Pancreas transplant
A pancreas transplant (PTx) is the operative transfer of the pancreas ( pancreas ) into an organism.
As a rule, the combined (simultaneous) transplantation of the pancreas and kidney (PNTx) of an organ donor takes place, the organ recipient being terminally (finally) kidney failure due to diabetes mellitus and being on a dialysis program. The successful PNTx leads to the complete normalization of the glucose metabolism and to freedom from dialysis. According to the International Pancreas Transplant Registry (IPTR), the chances of success (1-year function rate) for PNTx are 86% (pancreas) and 93% (kidney). Due to the higher complication rate compared to kidney transplantation alone, the recipients are selected more strictly, especially with regard to the cardiovascular risk. According to the IPTR, more than 35,000 pancreatic transplants had been performed worldwide by the end of 2010, 75% of them in the USA. In Germany, the number of pancreatic transplants since 2001 has been between 212 (2001) and 169 (2012) per year (DSO annual reports).
Transplant by Category
- Combined pancreas-kidney transplantation: Terminal, possibly pre-terminal type 1 diabetes with kidney failure, in rare cases also type 2 diabetes. Both organs come from the same organ donor and are immunologically identical. The function of the kidney transplant serves as an important parameter in the diagnosis of a rejection reaction, which is confirmed by a kidney transplant biopsy.
- Pancreas transplantation after previous kidney transplantation (PAK = pancreas-after-kidney transplant): The organ recipient has already had a kidney transplantation. The pancreas transplant is therefore carried out independently of this, the two transplanted organs therefore have different tissue characteristics ( HLA characteristics ). In principle, rejection reactions can take place in isolation in each of the transplanted organs; diagnosis in the area of the pancreatic transplant is difficult due to the lack of sensitive laboratory parameters.
- Isolated pancreas transplantation (IPT ): pancreas transplant alone in patients with repeated severe hypoglycaemia and stable kidney function. Diagnosis of rejection difficult due to lack of sensitive laboratory parameters.
- Pancreas transplantation as part of a multivisceral transplantation, e.g. B. combined with liver or small intestine
Organ allocation
Organ placement is comparable to kidney transplantation according to the criteria of Eurotransplant . Criteria include the waiting time and the correspondence of the tissue characteristics ( HLA characteristics ) of the donor and recipient. In addition, factors such as the country of origin of the donor and recipient and the distance between the location of the organ removal and the transplant center are included in the calculation.
Living donation
Living donation for pancreatic transplantation is possible in principle, but involves considerable risks for the pancreatic donor and significantly poorer results for the recipient.
Surgical technique
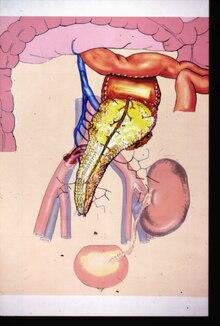
Like hardly any other organ transplant, pancreatic transplantation has been shaped for a long time by modifications of the surgical technique (see historical development). The transplantation of the entire organ including an approximately five to ten centimeter long segment of the duodenum ( duodenum ) (pancreatic duodenal transplantation) has established itself as the standard technique. The duodenal segment is used to drain the pancreatic secretion via an enteric anastomosis to the upper small intestine ( jejunum ) using the small intestine drainage technique or alternatively to the urinary bladder (bladder drainage technique). The bladder drainage technique (currently approx. 15%) was increasingly abandoned. The transplant is usually intraperitoneally in a heterotopic position, i.e. not at the location of the recipient's pancreas, which remains there. The graft is usually located in the right lower abdomen. The arteries are anastomosed to the common iliac artery (main pelvic artery ) and the transplant vein ( portal vein ) to the inferior vena cava (lower vena cava) and the superior mesenteric vein ( intestinal vein ). The venous anastomosis to the intestinal vein is also known as the portal venous drainage technique. In this way, quasi-physiological conditions of the insulin effect can be achieved.
Complications
Surgical complications after pancreatic transplantation are overall significantly more common than e. B. after an isolated kidney transplant. Transplant losses are mostly due to thrombosis of the transplant vein or inflammation of the transplanted pancreas ( transplant pancreatitis ). Transplant pancreatitis is largely to be understood as a consequence of the necessary organ preservation (reperfusion damage).
Immunosuppression and rejection reaction
Immunosuppressive therapy is basically comparable to other forms of organ transplantation from a combination of a calcineurin - inhibitor (. Eg cyclosporin or tacrolimus ), a proliferation inhibitor ( mycophenolate mofetil or azathioprine ) and a glucocorticoid (e.g., prednisolone ). As a rule, antithymocyte globulin (induction therapy) is also used initially . Acute rejection reactions are treated with steroids and antibodies.
historical development
The first pancreas transplant was performed as PNTx in 1966 by WD Kelly and RC Lillehei in Minneapolis (USA). In Europe, Felix Largiadèr carried out the first successful pancreatic transplant in 1973 in Zurich (Switzerland). In Germany, pancreatic transplantation is mainly associated with Walter Land (pancreatic segment transplantation with duct occlusion), Ulrich Hopt (pancreatic duodenal transplantation with bladder drainage) and Martin Büsing (small intestine and portal venous drainage).
swell
- AC Gruessner (2011): 2011 Update on Pancreas Transplantation: Comprehensive Trend Analysis of 25,000 Cases Followed Up Over the Course of Twenty-Four Years at the International Pancreas Transplant Registry (IPTR) . Reveau Diabetes Studies 8 (1): pp. 6-16
- WD Kelly, RC Lillehei, FK Merkel, Y. Idezuki, FC Goetz (1967): Allotransplantation of the pancreas and duodenum along with the kidney in diabetic nephropathy. Surgery 61 (6): 827-837
- TS Schulz, M. Kapischke, M. Buesing (2005): Neoquadruple induction with antithymocyte globulin / azathioprine / cyclosporine / prednisolone in simultaneous pancreas and kidney transplant recipients: 8.5-year results. Transplantation Proceedings 37 (4): pp. 1815-1817
- UT Hopt, M. Buesing, WD Schareck, HD Becker (1992): The management of exocrine pancreatic secretion - a central problem of allogeneic pancreas transplantation. The surgeon 63 (3); 186-192
- M. Buesing, D. Martin, T. Schulz, M. Heimes, J. Klempnauer, W. Kozuschek (1998): Pancreas transplantation with bladder and intestinal drainage technique with systemic-venous and initial experiences with portal venous drainage. Which technique can be recommended today? The surgeon 69 (3): pp. 291-297
- UT Hopt: Specific noxae in the pathogenesis of transplant pancreatitis in acute pancreatitis - transplant pancreatitis, editors: UT Hopt, M. Büsing, HD Becker, Verlag Karger, Basel 1994, ISBN 3-8055-5811-2
- Pancreatic transplantation "Chirurgische Gastroenterologie", Vol. 12, Suppl. 1 (1996) Editor: M. Büsing, UT Hopt, W. Kozuschek, Verlag Karger, Basel http://idw-online.de/de/news712
Web links
- Organ donation and transplantation in Germany 2012 - annual report. (PDF) DSO , April 2013, p. 33 ff. , Accessed on July 29, 2013 .
Individual evidence
- ↑ Felix Largiadèr. In: University Hospital Zurich. Clinic for Visceral and Transplant Surgery, accessed January 2, 2020 .