Listeriosis
| Classification according to ICD-10 | |
|---|---|
| A32.9 | Listeriosis |
| A32.0 | Cutaneous listeriosis |
| A32.1 † | Meningitis and meningoencephalitis due to Listeria |
| A32.7 | Listerial sepsis |
| P37.2 | Newborn listeriosis (disseminated) |
| ICD-10 online (WHO version 2019) | |
The Listeriosis is a by bacteria of the genus Listeria caused infectious disease in animals and humans. The most important pathogen is Listeria monocytogenes , which occurs worldwide and is highly contagious, but only has a moderate disease-causing effect . Infection with Listeria ivanovi or L. seeligeri also rarely occurs in humans .
Listeriosis is notifiable and occurs in humans especially in pregnant women and their unborn children as well as in newborns, in the elderly and in people with a weakened immune system ( AIDS patients, immunosuppressed ). The number of listeriosis in humans as a result of food infections - some of which are fatal - has increased in Europe in recent years. In the animal world, ruminants (cattle, sheep, goats) are particularly affected by the enzootic and epizootic disease. It rarely affects birds, horses and pigs, as well as rodents, fish and crustaceans, and very rarely predators.
For the spread of the disease in humans and animals, spoiled and contaminated food and feed play a role, which is why it is not a zoonosis in the classic sense - a disease that can be transmitted from humans to animals and vice versa - but rather a rot ( sapronosis ) or Earth germ infection ( geonosis ) is.
The clinical picture of listeriosis is very variable and depends primarily on the organ system affected. Therefore, the disease cannot be clinically determined with certainty, which is why adequate treatment with effective antibiotics is often too late. In the case of food infections, people generally experience diarrhea and abdominal pain first, but protracted sepsis can also occur. Most frequently, in the further course of the disease in humans and animals, central nervous disorders such as paralysis, tremors, physical deformities and drowsiness develop as a result of inflammation of the brain ( encephalitis ) and the meninges ( meningitis or meningoencephalitis ) . Miscarriages , death of the fetus, or severe neonatal sepsis can occur in pregnant women and pregnant animals . Finally, listeriosis can also manifest itself as a local wound infection and inflammation of the conjunctiva and cornea .
Listeriosis has been a reportable disease in Germany since 2001, both in humans and in animals .
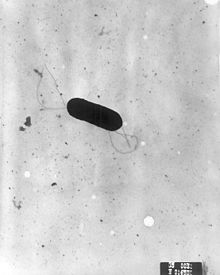
Pathogen
The most common pathogen is Listeria monocytogenes , a gram-positive rod 0.5 to 2 µm long and 0.4 to 0.5 µm wide. It forms flagella at temperatures below 30 degrees Celsius , above which it is mobile due to explosive polymerisation ( actin assembly-inducing protein ). It also grows in the absence of oxygen ( optionally anaerobic ). Listeria monocytogenes is extremely cold-resistant and reproduces even at refrigerator temperature. In addition, it is acid-resistant up to a pH value of 4.5 and also withstands high salt concentrations.
There are six serotypes . The virulence of the pathogen is mainly determined by the haemolysin gene (hly), which codes for the protein listeriolysin O (LLO). 90% of all human infections are caused by serotypes 4b, 1 / 2b and 1 / 2a. In the United States and Finland there are already databases in which the genetic patterns of the L. monocytogenes strains determined by pulsed field gel electrophoresis are recorded, so that cases of Listeriosis can be identified and combated quickly.
Listeria ivanovii also plays a role in sheep , but only in the shape of the uterus ( see below ). Other Listeria are not disease-inducing ( non-pathogenic ).
distribution

Listeria occur practically everywhere ( ubiquitous ). They are considered to be dirt germs and are particularly widespread in wastewater, soils and contaminated water, food and feed. Since Listeria are more likely to be seen as soil or putrefactive germs, the disease is also known as " geonosis " or " sapronosis ". There is practically no direct infection from animal to animal, animal to person or from person to animal.
The most common sources of infection for ruminants are inadequately fermented or soil-soiled silage with a pH value > 5.6 or rotten hay.
Almost every food contaminated with soil or dust contains Listeria, which is why fruit and vegetables or vegetable feed in particular are responsible for the infection. Exceptions are carrots, apples and tomatoes, in which the pathogen does not persist.
Food of animal origin is mostly secondary contaminated, so it is only inoculated with listeria during processing. Raw milk and butter are particularly at risk. Dairy products such as hard cheese, yogurt and quark, on the other hand, are considered safe. Proper pasteurization reliably kills Listeria. Pasteurized milk can, however, be contaminated again in the household, which can lead to an accumulation of listeria even if it is stored in the refrigerator. Mayonnaise , poultry and short-ripened raw sausages ( tea sausage , mettwurst ) are also critical foods. Listeria can multiply and form colonies, especially on the surfaces of raw and soft cheese and salami . Since in such cases only those people who happen to eat a piece of food with colonies become ill, while others who eat the same food do not, the explanation is particularly difficult here. In the case of vacuum-packed smoked salmon , contamination rates of up to 50% were found, although there are apparently only minor strains that are pathogenic to humans and food infections from smoked salmon are rare.
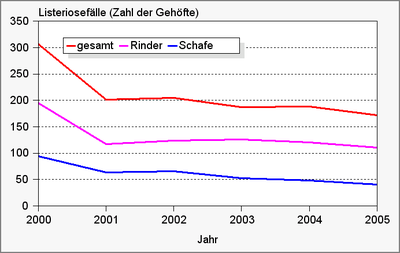
In Germany, 520 records of listeriosis in humans were reported for 2006, 707 for 2016, 770 for 2017, 698 for 2018 and 591 for 2019. Recently, an increase in Listeriosis cases as a result of food infections has been observed, while the number of newborn and pregnant women infections (see below) has remained constant. The former are usually individual illnesses, mostly in older people. The cause of this increase is not known. In the United States, L. monocytogenes is responsible for 28% of food-related deaths. In animals, cattle and sheep are mainly affected, in other animals listeriosis only plays a subordinate role. The number of outbreaks in cattle and sheep herds has shown a slight downward trend in recent years.
| Listeriosis cases in humans in Germany (according to information from the RKI ) |
Listeriosis cases in animals in Germany (according to information from the FLI ) |
|---|---|

|
|
Disease emergence
The infection occurs through the mouth (orally) or as a smear infection with soft tissue infections. The pathogen spreads in animals mainly via lymphatic vessels and along the cranial nerves V ( trigeminal nerve ) and XII ( hypoglossal nerve ).

In people with a weak immune system, L. monocytogenes has the ability to bind to E-cadherin by means of certain surface proteins (InlA, InlB and P60) and thus penetrate epithelial cells of the gastrointestinal tract and cells of other organs. Within the cells (intracellularly) L. monocytogenes survives in membrane-covered vacuoles and is thus protected from the mechanisms of unspecific defense. Even in macrophages , the pathogen can withstand intracellular degradation.
If certain virulence factors (listeriolysin, phospholipase) are present, the pathogen leaves these membrane envelopes and multiplies in the cytoplasm of infected cells. This results in granulomas ("listeriomas") scattered (disseminated) in the intestine . From these, the pathogen spreads through the blood ( bacteremia ) and colonizes other organs. Listeria have the ability to attach to the ends of the actin filaments of the cell structure and thereby move within the cells. Since actin filaments also radiate into certain cell contacts , Listeria are also able to penetrate neighboring cells and thus also overcome anatomical barriers such as the blood-brain barrier and the placenta .
The body reacts to the invasion of the pathogen with an immune reaction and normally develops cellular immunity . In infected, but not diseased organisms, the pathogen can be detected in the tonsils , the gastrointestinal tract and the liver . The disease usually only breaks out if the immune system is weakened. The pathogen therefore needs further factors in order to overcome the immune system and trigger a disease ( factor disease ). Infected animals and humans excrete the pathogen through the faeces and lactating animals also through the milk.
Listeriosis in animals
ruminant
- Sheep and goats
In sheep and goats, listeriosis can occur in four forms, although the disease is usually more dramatic in goats than in sheep.
The most common form is the central nervous form , in which neurological deficits occur due to an inflammation of the meninges . This form occurs mainly in 4 to 6 month old lambs and is mostly caused by L. monocytogenes type 4b. Typical symptoms are fatigue , turning movements (in English-speaking countries the disease is therefore also called circling disease ), drooping ears, trembling of the lips, trembling eyes and, in an advanced stage, lying on the side with rowing movements. In addition, tear and nasal discharge can often be observed. A hyperextension of the neck is rather rare, the reflexes are mostly undisturbed. The disease usually ends fatally within 10 days.
The metrogenic form (from the Greek metra " uterus ") manifests itself in miscarriages in pregnant ewes. The miscarriages are usually uncomplicated, i.e. without postpartum retention or endometritis . The trigger is usually L. ivanovii .
The septic form is characterized by the spread of pathogens in the blood ( sepsis ) and occurs mainly in lambs in the first few weeks of life. It is characterized by fever, weakness, reluctance to suckle and diarrhea. It usually occurs only sporadically in a herd, but is usually fatal for the animals concerned.
The shape of the eye shows up in conjunctivitis and corneal inflammation .
In sheep's differential diagnosis , Bornash disease , coenurosis , enterotoxemia , rabies , rumen acidosis , pregnancy ketosis , septicemic meningitis , abscesses of the brain and meninges, cerebrocortical necrosis , calcium or magnesium deficiency are particularly possible . Also, border disease , Spring disease , toxoplasmosis , scrapie , Visna , copper poisoning, botulism and tick paralysis are associated with central nervous system symptoms. Aujeszky's disease and Bradsot are usually peracute in sheep and can thus be clinically excluded.
- Bovine
Various forms also occur in cattle , with the central nervous and metrogenic forms dominating. Sepsis , keratoconjunctivitis and udder inflammation occur comparatively rarely, but are important because of the spread of germs.
In the central nervous listeriosis the pathogens reach presumably via mucosal lesions in the head area (for. Example, in the change of teeth) along the trigeminal nerve to the brain stem . By a usually unilateral encephalitis are core areas damaged by cranial nerves. Depending on the cranial nerves involved, there is usually one-sided paralysis of the corresponding muscles. The drooping of the eyelids can lead to inflammation of the cornea (so-called "exposure keratitis "). The incomplete lip closure and the impaired swallowing process lead to the loss of saliva. Due to the paralysis in the head area, the food and water intake are significantly impeded, which is why dehydration and the thickening of rumen contents and faeces soon occur. The damage to the sense of balance leads to tilting the head, pushing against the wall and later also to lying down. If left untreated, this form of listeriosis usually leads to death within 1–2 weeks.
Listeria-related abortions, stillbirths, and miscarriages occur experimentally about 7 days after intravenous infection. About 10% of spontaneous cases are associated with postpartum retention .
- Wild and zoo animals
Even in captive wild ruminants - especially pronghorn , Grant's gazelle , Blackbuck goats, wild sheep and, rare in deer - occur on listeriosis due to tainted feed from feed. The clinical picture is similar to that of domestic ruminants.
Other animal species
In birds, listeriosis usually takes the form of sepsis with unspecific symptoms and sudden death. Canaries and budgies are most commonly affected, but overall the disease is rare. Central nervous symptoms are also possible.
Central nervous disorders or abortions occasionally occur in horses and pigs. Listeriosis is very rare in dogs and cats. It can occur septicemically, with abortions or as a central nervous form in dogs , but mostly only in animals with impaired T-cell function, for example as a result of distemper . Cats mainly show a septicemic course with reluctance to eat, fatigue, vomiting and diarrhea, L. monocytogenes is occasionally involved in wound infections. In rabbits and rodents , listeriosis can manifest itself in the form of encephalitis with central nervous symptoms; in water pigs, the metrogenic form is also observed. In monkeys listeriosis occur most often at sea felines , less common in great apes , New World monkeys and Galagos on. As in humans, the central nervous and metrogenic forms with neonatal infections dominate , and liver inflammations are also observed.
Although reptiles are carriers of Listeria and excrete them, the significance as a cause of diseases in reptiles themselves has not yet been clarified. There is a confirmed case of a septicemic course in a bearded dragon after feeding pork containing listeria, which ended fatally after three days with microabscesses in various internal organs.
Veterinary pathology
From a veterinary pathological point of view, accumulations of white blood cells in the brain tissue ( leukocyte infiltrates) and meningitis with accumulation of lymphocytes (lymphocytic meningitis ) can be demonstrated in the central nervous form . Depending on the pathogenicity of the pathogen, abscessing , necrotic, or granulomatous processes also occur. It mainly affects the brain stem and the neck part of the spinal cord . A dry rumen content is relatively typical in sheep .
Septicemic forms are expressed as millet-sized (miliary) necroses in the liver and lungs, as well as bleeding under the inner lining of the heart (subendocardial) and the covering of the heart (subepicardial).
The metrogenic form shows itself in necrosis of the placenta , in ruminants in the area of the cotyledons .
Listeriosis in humans
Listeriosis in immunocompetent
Listeriosis is rare in immunocompetent people and the infection is usually symptom-free (inapparent). L. monocytogenes can persist in the gastrointestinal tract without causing clinical symptoms. In individual cases it can lead to flu-like symptoms, but these are self-limiting and therefore do not require therapy. However, recent studies indicate that after consuming foods heavily fortified with Listeria, severe gastrointestinal inflammation ( gastroenteritis ) can develop within 24 hours, even in otherwise healthy people . In humans, listeriosis probably always begins with gastroenteritis with abdominal pain and diarrhea. Since there can be a variety of causes here, it is often not fully diagnosed and specifically treated. Secondary symptoms can appear up to a few weeks later and are therefore often no longer associated with this event. According to the Occupational Diseases Ordinance, listeriosis is one of the occupational diseases in agriculture and the food industry, although this exposure is of little epidemiological importance and only plays a role in local skin and conjunctival infections.
Listeriosis in the immunocompromised
In an immunosuppression generally the risk of infection increases. Immunosuppression is usually acquired, e.g. B. by a virus infection ( HIV ), by an immunosuppressive therapy using cytostatics or glucocorticoids , which are used after an organ transplant or in the context of an autoimmune disease or blood cancer ( leukemia ). Chronic alcohol abuse also leads to a kind of immunosuppression. Natural, age-related immunosuppression also predisposes to infection.
Listeriosis in immunocompromised people is very often a serious, life-threatening disease. Several organs are often affected. The most common manifestation, affecting around a third of immunocompromised people, alcoholics and the elderly, is meningoencephalitis , which is most commonly manifested in the brain stem . In patients with liver cirrhosis one can peritonitis occur. Severe cases are acutely life-threatening. In the case of blood poisoning , the listeria are hematogenous and, as a result, there is a purulent inflammation of other organs ( heart valves , joints , bones , gall bladder ), and 12% of patients experience septic shock .
Angina with swelling of the lymph nodes with an increase in lymphomonocytic cells in the blood count is less common . These symptoms are called “pseudo- Pfeiffer ” (Paul-Bunnell-negative infectious mononucleosis).
With smear infection of the conjunctiva , conjunctivitis , corneal inflammation or uveitis can occur. Local skin infections can also occur.
Listeriosis in pregnant women and newborns
Pregnant women are about 12 times more likely to develop listeriosis. It usually manifests itself only as a flu-like short fever that is usually not taken seriously. However, an inflammation of the can placenta ( placentitis ) and set the infection pass to the unborn child ( congenital infection by placental transfer). With infections in early pregnancy (first trimester ), the embryo usually dies and an abortion occurs . Later infections, second and third trimester, lead to intrauterine listeriosis, which can lead to fetal death and thus to late abortion or to premature birth. With a perinatal infection the picture of a listeriosis infantiseptica can develop. The newborn can show symptoms immediately after birth (early-onset), or only a few days later, up to four weeks later; this is known as a late-onset . Despite intensive care medicine, the "early onset" disease has a very poor prognosis, with sepsis (blood poisoning), meningitis (meningitis) and pneumonia (pneumonia) frequently occurring . The mortality is 36%. With "late-onset" infection, the child usually acquires the listeria during the birth process. The disease usually manifests itself as meningitis. With a suitable therapy, the prognosis is better, the lethality is 26%.
In the differential diagnosis, a multitude of diseases can be considered in humans: diarrhea of other origins, viral infections such as Pfeiffer glandular fever and sepsis, meningitis and encephalitis caused by other pathogens.
diagnosis
The diagnosis can hardly be made clinically certain. The blood count shows an increase in the level of white blood cells ( leukocytosis ). The examination of the cerebrospinal fluid ( CSF ) is a pleocytosis with increased number of mononuclear cells. The pathological picture is also not characteristic. Serological examinations , i.e. the detection of antibodies , are of no significance.
Only a bacteriological examination can definitively confirm the diagnosis. The cultivation of the pathogen is usually problem-free, but it does not always succeed from the cerebrospinal fluid or from samples with strong involvement of other bacteria (feces, vaginal secretions). Molecular biological methods (DNA detection by polymerase chain reaction ) can help here, in particular the DNA of the bacteria can be detected very reliably in the cerebrospinal fluid in this way. If listeriosis is suspected, it is generally useful to take blood for blood cultures , as the pathogen can be grown from it in many cases.
In the case of meningitis, the suspicion of listeriosis usually arises from the detection of gram-positive rods in the cerebrospinal fluid. These are almost always listeria.
treatment
The biggest problem with therapy is that a reliable diagnosis can hardly be made in time, as the pathogen detection is not always successful. L. monocytogenes is sensitive to many antibiotics such as ampicillin , amoxicillin , erythromycin , gentamicin and sulfonamides , but treatment often begins too late due to the unclear symptoms. Another problem with the therapy is that the pathogen occurs optionally intracellularly, where it is not vulnerable to some antibiotics. In addition, the patients are usually immune to weakness, so that the body's own defense mechanisms do not adequately support the drug therapy.
Another problem is that cephalosporins - a group of antibiotics that are often routinely used and actually broadly effective - are not effective against Listeria. In a Spanish study, 50% of patients who empirically used cephalosporins died, but only 12% died when an antibiotic that was effective against listeria was used. According to other data, despite early treatment and the use of effective antibiotics, mortality is between 20 and 30%.
The therapy of choice is treatment with ampicillin, which is administered up to six times a day for 14 to 21 days, for meningitis, sepsis, brain abscess and endocarditis as well as newborns in combination with gentamicin . Erythromycin is used in the event of intolerance to β-lactam antibiotics .
prevention
The safest prophylaxis against food infections in humans is sufficient heating. Vegetables should be carefully washed and stored separately from raw meat. Hands, knives and surfaces should be washed well after contact with raw meat or vegetables. People with an increased risk of illness such as pregnant women, the elderly and the seriously ill should avoid raw meat, raw fish (salmon), raw milk and raw milk products such as raw milk cheese and reheat ready-made meals shortly before consumption.
For animals, avoiding the feeding of contaminated feed, spoiled hay or incorrectly fermented silage as well as avoiding stress and other factors that weaken the immune system are the most effective preventive measures.
In the USA, the Food and Drug Administration approved a bacteriophage- based product from Intralytix in August 2006 , which is sprayed onto food (especially meat) or surfaces that come into contact with food in food processing plants in order to kill listeria.
Reporting requirement
In Germany, the direct detection of Listeria monocytogenes in humans from blood, liquor or other normally sterile substrates as well as from smears from newborns must be reported by name if the evidence indicates an acute infection. In the case of animals, veterinarians, veterinary examination offices, animal health offices or other public or private examination centers are obliged to report after proof.
In Switzerland, is a positive laboratory analytical findings to listeriosis for doctors, hospitals, etc. notifiable and that after the Epidemics Act (EpG) in connection with the epidemic Regulation and Annex 1 of the Regulation of EDI on the reporting of observations of communicable diseases of man . In addition, the positive and negative laboratory analytical results for Listeria monocytogene for laboratories etc. must be reported in accordance with the standards mentioned and Appendix 3 of the EDI ordinance.
history
The disease was first described in 1923 by Everitt George Dunne Murray and coworkers in rabbits and guinea pigs in a laboratory animal facility in Cambridge. Three years later, Murray isolated the pathogen and named it Bacterium monocytogenes because of the high monocytosis in rabbits and guinea pigs .
In 1929, in Denmark, the first human case to be proven by culturing the pathogen was documented by Nyfeldt . Another description of listeriosis in humans was made according to Wurm and Walter in 1937. The first report in sheep was presented in 1931 by Gill from New Zealand, and in 1941 the disease was detected in chickens in Germany by Georg Pallaske . This was followed by evidence in cattle in the United States ( Johns and Little , 1935) and pigs ( Biester and Schwarte , 1940).
1940 was the pathogen on a proposal by JH Harvey Pirie after the British scientist Joseph Lister, 1st Baron Lister , in Listeria monocytogenes renamed.
Listeriosis was initially ignored as a disease, and the pathogen detection was more of a laboratory diagnostic curiosity. In 1952 Jürgen Potel from the Hygiene Institute at the University of Halle recognized the importance of L. monocytogenes for the newborn form (granulomatosis infantiseptica). With the development of effective immunosuppressive drugs from the 1950s and 1960s, listeriosis gained increasing clinical importance in humans. With the AIDS epidemic in the 1980s, the incidence of Listeriosis also increased, as AIDS patients have a 500-fold higher risk of developing the disease.
The knowledge that listeriosis in animals is a feed infection suggested that food should also be considered as a source of infection for humans. This thesis was proven with the first evidence of an endemic caused by contaminated food in 1981 in Halifax (Canada). Contaminated cabbage salad was the trigger for this - with 41 people affected, 83% of them pregnant women, and 17 deaths. There were further endemics in Le Vaud (Switzerland) (1983–1984 with 57 people affected by soft cheese, mortality 32%), in 1985 in California with 142 people affected and 48 deaths from consumption of Mexican cheese, 1992 (38 cases, mortality 32%) and 1999 (32 cases, mortality 31%) in France from pork and 1998/99 in the United States from hot dogs with 101 people affected and a mortality of 21%. A large number of those affected (1566), albeit without deaths, had a food infection from corn salad in Italy in 1997.
In August 2008, 24 people in Canada known to have died of listeriosis from eating contaminated meat found in ready-to-eat meals from Maple Leaf Foods , one of Canada's largest producers. The cause were hygienic deficiencies in the Toronto plant, which was closed by the Canadian authorities.
In Germany and Austria, eight people died at the end of 2009 after consuming Harz cheese contaminated with listeria .
After the death of at least five people from listeriosis, a vegetable factory in Texas / USA was closed in October 2010. Listeria has been detected in the celery processed by the factory .
Also in the United States, Listeria infection from contaminated melons occurred between July and September 2011 . 13 people died and dozens more fell ill. The melons came from a factory near Denver , on whose production machines and stored melons Listeria could also be detected.
In Denmark there were numerous illnesses and at least 12 deaths between September 2013 and August 2014 as a result of the consumption of various meat and sausage products from the manufacturer Jørn A. Rullepølser , which was then closed by the authorities.
In September 2019, three deaths from listeriosis were linked to the consumption of Wilke sausage products in northern Hesse . The operation was also closed due to further serious hygiene deficiencies, the company filed for bankruptcy.
Literature and Sources
- Heinrich Behrens et al. (Ed.): Sheep diseases . 4th edition. Paul-Parey-Verlag, 2001, ISBN 3-8263-3186-9 .
- Hartwig Bostedt, Kurt Dedie: Sheep and goat diseases . 2nd Edition. UTB, Stuttgart 1995, ISBN 3-8252-8008-X .
- M. Hamon et al.: Listeria monocytogenes: a multifaceted model . In: Nature Reviews Microbiology . No. 4 (6) , 2006, ISSN 1740-1526 , pp. 423-434 .
- H.-J. Selbitz: Listeria . In: Anton Mayr (Ed.): Medical microbiology, infection and epidemic theory . 7th edition. Enke-Verlag, Stuttgart 2002, ISBN 3-7773-1795-0 , p. 509-517 .
- Matthaeus Stöber: Listeriosis . In: Gerrit Dirksen et al. (Ed.): Internal medicine and surgery of the cattle . 4th edition. Verlag Parey, Berlin 2002, ISBN 3-8263-3181-8 , pp. 1239-1244 .
- W. Köhler among others: Medical microbiology . 8th edition. Urban & Fischer-Verlag, Munich / Jena 2001, ISBN 3-437-41640-5 .
- Werner Köhler : Listeriosis. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 857 f.
- Individual evidence
- ↑ Federal Institute for Risk Assessment: https://www.bfr.bund.de/de/listerien-54356.html Listerien
- ↑ Werner Köhler: Listeriosis. In: Werner E. Gerabek et al. (Ed.): Enzyklopädie Medizingeschichte. Berlin / New York 2005, pp. 857 f .; here: p. 857.
- ↑ Human: Section 7, Paragraph 1, No. 29 Infection Protection Act , Animal: No. 15 of Appendix 1 to Section 1 of the Ordinance on Notifiable Animal Diseases
- ↑ a b c d e f g Robert Koch Institute : Epidemiological Bulletin . December 8, 2006 / No. 49, pdf .
- ^ A b c Pascale Cossart: Listeriology (1926-2007): the rise of a model pathogen. In: Microbes Infect. 2007 May 6, PMID 17618157 .
- ^ JM Farber, PJ Peterkin: Listeria monocytogenes, a food-borne pathogen. In: Microbiological Reviews. 1991; 55, pp. 476-511.
- ↑ a b c d e f H. Hof et al.: Epidemiology of listeriosis in Germany - changing and yet ignored. In: Dtsch Med Wochenschr. 2007 Jun 15; 132 (24), pp. 1343-1348, PMID 17551889 .
- ↑ RKI: Epidemiological Bulletin No. 7 of February 16, 2017, p. 74
- ↑ RKI: Epidemiological Bulletin No. 3 of January 17, 2019, p. 28
- ↑ RKI: Epidemiological Bulletin No. 3 of January 16, 2020, p. 18
- ↑ a b c H.-W. Baenkler (ed.): Listeriosis. In: internal medicine. Thieme-Verlag 2001, ISBN 3-13-128751-9 , pp. 1226-1227.
- ↑ Shenoy et al .: A kinematic description of the trajectories of Listeria monocytogenes propelled by actin comet tails. In: PNAS . 2007; 104 (20), pp. 8229-8234. PMID 17485664
- ↑ a b c Reinhard Göltenboth, Heinz-Georg Klös: diseases of zoo and wildlife . Parey-Verlag, 1995, ISBN 3-8263-3019-6 .
- ↑ a b c K. Gabrisch, P. Zwart: Diseases of pets. 6th edition. Schlütersche Verlagsgesellschaft, Hanover 2005, ISBN 3-89993-010-X .
- ^ Katrin Hartmann: Listeriosis. In: Peter F. Suter, Hans G. Nobody (Hrsg.): Internship at the dog clinic. 10th edition. Paul-Parey-Verlag, 2006, ISBN 3-8304-4141-X , pp. 308-309.
- ↑ Reinhard Weiss: Listeriosis. In: Marian C. Horzinek et al. (Ed.): Diseases of the cat. 4th edition. Enke-Verlag, Stuttgart 2005, ISBN 3-8304-1049-2 , pp. 172-173.
- ↑ Elliot R. Jacobson: Bacterial diseases of reptiles. In: Elliot R. Jacobson (Ed.): Infectious diseases and pathology of reptiles . CRC Press, 2007, ISBN 978-0-8493-2321-8 , pp. 461-526.
- ↑ EA Antal et al.: Neuropathological findings in 9 cases of listeria monocytogenes brain stem encephalitis. In: Brain Pathol . 2005; 15 (3), pp. 187-191, PMID 16196384 .
- ↑ a b M. M. Suárez et al .: Listeria monocytogenes bacteremia: analysis of 110 episodes. In: Med Clin (Barc). 2007; 129 (6), pp. 218-221, PMID 17678604 .
- ↑ H. Hof: Chapter 29: Listeria monocytogenes and other Listeria. In: D. Adam et al. (Ed.): Die Infektiologie . Springer Verlag, Berlin 2004, pp. 945–952.
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 210 f.
- ↑ Jane Byrne: EPA approved antimicrobial could control listeria in food plants. July 1, 2008.
- ↑ Stephen Daniells: FDA approves viruses as food additive for meats. August 23, 2006.
- ^ Federal Register: August 18, 2006 Volume 71, Number 160, pp. 47729-47732.
- ↑ § 7 Paragraph 1 No. 29 Infection Protection Act (IfSG)
- ↑ § 1 of the Ordinance on Notifiable Animal Diseases
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid 1961, pp. 9-223, here: pp. 203 f.
- ↑ J. Potel: On Granulomatosis Infantiseptica. In: Central Bakteriol. I Orig 1952; 158, pp. 329-331.
- ↑ DB Louria include: listeriosis complicating malignant disease: a new association. In: Ann Intern Med . 1967; 67, pp. 260-281.
- ↑ RL Jurado et al .: Increased risk of meningitis and bacteremia due to Listeria monocytogenes in patients with human immunodeficiency virus infection In: Clinical Infectious Diseases . 1993; 17, pp. 224-227.
- ↑ Walter F. Schlechinger III: Foodborne listeriosis. In: Clinical Infectious Diseases. 2000; 31, pp. 770-775, PMID 11017828 .
- ↑ 57 sick including 24 dead in 2008 Maple Leaf Listeria outbreak: the scientific paper
- ↑ Change of law after eight Listeria deaths. Agrar heute , March 24, 2010, accessed on March 26, 2018 .
- ^ DSHS Orders Sangar Produce to Close, Recall Products. Texas Department of Health Services October 20, 2010, archived from the original September 7, 2015 ; Retrieved October 22, 2010 .
- ↑ Listeria infection: 13 Americans die from contaminated melons. In: Spiegel Online . September 28, 2011, accessed September 28, 2011 .
- ^ Deaths in Denmark: Contaminated sausages also in Schleswig-Holstein. In: Spiegel Online.
- ↑ "Extensively contaminated". In: Spiegel.inline
Web links
- Listeriosis - information from the Robert Koch Institute