Interstitial cystitis
| Classification according to ICD-10 | |
|---|---|
| N30.1 | Interstitial cystitis (chronic) |
| ICD-10 online (WHO version 2019) | |
The Interstitial cystitis / cystitis - ger .: interstitial cystitis or bladder pain syndrome (BPS) and Painful Bladder Syndrome (PBS) - which is why short form IC / BPS - is an incurable disease of the bladder, a chronic inflammation of all layers of the bladder walls goes hand in hand. Interstitial cystitis is characterized by pollakiuria, urogenital pain, and a constant urge to urinate. Synonyms for the disease are: chronic interstitial cystitis; Hunner's cystitis according to Guy Hunner ; non bacterial cystitis; abacterial cystitis; painful bladder syndrome; Bladder pain syndrome.
A globally standardized definition of the disease does not yet exist. In the international nomenclature, the term bladder pain syndrome (BPS), translated "bladder pain syndrome", is preferred. This term is also used in the guidelines of the European Association of Urology (EAU) and by the "European Society for the Study of Interstitial Cystitis / Painful Bladder Syndrome" (ESSIC). In the S2K guideline "Diagnostics and Therapy of Interstitial Cystitis (IC / BPS)", initiated by the Interstitial Cystitis Association (ICA) Germany eV and published by the German Society for Urology eV (DGU), however, it says: "The sole designation bladder Pain Syndrome (BPS) or Painful Bladder Syndrome (PBS) restrict the symptoms of IC / BPS too much, as they only focus on pain. " In Germany, the term interstitial cystitis (IC) or (IC / BPS) is common. The term "interstitial cystitis" is the primary term used in ICD-10 and Medical Subject Headings .
The German Society for Urology defines IC as follows: "Interstitial cystitis (IC / BPS) is a non-infectious, chronic urinary bladder disease, which is characterized by pain, pollakiuria, nocturia and the urge to urinate in various forms and combinations of symptoms and with the simultaneous exclusion of differential diagnostic diseases. The diagnosis of IC / BPS is not tied to a specific bladder volume or persistent pain. "
The symptoms of IC / BPS often resemble those of acute or chronically recurring cystitis and symptoms of other diseases. Because of this and because the disease is relatively rare and also unknown, there are often misdiagnoses. Interstitial cystitis is a diagnosis of exclusion. This is done on the basis of the symptoms, the findings of a cystoscopy and a micturition protocol. The correct diagnosis of IC is often made very late. Those affected have already had years of suffering and numerous visits to the doctor. The diagnosis of IC is based on the clinical appearance and a cystoscopy, during which characteristic bleeding and tearing of the mucous membrane (mucosa cracking) occur after hydrodistension (expansion of the bladder with saline solution).
The quality of life of those affected is significantly impaired. In particular, the massive pain and the often constant need to urinate have a strong impact on the patient. Since the urge to urinate also occurs at night, a restful sleep is not possible. Many patients suffer from severe exhaustion as a result of the stress. 79 percent are repeatedly or permanently unable to work.
Common comorbidities and symptoms include muscle and joint pain, migraines, depressive moods, allergies, and stomach and intestinal diseases.
Spread / epidemiology
IC / BPS affects men and women of all cultures, socio-economic backgrounds and age groups. The available figures on the frequency and prevalence of interstitial cystitis are very different, which is probably due to the low level of awareness of the disease as well as frequent misdiagnoses and different recording methods. It is estimated that around 0.5% of people are affected in the United States and Europe. Women are 9 times more likely to be affected than men. The highest prevalence is found in middle-aged people; However, a third of the patients already have symptoms before the age of 30. The disease is very rarely diagnosed in Germany. However, there may be a high number of unreported cases.
Causes and course of the disease
The actual causes of IC are largely unknown. The possibility of an autoimmune disorder is being discussed among medical professionals. What is certain is that an initially present immune and barrier defect is present in the urothelium , the tissue of the urinary tract. The inner protective layer of the urothelium, the so-called glycosaminoglycan layer, or GAG layer for short, is pathologically changed in interstitial cystitis and is therefore permeable; The bladder wall and deeper tissue layers of the bladder are exposed to harmful urine components without protection. This triggers a chronic inflammatory process of the organ. In addition, the irritated bladder wall nerves cause constant, reflex-like cramping of the bladder wall muscles. Both lead to severe, stabbing pain, muscle cramps and a constant, painful urge to urinate. Those affected can often only produce small amounts of urine with severe pain, as controlled loosening of the muscles is hardly possible. In addition, during micturition, the urine passes through the urethra, the protective layer of which is also damaged - intense stabbing and burning pain are the result. The bladder capacity of the sick person decreases, especially in the advanced stage of the disease up to the final stage of the shrink bladder.
The S2K guideline "Diagnostics and Therapy of Interstitial Cystitis (IC / BPS)" names as further discussed etiopathogenetic factors: inflammation, neural overactivity (hyperactivity), impaired microcirculation, exogenous substances (almost 90% of those affected by IC / BPS name food intolerances ) , histamine intolerance (intolerance of ingested with food histamine ), infection, dysfunction of the pelvic floor, visceral crosstalk between the intestine and urinary bladder ( irritable bowel syndrome ), endometriosis (disease of the uterine lining), nichtharnblasenassozierte factors (comorbidities), psychosomatic stress disorders, microbiome (settlements with microorganisms) .
Genetic factors
It cannot be ruled out that genetic factors also play a role. Various studies have been conducted, including familial clustering studies and twin studies. Unequivocal evidence for genetic factors could not be found.
Investigation methods
The diagnosis is based on several pillars: anamnesis, micturition and pain diary, urine examination, urological and gynecological examination, biopsy of the bladder wall, molecular diagnosis of specific cell proteins.
Differential diagnosis
Symptoms of IC / BPD are similar to other urological and gynecological conditions, including urinary tract infections (UTIs), overactive bladder, sexually transmitted infections, endometriosis, bladder cancer, chronic pelvic pain syndrome, and chronic prostatitis. This is one reason why it often takes a long time for interstitial cystitis to be properly diagnosed. Other diseases with similar or identical symptoms can be ruled out using differential diagnoses.
American Urology Association (AUA) guideline
AUA guidelines recommend starting with a careful medical history, physical exam, and laboratory tests to assess and document symptoms of IC / BPD as well as other possible disorders.
IC guideline of the European Society for the Study of Interstitial Cystitis (ESSIC)
In 2008 the ESSIC society proposed stricter and more sophisticated diagnostic methods with specific classification criteria. The condition is that a patient must have bladder pain, accompanied by another urinary symptom. A patient with the sole symptom of frequent or urgent urination would be excluded from this diagnosis. In addition, diseases with similar symptoms are expressly ruled out by means of an extensive series of tests: This includes (A) an anamnesis and physical examination, (B) a urinalysis with test strips, various urine cultures and a serum PSA in men over 40 years of age, ( C) Measurement of flow and post-fluid residual urine volume by ultrasound and (D) cystoscopy. The diagnosis of IC is often confirmed or excluded by cystoscopy under anesthesia, during which hydrodistension (stretching of the bladder with saline solution) is performed. If IC is present, characteristic bleeding and tearing of the mucous membrane (mucosal cracking) will occur during this procedure.
Guideline German Society for Urology
This guideline also recommends a detailed anamnesis at the beginning. Differential diagnoses follow in order to exclude diseases with similar or identical symptoms. These include diseases of the musculoskeletal system and connective tissue, gastrointestinal diseases, gynecological findings, neurogenic causes, mental disorders, urological causes. Biomarkers for diagnostics are still being researched, currently no recognized biomarkers for diagnosing IC / BPS are available. The recommended physical exam also includes pain mapping in the genital region and a rectal exam. A urine test should also be performed. Other additional examinations that should be performed are urosonography, uroflowmetry (in men), cystoscopy. Further possible examinations are hydrodistension (stretching of the urinary bladder with sterile saline solution to determine the anatomical capacity of the bladder) and flow EMG (urine flow measurement with pelvic floor drainage). A potassium chloride (KCI) test can be considered. The KCl test, also known as the potassium sensitivity test, uses a mild potassium solution to assess the integrity of the bladder wall. A biopsy of the urinary bladder wall and stool diagnostics can also be considered.
Questionnaires and documentation forms such as "O'Leary-Sant interstitial cystitis symptom and problem indices (ICPI / ICSI)", "Pelvic Pain and Urgency / Frequency (PUF) patient symptom scale" or "Bladder Pain / IC Symptom Score (BPIC-SS ) are used to record and evaluate the IC / BPS symptoms such as pain and urinary symptoms.
pathology
In the early stages of IC / BPS, there is often no evidence of tissue changes. The IC / BPS is later to be demonstrated pathologically. A special procedure is used for tissue examination (Giemsa staining S-100 immunohistochemistry).
treatment
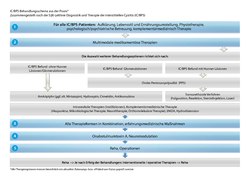
The current overview of the therapy options for the treatment of interstitial cystitis is provided by the German S2K guideline "Diagnostics and Therapy of Interstitial Cystitis (IC / BPS)" of the German Society for Urology (DGU). This classifies the treatment options under the headings "Conservative measures", "Oral drug therapy" (drugs to repair the GAG layer, drugs against pain and urination, antidepressants, pain therapy, etc.), complementary medicine (acupuncture, microbiological therapy, etc.), " Intravesical therapy ”(therapies that are introduced directly into the urinary bladder through a catheter), transurethral procedures (injections and instillations into the urinary bladder), hydrodistension and interventional / surgical therapy. Another option is inpatient rehabilitation. The choice of therapy options depends on the patient's medical history and diagnosis. The therapy concepts should be comprehensive, interdisciplinary and multimodal.
Pain therapy
Adequate pain management is a fundamental factor in IC treatment. Depending on the severity of the pain symptoms and the individual response of the patient, the oral administration of selective and non-selective non-steroidal anti-inflammatory drugs (NSAIDs), anticonvulsants, novaminsulfon and opioids is recommended. There is currently no uniform treatment concept for pain therapy in IC / BPS.
Oral drug therapy
Pentosan polysulfate / PPS (trade name elmiron) has been the only drug approved for the treatment of IC in Europe since October 2017 and is therefore reimbursed by health insurers. Pentosan polysulfate can relieve symptoms of IC by rebuilding the patient's damaged bladder wall and promoting blood flow to the urinary bladder. The earlier treatment with pentosan polysulphate begins, the better the results. In addition, analgesics, antihistamines, immunosuppressants, pain-relieving antidepressants and anesthetics can be used in oral therapy. Dimethyl sulfoxide can be used for additional anti-inflammatory properties. Accompanying pain therapy is recommended.
Intravesical therapy
In intravesical therapies, active ingredients are instilled into the bladder using a catheter. Intravesical therapy has the advantage of delivering high concentrations directly into the bladder. Pentosan polysulphate, which was also used for intraversical therapy for a long time, is currently no longer available on the European market. A distinction must be made between bladder instillations, which are approved as medical products (hyaluronic acid, chondroitin sulfate) and instillation cocktails, which consist of various drugs. Bladder instillations that have been approved as medical devices are only reimbursed by health insurers in individual cases and are mainly used to support the reconstruction of the GAG layer. Regular instillations on a weekly basis, later every one to two months, are required. Different drugs are used in instillation cocktails. The instillation of local pain medication (lidocaine) may also be useful. A possible addition to intravesical therapy is the Electromotive Drug Administration (EMDA). With the EMDA method, the medication can be introduced electrochemically into deeper layers of the urinary bladder wall by applying a voltage field to the transurethrally placed special catheter. .
Operational procedures
A hydrodistension performed under general anesthesia, which is also successfully performed to diagnose IC, has a therapeutic effect in about a third of patients that can last for about 2-3 months. Sacral neuromodulation has also proven to be effective, in which a neurostimulator ("bladder pacemaker") is implanted that delivers electrical impulses to the sacral spinal nerves in order to alleviate the symptoms of IC. Transurethral resection, in which diseased tissue is removed from the urinary bladder, can also be a treatment option. The last resort is the removal of a large part or the entire urinary bladder ( cystectomy ) with an artificial urine outlet.
Accompanying therapies
There are various therapy options that can be used alongside the treatment methods mentioned so far. Since IC patients are constantly confronted with massive restrictions on their quality of life, support in the form of psychotherapy can be helpful in learning how to deal with the disease and its effects on social life and relationships in a healthy way. Many patients also develop mental illnesses during the course of the disease, e.g. B. Depression and chronic fatigue, in which case psychotherapeutic treatment is essential. Since the chronic pain associated with IC often leads to poor posture and massive muscle tension, accompanying physiotherapy has also proven to be useful. A special form of physiotherapy is the treatment of the pelvic floor, which is often chronically tense in IC patients. Appropriate therapy to relax the internal muscles can alleviate the symptoms of IC. Other possible physiotherapeutic treatment approaches are relaxation and myofascial techniques as well as vibration therapy.
Complementary medicine
Various complementary medical approaches have been reported to support the treatment of IC. These include, for example, acupuncture , neural therapy , osteopathy and heat treatments.
Inpatient rehabilitation measures
Another therapy option that accompanies the other methods is inpatient rehabilitation. This is carried out in specialized urological rehabilitation clinics. In the clinical setting, the patient is offered multimodal therapy that requires active cooperation from those affected. Sometimes this is a way to prevent impending incapacity for work and / or to escape social isolation.
Self help
Last but not least, there are some self-help measures that patients can take to both improve their general quality of life and to reduce the severity of disease flare-ups. An important aspect is of course an increased, controlled fluid intake. A change in diet is also advisable. In many cases, patients often report a significant improvement in IC symptoms after changing their eating habits. Other lifestyle changes such as adapting clothing and physical activity, as well as a generally healthy lifestyle, can also have a positive effect on the course of the disease. Hypothermia, heavy physical exertion, excessive stress and general excessive demands should be avoided if possible. Many patients find the exchange with other affected persons helpful.
Prospect of healing
Interstitial cystitis is a chronic disease. According to the current state of knowledge, a cure is not possible. However, the further development of the disease can be prevented or at least delayed by alleviating the symptoms through multidisciplinary treatment approaches (see treatment). The earlier the interstitial cystitis is recognized and treated, the better the therapeutic success.
history
Earliest records of interstitial cystitis were published in 1836 by the Philadelphia surgeon Joseph Parrish. He described three cases of severe lower urinary tract symptoms without a bladder stone. The term "interstitial cystitis" was first used in 1887 by Alexander Skene , a New York doctor, in the publication Disease of bladder and urethra in woman . In 1915 there was a publication by the gynecological surgeon and pathologist Guy Hunner (1868–1957), after whom the Hunner lesions, special inflammatory changes in the urinary bladder, are named to this day.
The first guideline for diagnosing and treating interstitial cystitis was published in 2009 by a Japanese research team. The American Urological Association published the first American clinical practice guideline for the diagnosis and treatment of IC / BPD in 2011. In 2018, the German Society for Urology published the S2K guideline "Diagnostics and Therapy of Interstitial Cystitis (IC / BPS)".
On August 19, 1993 the "ICA-Germany e.V." - non-profit association and support association for interstitial cystitis - founded as the first IC / BPS organization in Europe (the second worldwide after the ICA in the USA). The association takes care of the education and information of doctors and the public, it initiated numerous research projects and contributed to the fact that diagnosis and therapy options were significantly improved.
In the United States, interstitial cystitis is officially recognized as a disability. In Germany, IC / BPS can also be recognized as a disability. However, the degree of disability is often disputed.
literature
- Laura M. Bogart, Sandra H. Berry, J. Quentin Clemens: Symptoms of Interstitial Cystitis, Painful Bladder Syndrome and Similar Diseases in Women. A systematic review. In: The Journal of Urology . Volume 177, 2007, pp. 450-456, doi: 10.1016 / j.juro.2006.09.032 ; PDF reprint by Rand Corporation .
- Karl H. Kurth: Interstitial Cystitis. Results Verlag, Hamburg 2004, ISBN 3-87916-069-4 .
- Ina Maria Teichgräber [1] , On the effectiveness of oral pentosan polysulphate therapy (SP54) in the treatment of chronic interstitial cystitis, dissertation at the Medical Faculty of the Friedrich-Alexander University Erlangen-Nuremberg, September 30, 2014.
Web links
- Guideline for the diagnosis and treatment of interstitial cystitis
- www.urologielehrbuch.de, chapter interstitial cystitis
- Website ICA Germany eV
- Ärzteblatt, Interstitial Cystitis
Individual evidence
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 6 , accessed on August 6, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 6 , accessed on August 6, 2019 .
- ↑ Bschleipfer, Thomas et al .: INTERSTITIAL CYSTITIS IC / BPS. Patient information. In: https://www.urologenportal.de/ . German Society for Urology, September 15, 2018, p. 4 , accessed on August 6, 2019 .
- ↑ Michels, Sven: Interstitial cystitis - own experiences in the treatment with Electromotive-Drug Administration (EMDA) at the Klinikum rechts der Isar, Munich. June 20, 2013, p. 1 , accessed August 6, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 6 , accessed on August 6, 2019 .
- ^ ICA Germany eV: Diagnosis of Interstitial Cystitis. In: Federal Association for Health Information and Consumer Protection. Retrieved August 6, 2019 .
- ^ German Society for Urology: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). In: https://www.urologenportal.de/ . September 30, 2018, accessed March 1, 2019 .
- ↑ Dr. med. Dirk Manski: Interstitial Cystitis (2/3): Pathology, Clinic and Diagnoses. In: https://www.urologielehrbuch.de/index.html . 2019, accessed March 1, 2019 .
- ↑ D. Engeler (Chair), AP Baranowski, J. Borovicka, AM Cottrell, P. Dinis-Oliveira, S. Elneil, J. Hughes, EJ Messelink (Vice-chair), AC de C Williams - Guidelines Associates: S. Goonewardene, MP Schneider: EAU Guidelines on Chronic Pelvic Pain. In: https://uroweb.org/guidelines/ . March 2017, accessed March 1, 2019 .
- ↑ ICA Germany eV: Interstitial Cystitis - EDITION 2017 - Information from ICA Germany eV Accessed on March 1, 2019 .
- ↑ Harro Albrecht: Cystitis - Sixty times to the toilet. In: https://www.zeit.de . October 17, 2018, accessed March 1, 2019 .
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ^ German Society for Urology: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). In: https://www.urologenportal.de/ . September 30, 2018, accessed March 1, 2019 .
- ↑ Dr. med. Dirk Manski: Interstitial Cystitis (2/3): Pathology, Clinic and Diagnoses. In: https://www.urologielehrbuch.de/index.html . 2019, accessed March 1, 2019 .
- ↑ D. Engeler (Chair), AP Baranowski, J. Borovicka, AM Cottrell, P. Dinis-Oliveira, S. Elneil, J. Hughes, EJ Messelink (Vice-chair), AC de C Williams - Guidelines Associates: S. Goonewardene, MP Schneider: EAU Guidelines on Chronic Pelvic Pain. In: https://uroweb.org/guidelines/ . March 2017, accessed March 1, 2019 .
- ↑ ICA Germany eV: Interstitial Cystitis - EDITION 2017 - Information from ICA Germany eV Accessed on March 1, 2019 .
- ↑ Harro Albrecht: Cystitis - Sixty times to the toilet. In: https://www.zeit.de . October 17, 2018, accessed March 1, 2019 .
- ↑ Harro Albrecht: Cystitis - Sixty times to the toilet. In: https://www.zeit.de . October 17, 2018, accessed March 1, 2019 .
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ gie / EB / aerzteblatt.de: First guideline for diagnosis and therapy of interstitial cystitis in progress. In: https://www.aerzteblatt.de/ . April 5, 2018, accessed March 1, 2019 .
- ^ German Society for Urology: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). In: https://www.urologenportal.de/ . September 30, 2018, accessed March 1, 2019 .
- ↑ SD Jocham, G. Froehlich, F. Sandig, A. Ziegler: The supply situation for patients with interstitial cystitis in Germany: results of a survey among 270 people affected. In: https://www.ica-ev.de/daten= März 2017. Retrieved on March 1, 2019 .
- ↑ Hertle, Lothar; Oberpenning, Frank; Ophoven, Arndt van: Chronic interstitial cystitis. In: https://www.aerzteblatt.de/ . 2002, accessed March 11, 2019 .
- ↑ SD Jocham, G. Froehlich, F. Sandig, A. Ziegler: The supply situation for patients with interstitial cystitis in Germany: results of a survey among 270 people affected. In: https://www.ica-ev.de/daten= März 2017. Retrieved on March 1, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 8 , accessed on August 7, 2019 .
- ↑ https://www.aerzteblatt.de/archiv/129764/Interstitielle-Zystitis-bleibt-oft-unerkannt
- ↑ https://www.medical-tribune.de/medizin-und-forschung/artikel/interstitielle-zystitis-trifft-vor-allem-frauen-mittleren-alters
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, pp. 8-13 , accessed on August 7, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 13 , accessed on August 7, 2019 .
- ↑ ICA Deutschland eV: How is the interstitial cystitis diagnosed? In: https://www.ica-ev.de/ . Retrieved March 1, 2019 .
- ↑ Dtsch Arztebl International: Interstitial cystitis often goes undetected. In: https://www.aerzteblatt.de/ . September 14, 2012, accessed March 1, 2019 .
- ↑ American Urological Association - ( en ) Accessed November 7 2018th
- ↑ Hanno, Philip M. et al .: Diagnosis and Treatment Interstitial Cystitis / Bladder Pain Syndrome. (pdf) American Urological Association (AUA) Guideline. In: https://www.auanet.org . American Urological Association, December 5, 2014, p. 45 , accessed August 8, 2019 .
- ↑ van de Merwe. JP et al .: Diagnostic Criteria, Classification, and Nomenclature for Painful Bladder Syndrome / Interstitial Cystitis: An ESSIC Proposal. (pdf) In: https://www.europeanurology.com . European Society for the Study of Interstitial Cystitis (ESSIC), September 20, 2014, accessed on August 8, 2019 .
- ↑ Viereck, V. et al .: Differentiation of the bladder pain syndrome from the overactive irritable bladder. (pdf) In: https://ch.universimed.com . Universimed Cross Media Content GmbH, December 7, 2017, accessed on August 8, 2019 .
- ↑ a b Tyagi P, Kashyap MP, Kawamorita N, Yoshizawa T, Chancellor M, Yoshimura N: Intravesical liposome and antisense treatment for detrusor overactivity and interstitial cystitis / painful bladder syndrome . In: ISRN Pharmacol . 2014, No. 601653, January 2014, p. 601653. doi : 10.1155 / 2014/601653 . PMID 24527221 . PMC 3914518 (free full text).
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, pp. 14-19 , accessed on August 7, 2019 .
- ↑ ICA Deutschland eV: How is the interstitial cystitis diagnosed? In: https://www.ica-ev.de/ . Retrieved March 1, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 15 , accessed on August 7, 2019 .
- ^ ICA Germany eV: Questions and answers. In: https://www.ica-ev.de/ . Retrieved March 1, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, accessed on August 21, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, pp. 23-25 , accessed on August 21, 2019 .
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, pp. 20-21 , accessed on August 21, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, pp. 21-25 , accessed on August 21, 2019 .
- ↑ Bschleipfer, Thomas et al .: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). (pdf) Long version, 1st edition, Version 1, 2018. In: https://www.urologenportal.de/ . German Society for Urology, September 30, 2018, p. 26 , accessed on August 21, 2019 .
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ Vetter, Christine: Interstitial cystitis: build up the layers of the urinary bladder wall. In: https://www.aerzteblatt.de/ . 2004, accessed March 1, 2019 .
- ↑ Meißner, Thomas: Urologists bring "light into the dark" in interstitial cystitis. In: https://www.aerzteblatt.de/ . October 15, 2004, accessed March 1, 2019 .
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ https://www.aerzteblatt.de/archiv/30183/Chronische-interstitielle-Zystitis
- ↑ https://www.gelbe-liste.de/leitlinien/leitlinie-interstitielle-zystitis
- ↑ German Society for Urology: DGU and ICA-Germany set milestone: First guideline for diagnosis and treatment of interstitial cystitis. In: https://www.urologenportal.de . March 26, 2018, accessed March 1, 2019 .
- ↑ C. Persu, V. Cauni, S. Gutue, I. Blaj, V. Jinga, P. Geavletel: From interstitial cystitis to chronic pelvic pain. In: Journal of Medicine and Life. May 25, 2010, accessed March 1, 2019 .
- ↑ DA Moutzouris, ME Falagas: Interstitial Cystitis: An Unsolved Enigma . In: Clinical Journal of the American Society of Nephrology . tape 4 , 2009, p. 1844-1857 , doi : 10.2215 / CJN.02000309 , PMID 19808225 .
- ↑ Klinikum Lüneburg - Center for Interstitial Cystitis and Pelvic Pain : Center for Interstitial Csystitis and Pelvic Pain. Retrieved March 1, 2019 .
- ↑ Yukio Homma, Tomohiro Ueda, Takaaki Ito, Mineo Takei, Hikaru Tomoe: Japanese guideline for diagnosis and treatment of interstitial cystitis . In: International Journal of Urology . 16, No. 1, 2009, pp. 4-16. doi : 10.1111 / j.1442-2042.2008.02208.x . PMID 19120522 .
- ^ German Society for Urology: S2K guideline: Diagnosis and therapy of interstitial cystitis (IC / BPS). In: https://www.urologenportal.de/ . September 30, 2018, accessed March 1, 2019 .
- ↑ Policy Interpretation Ruling Titles II and XVI: Evaluation of Interstitial Cystitis . Social Security Administration. Archived from the original on October 31, 2012. Retrieved March 8, 2019.
- ↑ ICA Germany eV: With expert knowledge, the degree of disability with 60 + G recognized. In: https://www.ica-ev.de/ . Retrieved March 1, 2019 .