Bronchopulmonary dysplasia
| Classification according to ICD-10 | |
|---|---|
| P27.1 | Bronchopulmonary dysplasia originating in the perinatal period |
| ICD-10 online (WHO version 2019) | |
Bronchopulmonary dysplasia ( BPD ) is a chronic lung disease that occurs primarily in premature babies with a low birth weight when these children are artificially ventilated for a long time , for example to treat newborn respiratory distress syndrome (IRDS). It can lead to protracted damage to the lungs into early adulthood or, with progressive lung changes, to death. Depending on the severity and effectiveness of the treatment, improvement can often be achieved in the first year of life.
frequency
The incidence of BPD decreases with increasing gestational age . Approx. 15–30% of preterm infants with a birth weight <1000 g or <32 weeks of gestation develop BPD, in preterm infants above 32 weeks of gestation BPD rarely occurs. Immature lungs with a lack of surfactant are a major risk factor for the occurrence of BPD. High ventilation pressure, high oxygen concentrations and long duration of artificial ventilation, a non-occluded ductus arteriosus and infections of the lungs are further factors. The development of BPD is the result of remodeling processes with inflammatory formation of connective tissue after initial water retention in an immature lung that is exposed to chemical (oxygen radicals), mechanical (pressure trauma, volume trauma) and biological (microbial pathogens) damage. Affected are the alveoli, the airways and the blood vessels in the lungs, which constrict and can then lead to increased pressure in the pulmonary circulation and a burden on the right ventricle.
diagnosis
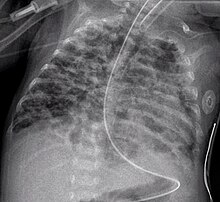
Clinical symptoms can be increased respiratory rate, deepened, strained breathing with retractions on the chest, increased bronchial secretions, cough, growth retardation and livid skin and mucous membranes. The x-ray of the lungs shows, among other things, diffuse areas of overinflation next to insufficiently ventilated areas ( atelectasis ). Diagnosis and classification are based on the oxygen requirement necessary for adequate oxygen saturation of the blood at a specified age of the child. By definition, the requirement at the time of a corrected age of 36 weeks of pregnancy (SSW) is decisive. A distinction is made between a mild (at 36 weeks no more increased oxygen demand), moderate (less than 30% oxygen in the inhaled air necessary) and severe (more than 30% and / or ventilation or respiratory support by CPAP necessary).
prevention
Measures to prevent BPD are: Avoidance of premature birth, induction of lung maturity before birth with the administration of corticosteroids to the mother, avoidance of infections, gentle ventilation that is as short as possible while accepting increased carbon dioxide blood gas levels, early diagnosis and closure of an open ductus arteriosus, possibly vitamin A administration to the child.
The use of surfactant in premature babies with respiratory distress syndrome, which was introduced in the late 1980s, has significantly improved the chances of survival for premature babies with BPD, but does not prevent the occurrence of BPD.
Treatment with systemic corticosteroids such as dexamethasone leads to a rapid improvement in lung function and, if given very early (in the first 96 hours of life), can also lead to a reduction in the incidence of BPD; however, if given early, the side effects are more severe and more frequent. Systemic corticosteroid treatment favors the occurrence of cerebral palsy.
therapy
The administration of oxygen to maintain an oxygen saturation of the blood of> 92% is the primary therapy. Corticosteroids (systemic or inhalation) counteract the chronic inflammatory process, but must not be used uncritically. The side effects such as B. hyperglycaemia , gastric ulcers and intestinal bleeding, development of osteoporosis etc. should be taken into account. Drugs that use water ( diuretics ) are used to treat pulmonary edema. If the airways are narrowed, inhalation with bronchospasmolytics is an option. Physiotherapeutic treatment should be carried out early and continuously. Medication that dilates the blood vessels can reduce increased pressure in the pulmonary circulation. Due to the increased energy requirements of the sick children, it is important to ensure that they eat a high-energy diet. The first vaccinations against whooping cough, pneumococcal and haemophilus influenzae infections must be carried out before discharge from the clinic. Since children with BPD are at great risk from RSV infections, the preventive administration of monoclonal antibodies against this virus infection should also be considered in the winter months in the first year of life if the disease is severe. Vaccination against influenza is recommended from the age of 6 months .
Individual evidence
- ↑ E. Eber, MS Zach: Long term sequelae of bronchopulmonary dysplasia (chronic lung disease of infancy). In: Thorax. 2001; 36, pp. 317-323.
- ↑ H. Christou, D. Brodsky: Lung injury and bronchopulmonary dysplasia in newborn infants. In: J Intensive Care Med. 2005 Mar-Apr; 20 (2), pp. 76-87.
- ↑ AH Jobe, E. Bancalari: Bronchopulmonary dysplasia. In: Am J Respir Crit Care Med. 2001; 163, pp. 1723-1729.
- ↑ RD Bland: Neonatal chronic lung disease in the post-surfactant era. In: Biol Neonate. 2005; 88 (3), pp. 181-191.
- ↑ HL Halliday, RA Ehrenkranz: Early postnatal (<96 hours) corticosteroids for preventing chronic lung disease in preterm infants. The cochrane library, Oxford 2000, Update software.
- ↑ HL Halliday, RA Ehrenkranz, LW Doyle: Moderately early (7-14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. In: Cochrane Database Syst Rev. 2003; 1, p. CD001144.
- ↑ G. Marckmann, D. Niethammer: Ethical aspects of pediatric research: To the introduction. P. 5.