Urethral stricture
| Classification according to ICD-10 | |
|---|---|
| N35 | Urethral stricture |
| N35.0 | Post-traumatic urethral stricture (birth, injury) |
| N35.1 | Post-infectious urethral stricture, not elsewhere classified |
| N35.8 | Other urethral stricture |
| N35.9 | Urethral stricture, unspecified |
| N99.1 | Urethral stricture after medical measures |
| ICD-10 online (WHO version 2019) | |
A urethral stricture is a scarred narrowing of the urethra . This can rarely be congenital, it is much more often the result of injuries or inflammation .
frequency
Urethral strictures predominantly affect men. Women are rarely affected by real strictures. Very rarely injuries to the woman's urethra with subsequent urethral narrowing occur during childbirth. Congenital strictures are also very rare.
causes
A basic distinction must be made between congenital and acquired urethral strictures.
Congenital urethral strictures
- Malformations of the external genitals (e.g. hypospadias )
Acquired urethral strictures
- Urinary catheters, so-called microtraumas (minimal injuries) play a role here during insertion, with latex catheters the release of toxic substances is still discussed as the cause
- direct injury such as the so-called straddle trauma (blunt trauma in the area of the perineum), pelvic fractures, open injuries (e.g. in traffic accidents), internal injuries during childbirth
- Urethral infections: urethritis , typically gonorrhea (gonorrhea)
- Related to balanitis xerotica obliterans (BXO)
- Tumors of the urethra or surrounding tissue
localization
- prostatic urethra: between the urinary bladder and the urethralis muscle (sphincter muscle)
- membranous urethra: below the prostate , inside the sphincter
- Bulbar urethra: between the sphincter muscle and the beginning of the mobile penis
- penile urethra: in the mobile part of the penis
- Navicular fossa : in the glans ( glans penis )
Symptoms
The main symptom is a weakened urine stream. The degree of weakening may increase over time. In extreme cases, urinary retention occurs . In addition, the urine stream can be twisted or split. Due to the increased resistance when urinating ( micturition ), incomplete emptying of the bladder with residual urine can occur. This residual urine build-up promotes the occurrence of infections of the urinary bladder ( cystitis ). Even without an infection, you may experience a burning sensation when urinating.
Another common symptom is evidence of blood in the urine, called microhematuria .
If the urethra has been narrow for a long time, the increased outlet resistance leads to a thickening of the bladder muscle ( bladder hypertrophy ) and thus to a decrease in elasticity and a further deterioration in the emptying function.
If the bladder is severely damaged, the urine may flow back into the ureters and kidneys ( reflux uropathy ). In extreme cases, this can damage the kidneys.
Diagnosis
At the beginning there is a precise questioning ( anamnesis ) of the patient. Particular attention should be paid to the duration of the complaints, injuries and infections. A urine test for infection diagnosis is also mandatory. The ultrasound gives information about the residual urine volume , the condition of the bladder , especially the thickness of the wall of the bladder and the kidneys . An X-ray examination with contrast agent is necessary to localize the stricture . In this so-called retrograde urethrography , contrast agent is injected into the stretched urethra and at the same time x-rayed . The location and length of the stricture can be determined here. If no clear statement can be made here, the urethra can be mirrored ( urethroscopy ).
treatment
The treatment is performed surgically. The following methods are essentially available for this purpose.
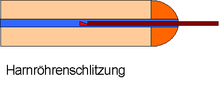
- Harnröhrenschlitzung ( urethrotomy ) : Here is a urethrotome entered into the urethra under direct vision (method according axis) or blind (method according to Otis) into the urethra and this slotted at 12 o'clock with a knife. A urinary catheter is then inserted. This remains for a few days, and after removal, a gel containing cortisone can be injected into the urethra to prevent it from occurring again ( relapse ).
- Oral mucosal plastic surgery: After one or two slits and recurrence of a urethral stricture or in the case of very long strictures, the urethra is widened by sewing in a piece of oral mucosa. To do this, the urethra is exposed from the outside and opened lengthways over the stricture. Now a piece of oral mucosa of the appropriate size is removed from either the lower lip or the cheek and sewn in. A urinary catheter is then placed here as well. In addition, an abdominal wall catheter is inserted into the bladder. The urinary catheter is used to splint and keep the urethra open. The abdominal wall catheter is used to empty the bladder. The urinary catheter is removed after about eight days. The abdominal wall catheter remains in place for about three weeks. After this time, an X-ray examination with contrast agent is carried out. The bladder is filled and the patient is then asked to urinate. If this is possible without any problems and if the bladder has been completely emptied, the abdominal wall catheter is removed.
- Urethral reconstruction with a tissue substitute made in the laboratory: In order to avoid the removal of larger segments of the oral mucosa during urethral plastic surgery, a tissue substitute can be made from the patient's own cells using tissue engineering in the laboratory. This tissue replacement, made from the patient's own cells, is used surgically to widen the urethra. Side effects that normally arise from the removal of larger segments of the oral mucosa during urethral surgery in the oral cavity are largely eliminated with this method.
- In the case of short strictures (up to 2 cm), the narrowed part can also be cut out. Both ends of the urethra are then sutured directly together.
- For tumors that occlude the urethra from the inside or outside, the treatment of the tumor is carried out depending on its type.
- An expansion ( bougienage ) to prevent recurrence is now only useful in exceptional cases.
See also
In contrast to scarred constriction, a non-scarred narrowing of the urethra can occur with an enlarged prostate .
Individual evidence
- ^ Hans U. Schmelz, Christoph Sparwasser, Wolfgang Weidner: Specialist knowledge of urology . 1st edition. Springer-Verlag, Heidelberg 2006, ISBN 978-3-540-20009-3 , p. 426.
- ↑ Clemens Gödel: Urethral constriction - causes in detail
- ↑ H. Knispel, B. Stuerzebecher et al. Clinical applications of autologous tissue-engineered oral mucosa graft for urethroplasty - An efficacy assessment. Urologist A Supplements 2014 (S1).