Retinopathia centralis serosa
| Classification according to ICD-10 | |
|---|---|
| H35.7 | Detachment of retinal layers |
| ICD-10 online (WHO version 2019) | |
As central serous chorioretinopathy (RCS) , and more recently preferred central serous chorioretinopathy (CRCS) is a disease of the retina (retina) of the eye referred to, there is liquid in from the blood vessels of the choroid accumulates (choroid) under the retina and thereby locally from Pigment epithelium stands out.
The accumulated fluid separates the light-sensitive sensory cells (visual cells) in the retina from the nourishing pigment epithelium and the choroid. Because here under the care of the retina with nutrients and oxygen, as well as the reduction of biochemical products of Sehzyklus suffering that can pin in the central fovea their function as (fovea) photoreceptors no longer fulfill completely. This shows up as a central gray-black spot ( central scotoma ) in the field of vision . In addition, the position of the retina can be changed by the local elevation in such a way that images - such as that of an Amsler grid - are perceived as distorted ( metamorphopsia ).
A fundamental distinction is made between the acute and the chronic form. While spontaneous healing is observed within 4 months in 68% and within 6 months in 84% of the patients, treatment with medication, various laser forms and injections into the eye ( intravitreal injection) is possible in the case of chronification .
Because of the significant involvement of the choroid ( choroid ), the term has central serous chorioretinopathy the old concept of central serous chorioretinopathy replaced. Due to the characteristic thickening of the choroid, the chorioretinopathia centralis serosa belongs to the spectrum of pachychoroidal diseases . Within this spectrum, central serous chorioretinopathy is classified as stage II of IV.
Epidemiology
The chorioretinopathia centralis serosa occurs with a frequency of 1 in 10,000. It is particularly common in young and middle-aged men (30–50 years of age). Men get sick six times more often than women. The occurrence of retinopathia centralis serosa is often related to mental or physical stress . RCS is the fourth most common non-surgical retinal disease. It is sometimes referred to as a manager's disease of the eye.
Symptoms
Typical symptoms of retinopathia centralis serosa are:
- Slight deterioration in vision
- Blurred vision
- "Gray-black spot" ( scotoma ) in the field of vision (reduced contrast sensitivity)
- Image distortion ( metamorphopsia )
- Farsightedness ( hyperopia )
- Color perception disorders
The symptoms vary depending on the extent and position of the retinal elevation. A leak in the area of the central retina ( macula ) results in severe distortions. With leaks that occur outside the macula, sometimes only small eccentrically located, iridescent colored spots or rings are perceived. These can be particularly noticeable when blinking and in semi-darkness, in front of tables on the screen and when looking at white surfaces. When working with tables, it is also easy to see the distortion from straight lines to waves and warps. At first you usually only have the feeling of a slight glare - but this is only one-sided and does not go away within minutes, as you are used to.
Risk factors
Since the chorioretinopathia centralis serosa is counted among the pachychoroidal diseases , factors that increase the choroid thickness and impair the functionality of the retinal pigment epithelium are considered to be the causes of the disease. The following risk factors were described:
- Young age (30-50)
- Male gender (6: 1)
- Farsightedness ( hyperopia )
- stress
- Type A personality
- Taking cortisone preparations
- Sleep apnea syndrome
- Helicobacter pylori infection
Diagnosis
The flat, central retinal detachment can be seen in the fundus . In addition, various imaging examinations are carried out in order to secure the diagnosis and to be able to assess the course. These include:
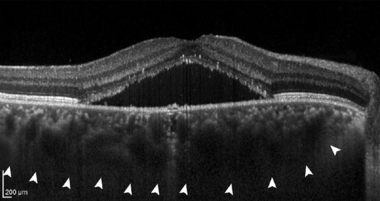
- Optical Coherence Tomography (OCT): The visualization of fluid under the retina is the typical sign of CRCS. Likewise, a thickening of the choroid (can choroid ) are observed. There is often a detachment of the retinal pigment epithelium . In chronic cases, damage to the retinal pigment epithelium and up to 25% of choroidal neovascularization (CNV) can be detected. The OCT is a standard examination for the initial diagnosis and for evaluating the course.
-
Fluorescence angiography : One of the two dyes fluorescein and indocyanine green , or often both together, are administered intravenously. The flooding in and out of both dyes is then observed in the eye by taking retinal images over a period of 5 to 30 minutes.
- Using the dye fluorescein , which is given intravenously, a leakage of fluid from the choroid through the Bruch's membrane and the retinal pigment epithelium into the retinal layers can be observed. More typically, in 10% of the cases, a “source point” of contrast medium is found at the point of the leak, from which the blister located below the retina fills. Much more often, however, the leak is discreet and only shows a slow build-up of dye. In chronic cases, the presence of choroidal neovascularization (CNV) is assessed using fluorescence angiography .
- An assessment of the choroid can take place using the dye indocyanine green . Typically, congested, thick choroidal vessels, local hypoperfusion, and later diffuse dye leakage from the vascular system, above which damage to the overlying layers (almost always retinal pigment epithelium , including retina) can be detected in optical coherence tomography .
- Optical coherence tomography (OCT) angiography: The vascular system of the retina and choroid can now be assessed using new vessel display modules in OCT even without intravenous administration of dye. OCT angiography is often carried out as an additional examination to the imaging modalities mentioned above in order to achieve better accuracy with regard to choroidal neovascularization (CNV) and, if necessary, to initiate intravitreal therapy using injections into the eye.
therapy
The therapy of chorioretinopathia centralis serosa is divided into acute and chronic forms due to the spontaneous healing tendency.
Acute
Spontaneous healing rates of 68% within four months and 84% within 6 months are reported from the initial diagnosis. Specialist societies therefore recommend starting therapy in most cases only after 4 months. Earlier initiation of therapy is, however, after consultation with an ophthalmologist due to personal circumstances, e.g. B. pronounced psychological strain or the desire for rapid healing possible. Another exception is the presence of choroidal neovascularization at the initial diagnosis; in this case a rapid anti-VEGF therapy can be useful.
In about 50% of the patients, a recurrence of the disease can be observed. In these cases, so-called relapses , rapid therapy can be useful.
Chronic
There is currently no standard therapy for chronic central serous retinopathy (overview: Cochrane Review). However, efficacy has been proven for many therapeutic approaches using drugs, lasers and intravitreal anti- VEGF injections ( ranibizumab , aflibercept , bevacizumab ).
- Mineralocorticoid receptor inhibitors: Since overactivation of the mineralocorticoid receptor in the choroid seems to be partially responsible for the CSCR, the mineralocorticoid receptor antagonist spironolactone is recommended for therapyin a large number of studies. The related drug eplerenone , which has fewer side effects, is also used by some ophthalmologists. However, according to a large-scale study from 2020, eplerenone is no more effective than placebo, which is why, according to data, patients should be treated with spironolactone if mineralocorticoid receptor inhibition is attempted. It should be noted that both spironolactone and eplerenone are "off-label"; H. be administered without authorization.
- Argon laser therapy: If the fluorescence angiography shows a clear source point that is outside the visual pit (macula), laser sclerotherapy is possible. This method, which has been used since the 1990s, shows an acceleration in the absorption of diseased fluid, but has no influence on visual acuity and the probability of future recurrences.
- "Subliminal laser" ( micropulse laser, selective retinal therapy , endpoint management): These laser methods attempt to selectively stimulate the retinal pigment epithelium without damaging the retina in order to trigger repair processes that lead to the resorption of the diseased fluid. The procedures appear to be comparable in terms of visual enhancement and complications. Furthermore, they can be repeated if the disease occurs again. However, according to a large-scale study from 2018, subliminal laser procedures seem to be inferior to photodynamic therapy .
- Half-dose / half-fluence photodynamic therapy (PDT): For PDT, a photosensitive drug (verteporfin) is administered intravenously tothe person affected. After 15 minutes, the affected area in the visual pit (macula) is irradiated using a non-thermal laser with a wavelength of 693 nm. This leads to the release of free radicals within the vascular system, which induce damage to the vascular wall. The following body's own repair processes thus seal leaking vessels. For chorioretinopathia centralis serosa, halving the dose of the drug to be administered (verteporfin) has proven useful (half-dose PDT) or, with the full drug dose, administering half the irradiation time (half-fluence PDT), as this significantly reduces the complication rates can. According to the results of a large-scale study from 2018, half-dose photodynamic therapy is considered by many ophthalmologists as the means of choice in chronic courses.
- Anti- VEGF therapy: In about 25% of the cases, a choroidal neovascularization (CNV) forms secondary in the long term. In these cases, the intravitreal administration of the anti-VEGF inhibitors ranibizumab , aflibercept and bevacizumab can be used to contain and seal the CNV, which can lead to improved vision. Ranibizumab is approved for this indication, while aflibercept and bevacizumab can be administered without approval ("off-label").
Web links
- RCS / CCS at Pro Retina Deutschland e. V. Pro Retina Germany is a self-help association for people with retinal degeneration.
- Information from the Kiel University Eye Clinic about the SRT laser: Selective retinal therapy (SRT). ( Memento from December 16, 2013 in the Internet Archive ) uni-kiel.de
- Visual impairment RCS: eyes under stress. In: Spiegel online. November 10, 2014.
Individual evidence
- ↑ a b c d e f g h i j Professional Association of German Ophthalmologists (Berufsverband der Augenärzte Deutschlands e.V., BVA), German Society of Ophthalmology (Deutsche Ophthalmologische Gesellschaft e.V., DOG), German Retina Society e. V. (Retinologische Gesellschaft e.V., RG): Statement of the Professional Association of German Ophthalmologists (BVA), the German Society of Ophthalmology (DOG) and the German Retina Society (RG) on central serous chorioretinopathy: Situation January 2018 . In: The ophthalmologist . tape 116 , S1, February 2019, ISSN 0941-293X , p. 10-20 , doi : 10.1007 / s00347-018-0809-7 ( springer.com [accessed March 17, 2020]).
- ^ A b Jakob Siedlecki, Benedikt Schworm, Siegfried G. Priglinger: The Pachychoroid Disease Spectrum — and the Need for a Uniform Classification System . In: Ophthalmology Retina . tape 3 , no. December 12 , 2019, p. 1013-1015 , doi : 10.1016 / j.oret.2019.08.002 ( elsevier.com [accessed March 17, 2020]).
- ^ Peter Wiedemann: RCS therapy with cold light laser. In: The ophthalmoscope. February 2, 2015.
- ↑ https://www.pharmazeutische-zeitung.de/2014-08/manag Krankheit-des-auges-sehstoerungen-durch-stress /
- ↑ https://www.deutsche-apotheker-zeitung.de/daz-az/2014/daz-44-2014/manag Krankheit-des- auges
- ↑ Chui Ming Gemmy Cheung, Won Ki Lee, Hideki Koizumi, Kunal Dansingani, Timothy YY Lai: Pachychoroid disease . In: Eye . tape 33 , no. 1 , January 2019, ISSN 0950-222X , p. 14–33 , doi : 10.1038 / s41433-018-0158-4 , PMID 29995841 , PMC 6328576 (free full text) - ( nature.com [accessed March 17, 2020]).
- ↑ M. Salehi, AS Wenick, HA Law, JR Evans, P. Gehlbach: Interventions for central serous chorioretinopathy: a network meta-analysis . In: Cochrane Database Syst Rev . tape 22 , no. 12 , 2015, p. CD011841 , doi : 10.1002 / 14651858.CD011841.pub2 .
- ↑ Elodie Bousquet, Talal Beydoun, Pierre-Raphaël Rothschild, Ciara Bergin, Min Zhao: SPIRONOLACTONE FOR NONRESOLVING CENTRAL SEROUS CHORIORETINOPATHY: A Randomized Controlled Crossover Study . In: Retina . tape 35 , no. December 12 , 2015, ISSN 0275-004X , p. 2505-2515 , doi : 10.1097 / IAE.0000000000000614 , PMID 26017871 , PMC 4697359 (free full text) - ( lww.com [accessed March 17, 2020]).
- ^ TR Herold, K. Prause, A. Wolf, WJ Mayer, MW Ulbig: Spironolactone in the treatment of central serous chorioretinopathy - a case series . In: Graefe's Archive for Clinical and Experimental Ophthalmology . tape 252 , no. December 12 , 2014, ISSN 0721-832X , p. 1985–1991 , doi : 10.1007 / s00417-014-2780-6 ( springer.com [accessed March 17, 2020]).
- ↑ Andrew Lotery, Sobha Sivaprasad, Abby O'Connell, Rosie A Harris, Lucy Culliford: Eplerenone for chronic central serous chorioretinopathy in patients with active, previously untreated disease for more than 4 months (VICI): a randomized, double-blind, placebo -controlled trial . In: The Lancet . tape 395 , no. 10220 , January 2020, p. 294–303 , doi : 10.1016 / S0140-6736 (19) 32981-2 ( elsevier.com [accessed March 17, 2020]).
- ↑ Edward H. Wood, Peter A. Karth, Steven R. Sanislo, Darius M. Moshfeghi, Daniel V. Palanker: NONDAMAGING RETINAL LASER THERAPY FOR TREATMENT OF CENTRAL SEROUS CHORIORETINOPATHY: What is the Evidence? In: Retina . tape 37 , no. 6 , June 2017, ISSN 0275-004X , p. 1021-1033 , doi : 10.1097 / IAE.0000000000001386 ( lww.com [accessed March 17, 2020]).
- ↑ a b Elon HC van Dijk, Sascha Fauser, Myrte B. Breukink, Rocio Blanco-Garavito, Joannes MM Groenewoud: Half-Dose Photodynamic Therapy versus High-Density Subthreshold Micropulse Laser Treatment in Patients with Chronic Central Serous Chorioretinopathy . In: Ophthalmology . tape 125 , no. 10 , October 2018, p. 1547–1555 , doi : 10.1016 / j.ophtha.2018.04.021 ( elsevier.com [accessed March 17, 2020]).
- ↑ Benedikt Schworm, Nikolaus Luft, Leonie F. Keidel, Felix Hagenau, Christoph Kern: Response of neovascular central serous chorioretinopathy to an extended upload of anti-VEGF agents . In: Graefe's Archive for Clinical and Experimental Ophthalmology . February 28, 2020, ISSN 0721-832X , doi : 10.1007 / s00417-020-04623-w ( springer.com [accessed March 17, 2020]).