Root canal revision
In dentistry, a root canal revision (also called endorevision ) is the repetition of a root canal treatment on a tooth . This secondary treatment may be necessary if the desired healing success has not occurred after the first root canal treatment.
The aim of the revision is the healing of the periapical region, the bone surrounding the tooth root and the periodontal ligament, as well as the elimination and prevention of complaints such as pain or swelling
By removing the old root filling, cleaning the root canal system again, filling the root and creating a new restoration ( tooth crown ), a permanent seal of the endodontic system should be created.
Reasons for the failure of root canal treatments
In addition to root fractures, the main cause of failure of root canal treatments is contamination of the root canal lumen with bacteria . These either remained in the root canal system, later penetrated the root canal system through leaky restorations or caries, or were transported iatrogenically into the periapical tissue during the treatment. A distinction is made between intraradicular (inside the root) and extraradicular (outside the root) localized infections. In addition, there are non-infectious causes of root canal treatment failure. In a scientific statement from the German Society for Dentistry, Oral and Maxillofacial Medicine (DGZMK) from 2004, the causes of endodontic failure / post-endodontic diseases are defined as follows:
- Persistence of microorganisms after initial treatment
- Untreated root canals or root canal sections
- Leaky coronal restoration (leaky crowns or fillings) or coronal “microleakage” with new entry of microorganisms
- Foreign body reaction
- Extra radicular infections
Intraradicular infections
In the context of bacterial contamination, bacteria of the Enterococcus faecalis species are found significantly frequently in root-filled teeth with inflammation at the root tip. Fungal infections, especially fungi of the species Candida albicans, can also be detected in the canal if the root fillings have failed. The colonization with Candida albicans or Enterococcus faecalis in the root canal is favored by working without a rubber dam , a leaky temporary or permanent coronal closure of the access cavity, unnecessarily long total treatment time over several sessions or the use of ineffective antiseptic agents.
Extra radicular infections
Intraradicular infection can spread to surrounding tissues, bone and periodontium through the natural opening at the tip of the root , and eventually to the outer surface of the root. This extraradicular infection can also be caused by accidentally spreading germs during root canal treatment. On the root surface, the bacteria settle in a biofilm that cannot be adequately eliminated by the body's own immune system (13). It is also possible that bacteria remain in nests of epithelial cells , for example in residual tissue from cysts, and thus prevent the periapical region from healing (17). In contrast to intraradicular infections, extra-radicular infections cannot be successfully treated by revision treatment alone.
Non-infectious causes
In rare cases, non-infectious causes such as foreign body reactions are the cause of the failure of a root canal treatment. For example, cholesterol crystals that arise from long-term chronic inflammation can cause foreign body reactions in the periapical tissue. Traces of the talc in the root filling material ( gutta-percha ) or cellulose particles from paper points used to dry the root canals can also cause non-infectious inflammation. In the case of failures with extraradicular or non-infectious causes, only a surgical intervention (root tip resection) can enable a cure.
Indications for the need for a root canal revision
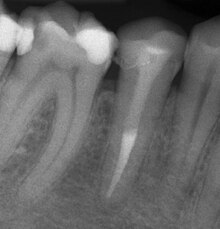
To assess the success of a root canal treatment, clinical complaints such as pain, swelling or fistulas as well as the radiological findings are used. Often there are no clinical symptoms despite endodontic infection, which is why the radiological control is the main criterion for the assessment. In addition to the existing root filling and changes in the root physiognomy (resorptions), the condition of the periapical tissue in particular is examined and checked for the presence of apical periodontitis or a radical cyst.
Indications for revision according to professional associations
The European Society of Endodontology (ESE) gives the following reasons for the need for a root canal revision in its quality guidelines for endodontic treatment (20):
- For teeth with inadequate root filling with radiological findings of developing or remaining apical periodontitis (inflammation of the tissue surrounding the tooth root) and / or symptoms (pain, discomfort).
- For teeth with inadequate root fillings that require replacement of the coronal restoration (e.g. crown) or coronal bleaching .
The indications for revision of a root canal treatment of the DGZMK are:
- Root canal-treated teeth with radiological symptoms of persistent or newly developed, endodontically caused apical periodontitis.
- Root canal treated teeth with clinical symptoms of endodontically caused apical periodontitis.
- Root canal treated teeth with radiologically or clinically insufficient root canal filling (e.g. insufficient homogeneity of the filling, untreated root canals, unfilled areas of the endodontic system, questionable and no longer indicated filling material etc.) without clinical or radiological signs of apical periodontitis.
- Root canal fillings with exposure to the oral cavity environment.
- Root canal treated teeth with progressive, external inflammatory resorptions.
Contraindications
If an improvement of the initial condition and a removal of the possible causes cannot be expected or the preservation of the tooth is questionable, a revision should not be carried out. Likewise, non-endodontic causes of the disease must be ruled out before an intervention. According to Strindberg et al. the endodontic failure after a sufficient healing time of four years is defined as the presence of residual, persistent or progressive radiographic lightening (dark point at the root tip in the X-ray image) and / or the presence of clinical complaints of any kind.
Clinical course of treatment
In order to be able to guarantee the treatment in a bacteria-free environment, a rubber dam should first be applied to keep the bacteria in the saliva away from the surgical field.
In a second step, any existing caries and leaky fillings are removed and the missing parts of the tooth are supplemented with a bacteria-proof filling. If necessary, existing restorations such as crowns must be completely removed. If it turns out that the tooth is no longer worth preserving because there is no longer any prospect of preservation, a revision is not carried out.
A sufficiently large access cavity is then created and possibly. Existing root posts and the old root filling material are completely removed from the canals with special files. Whole canals or canal sections that were not treated during the first root canal treatment are prepared along with the cleared canals over their entire length up to the natural exit at the root tip. The goal is to achieve complete continuity of the channels. Any broken instrument fragments remaining in the canal system from the initial treatment are removed if necessary.
The canals are completely prepared chemo-mechanically, with the disinfection of the endodontic system preferably being done with sodium hypochlorite , ethylenediaminetetraacetic acid (EDTA) and chlorhexidine (CHX). In some cases it is necessary to apply a medical insert to the canals after reprocessing. The tooth is then temporarily closed and the root canals are filled in another session.
As after an initial treatment, the root canal system is definitely closed with a volume-stable and biocompatible filling material, usually with gutta-percha (1).
Root canal revision success rates
The success rate of the root canal revision treatment depends very much on the initial findings. Above all, whether a periapical lesion was present at the start of treatment is decisive for the prognosis. Friedman and Mor showed that initial treatments and revision treatments without inflammation at the root tip achieved success rates between 92% and 98% in the 10-year follow-up. If apical periodontitis is present, the chances of recovery drop to values between 74% and 86% (23). On average, success rates for revision treatments of 60% to 80% are given in the literature.
Individual evidence
- ↑ a b c d e Revision of a root canal treatment. Joint statement of the DGZMK and DGZ DGZMK 2/2004. Retrieved May 9, 2015.
- ↑ PN Nair, U. Sjögren u. a .: Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. In: Journal of endodontics. Volume 16, Number 12, December 1990, ISSN 0099-2399 , pp. 580-588, doi : 10.1016 / S0099-2399 (07) 80201-9 , PMID 2094761 .
- ↑ U. Sjögren, D. Figdor and a .: Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. In: International endodontic journal. Volume 30, Number 5, September 1997, ISSN 0143-2885 , pp. 297-306, PMID 9477818 .
- ↑ CJ Ruddle: Nonsurgical retreatment. In: Journal of endodontics. Volume 30, Number 12, December 2004, ISSN 0099-2399 , pp. 827-845, PMID 15564860 (review).
- ↑ JF Siqueira: Aetiology of root canal treatment failure: why well-treated teeth can fail. In: International endodontic journal. Volume 34, Number 1, January 2001, ISSN 0143-2885 , pp. 1-10, PMID 11307374 (review).
- ↑ a b A. Molander, C. Reit u. a .: Microbiological status of root-filled teeth with apical periodontitis. In: International endodontic journal. Volume 31, Number 1, January 1998, ISSN 0143-2885 , pp. 1-7, PMID 9823122 .
- ↑ V. Peciuliene, I. Balciuniene u. a .: Isolation of Enterococcus faecalis in previously root-filled canals in a Lithuanian population. In: Journal of endodontics. Volume 26, Number 10, October 2000, ISSN 0099-2399 , pp. 593-595, doi: 10.1097 / 00004770-200010000-00004 , PMID 11199800 .
- ↑ TM Waltimo, EK Sirén u. a .: Susceptibility of oral Candida species to calcium hydroxide in vitro. In: International endodontic journal. Volume 32, Number 2, March 1999, ISSN 0143-2885 , pp. 94-98, PMID 10371902 .
- ↑ TM Waltimo, EK Sirén u. a .: Fungi in therapy-resistant apical periodontitis. In: International endodontic journal. Volume 30, Number 2, March 1997, ISSN 0143-2885 , pp. 96-101, PMID 10332243 .
- ↑ a b c d L. Thiele, R. Hickel, M. Folwaczny, The endodontic failure - from definition to strategy ( Memento of May 18, 2015 in the Internet Archive ). Dtsch zahnarztl Z 58, 3: 144 (2003). Retrieved May 9, 2015.
- ↑ G. Lomçali, BH Sen, H. Cankaya: Scanning electron microscopic observations of apical root surfaces of teeth with apical periodontitis. In: Endodontics & dental traumatology. Volume 12, Number 2, April 1996, ISSN 0109-2502 , pp. 70-76, PMID 9028200 .
- ↑ L. Tronstad, F. Barnett, F. Cervone: Periapical bacterial plaque in teeth refractory to endodontic treatment. In: Endodontics & dental traumatology. Volume 6, Number 2, April 1990, ISSN 0109-2502 , pp. 73-77, PMID 2132213 .
- ^ BE Wayman, SM Murata et al. a .: A bacteriological and histological evaluation of 58 periapical lesions. In: Journal of endodontics. Volume 18, Number 4, April 1992, ISSN 0099-2399 , pp. 152-155, doi : 10.1016 / S0099-2399 (06) 81409-3 , PMID 1402568 .
- ↑ Siqueira jr, JF, Rocas, IN, Veiga, LM, Lopeas, HP, Oliveira, JCM, Alves, FRF: Causes of persistent postoperative complaints in endodontics. Endodontics 19, 29 2010
- ↑ Wu, M.-K., Wesselink, PR: Strategies for dealing with persistent post-endodontic diseases. Endodontics 17, 9 (2008).
- ↑ HS Koppang, R. Koppang u. a .: Cellulose fibers from endodontic paper points as an etiological factor in postendodontic periapical granulomas and cysts. In: Journal of endodontics. Volume 15, Number 8, August 1989, ISSN 0099-2399 , pp. 369-372, doi : 10.1016 / S0099-2399 (89) 80075-5 , PMID 2637329 .
- ↑ PN Nair, U. Sjögren u. a .: Therapy-resistant foreign body giant cell granuloma at the periapex of a root-filled human tooth. In: Journal of endodontics. Volume 16, Number 12, December 1990, ISSN 0099-2399 , pp. 589-595, doi : 10.1016 / S0099-2399 (07) 80202-0 , PMID 2094762 .
- ↑ Strindberg, LZ: The dependence of the results of pulp therapy on certain factors. Acta Odontol Scand 14, (suppl.21) (1956)
- ↑ YES Basel, the patency concept. Master's thesis , Department for Interdisciplinary Dentistry and Technology, Danube University Krems, Austria, (2010)