Retina

1. sclera (sclera)
2. choroid ( choroid )
3. Schlemm's canal ( sinus venosus sclerae )
4. Arterial vascular ring ( arterial circle iridis major )
5. cornea ( cornea )
6. iris ( Iris )
7. pupil ( pupilla )
8. anterior chamber ( camera anterior bulbi )
9. posterior chamber ( camera posterior bulbi )
10. ciliary body ( corpus ciliare )
11. lens ( lens )
12. vitreous body ( corpus vitreum )
13. retina ( Retina ) and pigment epithelium
14. Optic nerve ( Nervus opticus )
15. Zonular fibers ( Fibrae zonulares )
Outer skin of the eye ( Tunica externa bulbi ): 1. + 5.
Middle skin of the eye ( Tunica media bulbi ): 2. + 6. + 10.
Inner eye skin ( Tunica interna bulbi ): 13.
The retina , retinal (from latin rete , Power ') or inner eye skin is multi-layered, the specialized nerve tissue, the inside of the eye of vertebrates , some squid , and snails lining. In the retina, the incident light is converted into nerve impulses after it has passed through the cornea , the lens and the vitreous humor . The layer of light-sensitive sensory cells ( photoreceptors ) lies on the inside of the darkening retinal pigment epithelium . Their impulses are processed and passed on in further layers of nerve cells that follow inward. In addition, the retina contains various supporting and supplying structures.
Put simply, the retina becomes a kind of projection surface for the image of our surroundings, similar to a screen or a light-sensitive film, and transmits the stimuli caused by light stimuli to regions of the brain.
Anatomy of the human retina
Direction and location designations
As far as the layers of the retina are concerned, the outer side of the retina that is closer to the outer wall of the eyeball is called outer. The side closer to the center of the eyeball is referred to as the inside . The light that penetrates the eyeball through the pupil first reaches the inner layers of the retina and only then the outer layers; the outermost layer of the retina is made up of a layer of dark pigmented cells, the retinal pigment epithelium .
As forward , anterior or distal , is called the retina portions which are close to the structures of the anterior chamber, the iris and the lens. Back , posterior or proximal , are called retinal parts on the wall of the eyeball opposite the lens. For the indication of directions in the transverse axis, the expressions nasal ( nasal ) and temple ( temporal ) are used.
Sections and Borders
By far the largest part of the inner surface of the eyeball is the pars optica retinae, called the neuroretina , which carries the photoreceptors . Towards the front, it is about 3 mm behind the ciliary body ( corpus ciliare ) with a jagged border, the ora serrata , separated from the pars caeca retinae (Latin caecus 'blind'), which covers the ciliary body at the very front as the pars ciliaris retinae . The anterior retinal sections can be viewed in the intact eye during the contact lens examination with a three-mirror contact lens .
The retina is located outside the choroid ( choroidal on) that by diffusion provides the outer layers of the retina with nutrients. Inside the retina lies the vitreous body ( corpus vitreum ). At the rear, the retina merges into the optic nerve ( nervus opticus ) in the optic nerve papilla , which contains the nerve fibers of the ganglion cell layer .
The so-called blood-retina barrier serves to protect the retina .
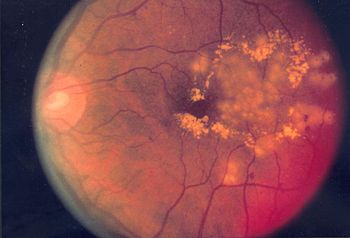
Macroscopic image of the retina, fundus
When looking at the fundus of the eye ( fundus oculi or fundus ) through the pupil , one looks through the colorless and transparent neuroretina at the darkly pigmented retinal pigment epithelium (RPE) and the underlying choroid, which is more or less darkly pigmented depending on the type. A noticeable landmark is the exit point of the optic nerve with its papilla ( papilla nervi optici ) about 15 ° nasally from the optical axis . Its pink to light red color makes it stand out from the rest of the brown orange of the fundus. The papilla has an average diameter of about 1.5 mm and is round or oval shaped with individually differently pronounced edges.
The blind spot
The blind spot is the point in the field of vision onto which the optic nerve papilla is projected (about 15 ° on the temple side from the fixation point). There are no light receptors where the nerve fibers of ganglion cells of the inner layer converge and pass through all the layers of the retina and leave the eyeball to form the optic nerve (see below). The area of the optic nerve papilla is really insensitive to light, "blind".
The fact that this “blind” spot is not perceived even with one-eye vision is due to the so-called complementary effect . The visual system uses information provided by the receptors around the papilla to complement the image.
Vessels of the retina, macula lutea
The large retinal vessels, the arteriola and venola centralis retinae , which contribute significantly to the ocular blood flow , also pass through the eyeball wall and pass through the center of the papilla. Here they branch into an upper and a lower tuft and usually divide again into a nasal and a temple-side branch. The arterioles can be distinguished from the venules by their different shades of red and their caliber .
The vascular branches on the temporal side arc around a vascular-poor and vascular-free area in the center, which represents the yellow spot ( macula lutea ). The yellowish color of this area of the retina with a diameter of around 3 mm is caused by the carotenoids lutein and zeaxanthin stored here . These filter high-energy (UV) light and protect the retinal cells from photo-oxidative damage. The middle of the macula lutea is a shallow recess, the fovea centralis , short fovea or fovea called; around the fovea centralis the retina is thickened into a flat wall. This surface shape is by deflection of retinal layers and can materialize at mirroring the fundus of reflections, called Wall reflex, are detected.
The pit of vision in the “yellow spot” contains the point of sharpest vision. This is where the retina has the greatest resolution, such as that needed when reading small print. The surrounding retina has a lower resolution ; These peripheral retinal regions essentially serve to perceive the environment, to recognize things "from the corner of the eye", and are the basis of the peripheral visual field . The central retina with the fovea centralis represents in the foveola with its center as the motor zero point the direction value straight ahead, also called the main viewing direction . Each peripheral retinal point has a different sense of direction, which leads to a correspondingly large number of secondary directions .
Severe damage to the macula lutea, e.g. For example, age-related macular degeneration (AMD) can lead to significant loss of visual acuity , so that it is no longer sufficient for reading or driving a car, for example.
Retinal nerve cells

v. l. Right: white: ganglion cells and their axons, gray: inner plexiform layer, white: amacrine cells, bipolar, horizontal cells, yellow: outer plexiform layer, white: photoreceptors, light brown: photoreceptors outer segments
A cross-section of the retina shows a conspicuous stratification in the light microscope , which is formed by alternating layers with and without nuclei. The layers have characteristic cell types and subcellular compartments. The nerve cells of the retina can be divided into three groups:
- The light-sensitive or photoreceptive cells that convert incoming light into nerve impulses. These include the rods and cones and possibly other cell types.
- The intermediate cells or interneurons, which subject the generated impulses to an initial processing within the retina. These include the horizontal cells , the bipolar cells and the amacrine cells .
- The ganglion cells , which forward the processed information to the next switching point outside the retina.
As a result of evolutionary development, according to which the retina of a protuberance of the diencephalon has been formed, it is inversely constructed, since the actual light-sensitive cells are in the outer layers, which are remote from the light most.
Photoreceptors
The photoreceptor cells are of particular importance among the cells of the retina because they represent the actual light-sensitive cell type. The photoreceptor cells are highly polar cells, which consist of an outer segment, an inner segment, the cell body and an axon with a complex synapse . Basically, one differentiates in the retina of the vertebrate photoreceptor cells according to their structure in two types, rods and cones ( English rods and cones ), which are distributed in a mosaic. The rod cells are used for vision in weak lighting ( scotopic vision ), the cone cells, represented by three different types in humans, the color vision ( photopic vision ). There are around 120 million rods and around 6 million cones in the human eye, but not evenly distributed. In the center of the yellow spot ( macula lutea ) is located in the fovea ( fovea centralis ), the region of maximum visual acuity; Here the cone cells are particularly densely packed at around 150,000 per square millimeter, while rod cells are absent. However, these reach a similarly high density in a ring-shaped area at the macular edge; towards the retinal periphery their number decreases to around 35,000 / mm 2 , with cones occurring around ten times less often here. A third type of light-sensitive nerve cells are the photosensitive ganglion cells , which contain the light-sensitive protein melanopsin . These cells help to synchronize the internal clock with the day-night rhythm, to suppress the hormone melatonin and to control the size of the pupil .
Humans are trichromats : They have three types of cones with different absorption maxima . In simple terms, one can say that there are red-sensitive , green-sensitive and blue-sensitive cones. The nervous system combines the signals from the three types of cones to assign a color to light in a specific spectral distribution . The cones are less sensitive to light than the rods. Therefore, the perception of color changes at night, the so-called Purkinje effect . Hence the saying is true: At night all cats are gray (for Note: with the S täbchen one sees beautiful warz / white, with the Zap f s F arben).
A single light particle ( photon ) can activate a rod. However, several rods have to be activated for the retina to signal the presence of light. When a photon hits the visual pigment rhodopsin , which is embedded in the membrane stack of the photoreceptors , the latter undergoes a conformational change . This triggers an enzyme cascade , the so-called visual signal transduction cascade , which ultimately leads to a change in the activity of the nerve cell (cones like rods). The American biochemist George Wald received the Nobel Prize for Medicine in 1967 for clarifying the importance of the retinal 1933–1958 .
Possibly a third group of light sensory cells belongs to the photoreceptors; these contain the pigment melanopsin . This cell type was only discovered recently and is still relatively unexplored. It has been proven that the melanopsin cells act as photoreceptors and play an important role in the function of the "internal clock". They send signals to the ( nucleus suprachiasmaticus ), in which circadian rhythms are generated and time information is passed on to the body (see chronobiology ). According to new findings, these ganglion cells are also responsible for the pupillary reflex .
Horizontal cells, bipolar cells, amacrine cells

The photoreceptors interconnect two different types of horizontal cells. You yourself are in contact with neighboring cells via gap junction . Horizontal cells serve u. a. for contrast enhancement through lateral inhibition of neighboring photoreceptors.
The bipolar cells are innervated by the photoreceptors. In the mammalian retina, there are eight to twelve types of bipolar cells that contact cones (cone bipolar cells) and one bipolar cell type that makes contact with rods (rod bipolar cells), depending on the species. A distinction is made between ON and OFF bipolar cells. ON bipolar cells depolarize in response to a light stimulus, whereas OFF cells react with hyperpolarization.
The bipolar cells innervate the amacrine cells . Amacrine cells - similar to the previous horizontal cells - ensure both lateral and vertical interconnection of the neural network in this layer of the retina and also contribute to the modulation of signal processing. There are over 30 different types of amacrine cells in total. One type, the so-called A2 amacrine cell, forwards signals from rod bipolar cells to the cone bipolar cells, thereby coupling these two signal paths. Another type of amacrine cell, the so-called starburst cell, is involved in motion vision.
Ganglion cells
Downstream of the bipolar and amacrine cells are the ganglion cells. They are the output neurons of the retina and convey the visual information via the optic nerve (nervus opticus) to the next switching station in the brain, the corpus geniculatum laterale . A total of at least 30 ganglion cell types can be distinguished.
Layers of the retina

The light entering through the pupil penetrates the lens and vitreous body as transparent media and then passes through several layers of the retina before it is detected by the photoreceptor cells of the neuroepithelium, which face the pigment epithelium on the outside. From the vitreous to the choroid, i.e. from the inside to the outside in relation to the eye, the light-sensitive retina shows a layer-like structure of cell bodies alternating with cell processes. Usually ten layers can be distinguished, in the area of the visual pit of the yellow spot some are shifted sideways.
Epiretinal membrane (ERM), or inner boundary membrane
The internal limiting membrane ( Membrana limitans interna ), English epiretinal membrane (ERM) or internal limiting membrane (ILM) , separates the retina from the vitreous humor. This inner boundary of the retina is formed by the basement membrane and the plasma membrane of Müller's cells and possibly other glial cells . In addition, it consists of collagen fibers and proteoglycosides . The layer, which appears homogeneous in the light microscope, covers the entire retina and merges into the zonal lamella with a somewhat coarser structure .
The older histologists were of the opinion that the brush-like end feet of the Müllerian supporting fibers are firmly anchored in the boundary membrane, so that the latter is to be assessed as a glious product. However, the electron microscope was able to show that the inner boundary membrane has the character of a basement membrane and can be clearly delimited from the base points of Müller's cells. The clinically demonstrable strong adhesion of the membrane to the retina is probably due to the intermediate layer filled with cement substance, which connects the glial processes of Müller's cells with the boundary membrane.
The inner boundary membrane is also understood as the peripheral compression of the vitreous tissue, as its fiber lamellae rise in layers from the retina and merge into the vitreous membrane. The thickness of the boundary membrane is approx. 2-3 µm.
Nerve fiber layer
The nerve fiber layer ( Stratum neurofibrarum ), English nerve fiber layer (NFL) , consists of nerve fibers with the axons of the ganglion cells and increases in thickness towards the blind spot . They each conduct the signals of a retinal ganglion cell with the processed information from photoreceptors of a circumscribed retinal area to different brain regions. The nerve fiber layer of an eye contains about 1 million ganglion cell axons in humans. In his case, these nerve fibers are medullary and receive their myelin sheaths only when they exit the globe at the discus nervi optici , the optic nerve papilla . Destruction of a portion of the nerve fiber layer, for example through pressure damage in glaucoma , results in irreparable blindness in the affected retinal area.
In the foveola of the fovea centralis , the nerve fiber layer is smallest because it is shifted sideways. From the wall of the optic pit, axons start in a star shape and then move in a more or less pronounced arc to the exit point of the optic nerve ( papilla ). They converge between the fovea and papilla and thus form the maculopapillary bundle . All other ganglion cell axons arc around this bundle either above or below. They never cross the horizontal center line ( Rhaphe ).
The nerve fibers of the anterior retina, the ganglion cell bodies of which are furthest away from the papilla, run furthest outside in the fiber layer. So when they pull towards the papilla, they stay outside and therefore also take a more peripheral position in the optic nerve. The axons of the ganglion cells, which are closer to the papilla, run closer to the surface in the NFL, so they also come to lie more centrally in the optic nerve.
Centrifugal fibers - from the brain to the retina - have also been described variously in the nerve fiber layer. However, their function and significance are uncertain. Some authors assign them inhibitory functions in the act of vision, others associate them with the vascular innervation of the retinal vascular network.
The branches of the central blood vessels of the retina also run in the nerve fiber layer and the adjacent ganglion cell layer. Neuroglial cells are also present in this layer and scattered ganglion cells can be found. The thickness of the nerve fiber layer is approx. 20–30 µm.
Ganglion cell layer

legend on the left side:
RPE Retinal pigment epithelium
OS outer segments of the photoreceptor cells
IS inner segments of the photoreceptor cells
ONL outer nuclear layer
OPL outer plexiform layer
INL inner nuclear layer
IPL inner plexiform layer
GC ganglion cell layer
legend on the right side:
BM Bruch's membrane, P pigment epithelial
R Rods, C cones
Arrow: Membrana limitans externa
H horizontal cell , bi bipolar cell
M Müller cell, A amacrine cell
G ganglion cell, ax axons Incidence of
light from inside (below, GC) to outside (above, RPE)
The ganglion cell layer ( Stratum ganglionare ), English ganglion cell layer (GCL) , contains the cell bodies of the retinal ganglion cells .
The dendrites of the ganglion cells move into the adjacent inner plexiform layer (IPL), where they branch out and receive the signals from the bipolar cells and the amacrine cells. The signals are then passed on to regions in the brain via the axons of the ganglion cells, which run in the nerve fiber layer and bundle to form the optic nerve .
The size of the cell bodies is different, the arrangement of the cells in the peripheral retina is usually single-layered, in the middle and central zones multilayered. In addition to ganglion cells, some types of amacrine cells ('displaced amacrine cells') and glial cells can be found in the GCL . The thickness of the GCL is approx. 20–30 µm.
Inner plexiform layer
In the inner plexiform layer ( Stratum plexiforme internum ), English inner plexiform layer (IPL) , a stage of preprocessing takes place before the information is passed on, for example, to visual centers in the brain.
The IPL consists of a dense network formed by the axon terminals of the bipolar cells and by the dendrites of the amacrine cells and ganglion cells. The bipolar cells deliver processed signals from the photoreceptors from the outer retinal layers. The IPL can be divided into five sub-layers. This structure results from the interconnections of the bipolar cells. The tonic OFF bipolar cells form synapses in the first sublayer of the IPL. The phasic OFF bipolar cells interconnect in the second. The phasic ON bipolar cells interconnect in sublayer four and the tonic ON bipolar cells in the fifth.
The signal transmission is modulated by synaptic interactions with amacrine cells and finally reaches the retinal ganglion cells.
Occasionally found in the IPL and cell body of "misplaced" ( misplaced as well) neurons, neuroglia. The thickness of this layer is about 50-70 µm.
Inner granular layer
The inner nuclear layer ( Stratum nucleare internum ), English inner nuclear layer (INL) , contains the cell bodies of functionally very different cells.
The cell bodies of bipolar, amacrine and horizontal cells for the preprocessing of signals are located in the INL, as are the cell bodies of the neural supporting tissue, the Müller cells. The horizontal cells are furthest out, followed by the cell bodies of the bipolar cells and Müller cells, the amacrine cells are located on the inner boundary. Within the macula in the wall around the visual pit, the INL is particularly thick with a dozen rows of cells; it tapers peripherally to a two- to three-row arrangement of cell nuclei. The thickness of the inner granular layer is 30 µm.
Outer plexiform layer
The outer plexiform layer ( Stratum plexiforme externum ), English outer plexiform layer (OPL) , creates the connection between the photoreceptors and the downstream cells.
The dendrites of the bipolar and horizontal cells are connected to the synaptic ends of the photoreceptors and thus form the first stage of intraretinal information processing. This layer also contains the extensions of the Müllerian supporting fibers. In the transition zone to the next layer lies the deeper supply network of the retinal capillaries, which are descendants of the central retinal artery. These vessels run very constantly in one plane and hardly penetrate into other layers. The thickness of this layer is about 20 µm.
Outer granular layer
The outer nuclear layer ( stratum nucleare externum ), English outer nuclear layer (ONL) , the layer of the cell bodies of the photoreceptors.
The cell bodies of the rods and cones are grouped parallel to each other in the ONL and their thickened light-sensitive processes, the outer segments, extend in the direction of the RPE. The cores of the cones lie in a single layer near the boundary membrane, those of the rods form 4 to 6 layers. An exception to this arrangement is in humans in the fovea region, in which cones are also stored in multiple layers.
It should be noted in particular that there are significantly more cell nuclei in this layer than in the layer of bipolar and ganglion cells. The thickness of this layer is about 40 µm.
Outer boundary membrane (ÄGM)
The outer limiting membrane ( Membrana limitans externa ), English external limiting membrane (ELM) , is a largely impermeable separating layer, also called Stratum limitans externum .
It is formed by a horizontally located row of cell adhesion connections ( zonulae adhaerentes , adhering junctions ), which are formed between the outgrowths of Müller's cells and the photoreceptor cells. The inner members of the receptor cells pass through the gaps in this fibrillar network. In the region of the ora serrata, the outer boundary membrane continues into the substance that connects the two layers of the ciliary epithelium.
Inner segment (IS)
The inner segment or inner member, English inner segment (IS) , consists of metabolically rich compartments of the photoreceptors.
The IS is the area of photoreceptor cells that contains mitochondria and endoplasmic reticulum (ER). Here, among other things, protein biosynthesis and other metabolic activity take place. The inner and outer segments are separated by a narrow connecting cilium through which all substances for the outer segment must be actively transported.
Outer segment (AS)
The outer segment or outer member, English outer segment (OS) , is the light-sensitive compartment of the photoreceptors. Here the outer segments of the photoreceptors extend from the connecting cilium to the RPE. At the connecting cilium , new disc membranes , membrane constrictions, are created packed with rhodopsin . Rhodopsin is stored in the disks and initiates visual signal transduction . As a result of the new synthesis, these disks move to the RPE and are phagocytosed there .
Retinal pigment epithelium (RPE)
The retinal pigment epithelium ( Stratum pigmentosum ), English retinal pigment epithelium (RPE) , is initially a shading light filter. There is also an exchange of substances with photoreceptors.
With the pigment epithelium, a hexagonally assembled monolayer epithelium from the outer leaf of the embryonic optic cup is apparent, the retina is against the choroid ( choroidal ) discontinued. The cells of the RPE contain melanosomes colored black by melanin, which functionally represent light filters. Apically, finger-like, microvillary processes of the RPE encompass the photoreceptor cells, which serve to nourish the photoreceptors, to recycle the old disc membranes of the photoreceptor outer segments and to regenerate the bleached retinal from activated rhodopsin . Basally, these cells show deep furrows, which serve for a better exchange of substances with the blood vessels of the choroid. RPE cells prevent blood from entering the heavily vascularized choriocapillaris (the highly perfused boundary layer of the choroid). In the pars optica retinae , the connection between the RPE and the neuroretina is only maintained by suction actively generated by the RPE; a fixed connection only exists at the ora serrata .
Diseases of the retina
Examples of diseases of the retina are:
- Diabetic retinopathy , a disease of the retina that occurs as a result of diabetes
- hypertensive retinopathy , a disease of the retina caused by high blood pressure
- eclamptic retinopathy , retinal disease that occurs in pregnant women as part of eclampsia
- Retinopathia prematurorum , retinal disease occurring in premature infants
- Retinopathia pigmentosa , also called retinitis pigmentosa (RP) , congenital retinal disease
- Retinopathia centralis serosa , central retinal detachment caused by swelling
- Retinoblastoma , malignant tumors in infancy and early childhood
- Retinal dystrophy
- Retinal detachment
- Retinal foramen
- Retinal splitting
- Vascular occlusion, arterial with ischemia , and infarcts
- Macular degeneration
- Macular telangiectasia
- Azoor Acute Zonal Occult External Retinopathy
- peripheral retinal degeneration with thinning of the retina and clouds of glitter
Acetylsalicylic acid
A US American long-term study from Wisconsin suggests that regular intake of acetylsalicylic acid could possibly damage the retina and significantly increase the risk of age-related macular degeneration (AMD) . However, a causal connection with the development of the disease could not be proven.
Investigation procedure
A standard method for examining the retina is direct or indirect ophthalmoscopy or fundoscopy ( ophthalmoscopy ). It consists of illuminating the fundus and viewing the reflected image with a magnifying glass. This method has been established in ophthalmoscopic diagnostics since the invention of the ophthalmoscope in 1851 by Hermann von Helmholtz .
In the last few decades, further methods for retinal diagnostics have been developed:

- A relatively new, technically outstanding and more expensive method is optical coherence tomography (OCT), which extends the imaging of the examination area by the third dimension. It enables the production of high-resolution sectional images or even three-dimensional tomographies with a quality comparable to histological images (resolution of up to 3 µm compared to 0.3 µm for a light microscope). Here the individual retinal layers can be broken down and their thickness measured. This makes it possible to determine the finest differences, which can be decisive for the adequate therapy of certain retinal diseases or for testing drugs.
- Other imaging methods are offered by new types of scanning laser ophthalmoscopes , such as the Heidelberg Retina Tomograph (HRT), which can generate high-resolution three-dimensional slice or relief images by scanning the retina point by point or line by line and using confocal aperture and lighting technology.
Further examination and assessment options exist at the electrophysiological level
- the electroretinogram (ERG)
- the electrooculogram (EOG)
as well as to show the retinal blood flow through
- The fluorescein angiography (also FLA, FAG or Angio abbreviated)
- the ICG - angiography
- the Retinal vessel analysis with the Retinal Vessel Analyzer, which is used not only in diabetes mellitus, but also for the diagnosis of general changes in the microvessels ( "mirror image of the microvasculature").
See also
- Eye development (vertebrates)
- Eye evolution
- Retinal correspondence
- Choroid , uvea , Bruch's membrane
- Emmert's law
- visual signal transduction
- Retinal projector
- Retinometer
literature
- Robert F. Schmidt , Hans-Georg Schaible (ed.): Neuro- and sensory physiology . 5th edition. Springer Verlag, Berlin 2005, ISBN 978-3-540-25700-4 .
- Franz Grehn: Ophthalmology . 30th edition. Springer Verlag, Berlin 2008, ISBN 978-3-540-75264-6 .
- Albert J. Augustin: Ophthalmology . Springer Verlag, Berlin 2007, ISBN 978-3-540-30454-8 .
- RW Young: The ninth Frederick H. Verhoeff lecture. The life history of retinal cells. In: Transactions of the American Ophthalmological Society. Volume 81, 1983. pp. 193-228, ISSN 0065-9533 . PMID 6375087 . PMC 1312450 (free full text). (Review).
Web links
- Thumbnail overview of the retina of mammals
- Dendritic Processing in the Retina
- The photo laboratory in the retina . In: MaxPlanckResearch , 03/2001
- electron microscopic images of the human retina
- The Organization of the Retina and Visual System . Webvision, website of the John Moran Eye Center of the University of Utah on almost all aspects of mammalian retina
Individual evidence
- ↑ Wilfried Westheide, Gunde Rieger: Special Zoology. Part 2: vertebrates or skulls. Volume 1, Spektrum Akademischer Verlag, 2009, ISBN 978-3-8274-2039-8 , p. 100 ( limited preview in the Google book search)
- ↑ Johannes W. Rohen, Elke Lütjen-Drecoll: Functional Histology . Schattauer, FK Verlag 4th edition March 2000, p. 476, ISBN 978-3-7945-2044-2 .
- ^ Peter K. Ahnelt, Helga Kolb: The mammalian photoreceptor mosaic-adaptive design. In: Progress in Retinal and Eye Research. Volume 19, No. 6, 2000, pp. 711-777, doi: 10.1016 / S1350-9462 (00) 00012-4
- ↑ Imke Ortmann: Observed live: the direction detector in the eye. In: Spectrum of Science , November 2002, issue 11, p. 12ff.
- ↑ Joshua R. Sanes, Richard H. Masland: The Types of Retinal Ganglion Cells: Current Status and Implications for Neuronal Classification . In: Annual Review of Neuroscience . tape 38 , no. 1 , July 8, 2015, ISSN 0147-006X , p. 221–246 , doi : 10.1146 / annurev-neuro-071714-034120 ( annualreviews.org [accessed January 27, 2020]).
- ^ Richard H. Masland: The Neuronal Organization of the Retina, in Neuron 76, October 18, 2012
- ↑ Th. Axenfeld (original), H. Pau (ed.): Textbook and atlas of ophthalmology . With the collaboration of R. Sachsenweger u. a. Gustav Fischer Verlag, Stuttgart 1980, ISBN 3-437-00255-4 .
- ↑ Aspirin can apparently damage the retina. In: welt.de . January 23, 2013, accessed January 21, 2015 .
- ↑ rme / aerzteblatt.de: Acetylsalicylic acid could promote eye problems . In: aerzteblatt.de . December 19, 2012, accessed January 21, 2015 .
- ^ BE Klein, KP Howard et al. a .: Long-term use of aspirin and age-related macular degeneration. In: JAMA. Volume 308, number 23, December 2012, ISSN 1538-3598 , pp. 2469-2478, doi: 10.1001 / jama.2012.65406 , PMID 23288416 , PMC 3630794 (free full text).
- ↑ Ronald D. Gerste: Mirror image of the microvasculature. Deutsches Ärzteblatt 115 (48): A2234-A2238. November 30, 2018.