mostly originate from the gland cells (adenocarcinomas), this group makes up about half of the malignant small intestinal tumors. About every fifth malignant tumor is a manifestation of a lymphoma . There are also carcinoid tumors , most commonly found in the distal ileum , as well as gastrointestinal stromal tumors and leiomyosarcomas . Papillary tumors affect the small intestine, but are not actually small intestine tumors , as they originate from the biliary or pancreatic duct .
Treatment methods of the small intestine
- Sufficient fluid, salt and sugar substitutes for diarrhea
- Food leave
- parenteral nutrition
- Rinsing with physiological saline solution
- Antibiotic therapy
- surgery
- Cortisone
- Diet without certain food components (gluten, lactose, etc.)
- Visceral osteopathy
literature
- Franz-Viktor Salomon: Gut, Intestinum (Enteron) . In: Salomon u. a. (Ed.): Anatomy for veterinary medicine . Enke-Verlag Stuttgart, 2nd ext. 2008, pp. 293-311, ISBN 978-3-8304-1075-1 .
- Gerhard Aumüller et al .: Dual Series Anatomy , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 .
- Giulia Enders ; Jill Enders (illustrations): Gut with charm. All about an underrated organ . Ullstein, Berlin 2014, ISBN 978-3-550-08041-8 (paperback) / ISBN 978-3-550-08108-8 (hardback).
- Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 .
- Renate Lüllmann-Rauch: pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 .
Web links
Individual evidence
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 628.
- ↑ a b Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 628 f.
- ↑ a b Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , pp. 628-631.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . Georg Thieme Verlag, 2nd edition 2006, ISBN 978-3-13-129242-1 , p. 375.
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 631.
- ↑ Kuno Weise (Ed.): Surgery: Cut for Cut . Georg Thieme Verlag 2004, ISBN 978-3-13-130841-2 , p. 582.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 , pp. 411-413.
- ↑ a b Renate Lüllmann-Rauch: Pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 , p. 424.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 , pp. 425-428.
- ↑ Renate Lüllmann-Rauch: Pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 , p. 429f.
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 626.
- ↑ a b c Renate Lüllmann-Rauch: Pocket textbook histology . 5th edition. Georg Thieme Verlag, Stuttgart 2015, ISBN 978-3-13-129245-2 , p. 431.
- ↑ a b Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 630.
- ↑ Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 , pp. 217 and 276.
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 632 f.
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , p. 633.
- ↑ Gerhard Aumüller et al .: Duale Series Anatomie , 2nd edition. Georg Thieme Verlag, Stuttgart 2010, ISBN 978-3-13-152862-9 , pp. 631, 633 and 786, 787.
- ↑ Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart · New York, 2015, ISBN 978-3-13-139534-4 , pp. 40–42.
- ↑ Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 , p. 42.
- ↑ Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 , pp. 43f.
- ↑ Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 , p. 46.
- ↑ a b Pathology of the midgut . In: embryologie.ch (accessed on May 19, 2016).
- ↑ a b Michael Schünke et al .: Prometheus - Learning Atlas of Anatomy. Inner organs , 4th edition, Georg Thieme Verlag, Stuttgart New York, 2015, ISBN 978-3-13-139534-4 , p. 49.
- ^ Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 495.
- ^ Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 504.
- ^ Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 503.
- ↑ a b Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 477.
- ^ Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . Pp. 482 and 485.
- ↑ Intestinal motor skills . In: Spektrum.de , 1999, Spektrum Akademischer Verlag, Heidelberg. (last accessed on February 16, 2017).
- ↑ a b c Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 485.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 486.
- ↑ a b Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 479.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , pp. 480 and 481.
- ↑ a b c Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 480.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 565.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 571.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , pp. 477, 504.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , pp. 496 f., 500 and 502.
- ↑ a b c d e Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 506.
- ↑ a b c Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 508.
- ↑ a b c d Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 507.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , pp. 500 and 506.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 508 f.
- ↑ Jan C. Behrends et al .: Dual Series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 470.
- ↑ a b c d e f g h Jan C. Behrends et al .: Dual series Physiology . 3. Edition. Georg Thieme Verlag, Stuttgart 2017, ISBN 978-3-13-138413-3 , p. 511.
- ↑ Michael Gekle et al. a .: Physiology . 1st edition. Thieme-Verlag, Stuttgart 2010, p. 466.
- ↑ a b c d e f g Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 510.
- ↑ a b c d e Jan C. Behrends et al .: Dual Series Physiology , 3rd edition. Georg Thieme Verlag, Stuttgart, 2017, ISBN 978-3-13-138413-3 . P. 509.
- ↑ Joachim Rassow , Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 332.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 328.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 329.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 330.
- ^ A b Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 331.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 333.
- ^ A b Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 334.
- ↑ Claus Leitzmann, Claudia Müller, Petra Michel, Ute Brehme, Andreas Hahn, Heinrich Laube: Nutrition in Prevention and Therapy. A textbook. 2nd Edition. Georg Thieme Verlag, 2003, ISBN 3-8304-5273-X , p. 76.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 323.
- ↑ a b c Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Series Biochemistry , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . P. 324.
- ↑ Joachim Rassow, Karin Hauser, Roland Netzker and Rainer Deutzmann: Dual Biochemistry Series , 4th edition. Georg Thieme Verlag, Stuttgart, 2016, ISBN 978-3-13-125354-5 . Pp. 324-327.
- ^ Robert J. Mayer: Malignant tumors of the gastrointestinal tract . In: M. Dietel, N. Suttorp, M. Zeitz (eds.): Harrisons Innere Medizin, Volume 1 , ABW-Wissenschaftsverlag, Berlin 2012, ISBN 978-3-940615-20-6 , pp. 818-831, here P. 329 f.