German Diagnosis Related Groups
German Diagnosis Related Groups , G-DRG system for short , in German : diagnosis-related groups or, better, diagnosis-related case groups , is a uniform flat-rate system in health care that is linked to diagnoses. It replaced the old mixed system in Germany in 2003. The legal basis is § 85 SGB V and § 17b Hospital Financing Act .
Emergence
Up to the year 2002, around 80% of inpatient hospital services were billed using the same daily care rates and around 20% using flat rates or special fees, mainly in the surgical area.
Based on the original Australian model, the clinics have been calculating optional since 2003, and since 2004 all acute hospital services have been compulsory on the basis of flat-rate per case, i.e. H. DRGs, from. Departments and clinics for psychiatry, psychosomatics and psychotherapeutic medicine are generally excluded from this. In addition, highly specialized facilities can apply to be removed from the DRG system for a limited period of time if their services cannot yet be mapped in the DRG system according to the effort.
Every year, the system is adapted to the special circumstances in Germany with effect for the following year. The aim is to be able to map all inpatient “somatic” services with this “flat-rate remuneration system” in a manner appropriate to their performance. The Institute for the Hospital Remuneration System (InEK) in Siegburg is in charge of the introduction and revision of the DRG system .
The introduction of the DRG in 2003 and 2004 was budget-neutral, i. H. the amount of the hospital budget was negotiated and determined according to the classic model, but the billing was already carried out via DRGs.
introduction
The so-called option model made it possible for hospitals to convert their billing to the G-DRG system on a voluntary basis from January 1, 2003. In addition to timely registration, the prerequisite was a completed budget negotiation with the cost bearers. Due to time delays in budget negotiations, most of the participating clinics switched to during the year.
From January 1, 2004, the introduction of the DRG system was mandatory. However, since the completed budget negotiation was a prerequisite for the introduction, many clinics were only able to bill according to DRGs during the course of the year. A number of hospitals only started billing according to DRG in 2005.
Update of the German DRG system
When the DRG system is updated, it is adjusted based on the development of expenditure and costs using the various levers without changing the basic structure. This can result in:
- Differentiation of DRGs based on cost differences e.g. B. due to comorbidities, age, performed (non-surgical) procedures,
- Summary of previously different DRGs due to the lack of cost differences,
- the use of additional criteria such as birth weight, one-day case, emergency.
Compared to the Australian original, significant changes were made in 2005; the influence of the secondary diagnoses on the classification in a certain DRG is less than in previous years. In contrast, the importance of the procedures has increased significantly.
Further development
The DRGs have partially achieved the desired cost containment. The main finding, however, is that the DRGs alone do not achieve sufficient control intervention. Attempts are increasingly being made to achieve this through concepts of integrated care. However, unlike the DRGs for integrated care, a status of republic-wide uniformity cannot be foreseen in a predictable time.
The introduction of the flat rate per case resulted in a reduction in the number of nursing staff. This development should be counteracted with additional remuneration in the form of surcharges, additional fees (according to PKMS or care level ). Due to the inadequate effect, the maintenance costs for 2020 were calculated outside of the case-based flat rates and reimbursed through separate flat rates. At the end of the year, the remuneration within the framework of these flat-rate nursing care fees is offset against the costs actually incurred.
Basics of the German DRG system G-DRG
G-DRG (German-DRG) is the name for the German adaptation of the Australian DRG system ( AR-DRG ). It has been mandatory for all hospitals since 2004. According to Section 17b of the KHG , the German Hospital Association (DKG), the central associations of health insurers (GKV) and the Association of Private Health Insurance (PKV) are jointly responsible for the introduction of a flat-rate remuneration system.
The G-DRG catalog is divided into main diagnostic groups (Major Diagnostic Category MDC ) chapter by chapter .
Requirements: grouping of patients, encryption, evaluation relations
A prerequisite for classifying a patient in a DRG is the encryption of a main diagnosis and, if applicable, treatment-relevant secondary diagnoses as an ICD code and the essential services ( procedures ) performed on the patient as an OPS code.
In order to ensure uniform encryption, a set of rules ( German coding guidelines or DKR) was created. From the diagnoses and procedures as well as the age, gender, weight information for newborns, the number of hours of mechanical ventilation, the length of stay and the type of discharge (e.g. relocated, deceased, normal discharge, etc.), the DRG is determined by a from the Institute for the hospital remuneration system (InEK) created and published algorithm ( definition handbooks ). This algorithm is implemented in EDP programs, so-called DRG groupers , which are certified by the InEK and can be integrated into the EDP systems via interfaces from the hospital and the health insurance companies.
unification
The InEK annually compiles the catalog of billable DRGs from the performance and cost data of hospitals that voluntarily participate in the so-called calculation . In addition, an evaluation ratio (BR) (synonym: cost weight, relative weight ) is calculated for each DRG , which reflects the cost difference between the various DRGs. Therefore, the DRG system is primarily an economic and only to a limited extent a medical classification.
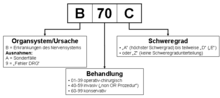
The DRGs are displayed as a four-digit combination of letters and numbers, for example F60B for circulatory diseases with acute myocardial infarction, without invasive cardiological diagnostics and without extremely serious comorbidities . The three-digit combination of the DRGs is referred to as Basis-DRG (e.g. A01) and the four-digit combination as G-DRG (e.g. A01A; A01B).
The first digit of the DRG code designates the chapter (so-called main diagnostic group , from the English Major Diagnostic Category (MDC)) according to the organ system (e.g. MDC 1: Diseases of the nervous system = B ) or cause of the disease (e.g. MDC 21: Injuries = X ) divided. In addition, there are special cases (ventilation cases, transplants, etc. = A ) as well as so-called error DRGs (incorrect main diagnosis, OP does not match diagnosis, etc. = 9 )
The second and third digits of the DRG code indicate the type of treatment. In the original Australian system, 01–39 denotes surgical treatment (partition O), 40–59 denotes a non-operative but invasive treatment such as a colonoscopy (partition A) and 60–99 denotes purely medical treatment without interventions (partition M). In the German adaptation of the G-DRG system in 2005, the boundary between the operative and the non-OR partition, ie between the numbers 01–39 and 40–59, was softened, so that now also DRGs that require surgical treatment , with digits greater than 39 exist. The basic DRG I95 for tumor endoprosthesis in the G-DRG system version 2006 is given as an example.
The last digit of the DRG code indicates the (economic) severity of the DRG. The letter A indicates a complex (expensive) treatment. Depending on the basic DRG, various differentiations are possible downwards, currently up to the letter I. The letter Z indicates DRGs that are not further differentiated.
The price to be billed for the flat rate per case results from the calculated relative weight multiplied by a so-called base case value , which was negotiated on a hospital-by-hospital basis in 2003 and 2009, but was gradually adjusted to a base case value that is uniform for the federal state (state base case value, LBFW) between 2005 and 2009 ( Convergence phase ), so that from 2010 the same services within a federal state also have the same price, regardless of the hospital in which the patient was treated. From 2010 to 2014, in accordance with Section 10 (8) KHEntgG, the LBFW is to be gradually aligned nationwide to a base rate corridor of +2.5% to −1.25% of the uniform base rate.
To take into account outlier cases, i.e. patients who have been treated for an extremely long or particularly brief period, there is an upper and a lower limit of length of stay for most DRGs. If the length of stay is below the lower limit , a discount is applied; if the upper length of stay is exceeded, there is a surcharge on the respective DRG price. In addition, a deduction is made if the patient is transferred to another hospital or from another hospital and is not treated for at least the mean length of stay of the DRG invoiced. Surcharges and discounts are defined as valuation ratios per day, so that the respective amount results from the multiplication of the relevant days and the valuation ratio with the base rate.
DRG calculation variables
The DRG calculation variables include the following:
- Valuation ratio : The valuation ratio (or relative weight) is the revenue equivalent that is determined individually for each DRG on the basis of a cost calculation. The cost calculation is carried out by the Institute for the Hospital Remuneration System (InEK)
- Case mix (CM): The case mix is the sum of the valuation ratios of all DRGs provided within a time unit
- Case mix index (CMI): The CMI is calculated from the case mix divided by the number of cases
- Base rate (base rate): The base rate is agreed at the state level in accordance with Section 10 (1) KHEntgG and adjusted from 2010 to 2014 in five equal steps to the nationwide uniform base rate corridor.
aims
The goals of the DRG introduction are
- to shorten the length of stay in German hospitals
- to standardize the payment of medical services in hospitals ( same price for the same service ),
- Increase the transparency and comparability of hospital services,
- reduce suspected overcapacities in the hospital sector,
- overall to limit future expected cost increases in the inpatient area.
Development of the G-DRGs
| 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G-DRG main departments | 664 | 824 | 878 | 954 | 1082 | 1137 | 1192 | 1200 | 1194 | 1193 | 1187 | 1196 | 1200 | 1220 | 1255 | 1292 | 1318 |
| G-DRG document departments | 806 | 762 | 748 | 771 | 933 | 882 | 873 | 857 | 844 | 835 | 824 | 815 | 799 | 814 | 824 | 825 | |
| Minimum valuation ratio | 0.122 | 0.113 | 0.118 | 0.117 | 0.106 | 0.111 | 0.119 | 0.130 | 0.140 | 0.141 | 0.145 | 0.135 | 0.123 | 0.141 | 0.151 | 0.205 | 0.210 |
| Maximum valuation ratio | 29,709 | 48.272 | 57.633 | 65,700 | 64.899 | 68.986 | 78.474 | 73.763 | 72.926 | 65.338 | 62,477 | 64.137 | 65.943 | 68.208 | 61.787 | 71.528 | 71,598 |
| span | 29,587 | 48.159 | 57.515 | 65,583 | 64.793 | 68.875 | 78.355 | 73.633 | 72.786 | 65.197 | 62,332 | 64.002 | 65.820 | 68,067 | 61.636 | 71,323 | 71.388 |
criticism
In Germany, the DRG system has been criticized since it was founded in 2003, among other things, because it leads to a commercialization of the health system and the associated significant increase in the workload of nurses and doctors.
Practical implementation
The division of labor in hospitals has changed with the introduction of DRG billing. Since the introduction of DRG accounting, medical documentaries and medical documentation assistants have also been used occasionally in hospitals. The coder's field of activity, which is already known in other countries, is new . This is to relieve the doctors so that they can devote themselves to their actual task. This concept has been asserting itself across Germany since 2010 due to the increasingly complex requirements in the coding and billing context. The doctor's knowledge is still necessary for the correct presentation of the individual case in the patient records, so that the documentation work remains on the side of the doctors. If the code is incorrectly coded, the cases will be refused for payment by the medical service of the health insurance funds after the examination , which means a considerable additional effort for additional documentation and considerable losses in income for the hospitals. As a result, health insurances are more and more inclined to carry out precise case checks, as the post-documentation effort for many DRGs is not worthwhile for the hospital and this would result in effective cost savings for the insurer.
A coding accompanying the treatment (case management under DRG conditions) also ensures proximity to the patient in the coding.
The shortening of the length of stay leads to an increased workload for the nursing staff and the doctors, because it increases the proportion of patients with increased treatment and care costs in the hospital.
administration
In the administrative area of the service providers and the cost units, the expense for billing has increased. While up until now the price for a treatment was relatively easy to determine by multiplying the treatment days and recording individual services, medical knowledge is now required for the list, such as checking the ICD, OPS and DRG codes.
The DRG system increases the complexity and level of detail of the coding. While in countries like Switzerland coding is done by professional documentation assistants, in Germany the coding of diagnoses and procedures in some hospitals is still a task of the doctor, which is revised by coders. This significantly increases the administrative work of the hospital doctors, leaving less time for the patients.
Due to the constantly increasing complexity of the G-DRG system and its constant further development, the occupational profile of the medical coding specialist (MKF) is now gaining more and more importance across Germany as well. Coders should ideally be able to demonstrate a combination of medical background knowledge, advanced knowledge of the DRG system, business management expertise and practice-oriented IT skills.
In German clinical practice, the flat rate covers any requirement for detailed operating accounting. In fact - as in other countries - in Germany the classifications are checked and corrected by specialists at both the service provider and the cost provider. Finally, 10–20% of the accounts are objected to due to a lack of individual evidence and renegotiated. Whether the billing basis created in this way with a time delay to the service rendered is revision-proof, depends on the level of detail in the primary recording and whether the resulting encryption and subsequent changes can be traced.
Participation in the annual DRG recalculation is voluntary for hospitals. This is usually based on post-accounting surveys with estimates of the individual personnel costs. As a result, the incoming data are representative, but not increasingly more authentic than in the previous year.
The regular adjustments to the DRG cost weights lead to more or less strong fluctuations in remuneration, which can be associated with considerable financial risks for the hospitals.
The accompanying research stipulated by the legislator in Section 17b (8) of the Hospital Financing Act to be submitted by the end of 2005 was only commissioned in May 2008 through a tender in the Official Journal of the European Union.
The profitability of the system is questioned in a report by Plusminus magazine dated March 25, 2008.
Combat the rise in costs
The goal of combating the rise in health care costs was not achieved with the introduction of the DRG, and the costs rose unabated. In September 2013, the Lower Saxony Hospital Society criticized the fact that the flat-rate case fees only incompletely cover the costs of medical treatment in the hospital. Since its introduction, these have increased by 8.5 percent. The general price increase was 15.2 percent.
The increase in ventilation hours per case from 2002 to 2004 from 1.6 to 3.2 million is associated with the DRG system, since the health insurers pay more for the ventilation hours, which is a complex procedure.
Distribution and control function
Due to the measurement principle of relative costs and distribution from the total budget, there is no economic incentive to reduce the total costs. Because the procedures carried out, secondary diagnoses and complications and apparatus times that have been carried out, the lump sums are charged with additional amounts, there is still the incentive to report a higher level of complexity than may actually be required for the best outcome .
While the billing based on the length of stay was an economic incentive for an extension of the treatment, the billing according to the DRG flat rate case is an incentive for a rather early discharge ( bloody discharge ). Patients stay in hospital shorter per case, but with more consecutive stays in hospital ( revolving door effect) . A negative revolving door effect could not be proven in the previous, larger studies in Germany as well as in Switzerland. In order to prevent a possible negative effect, hospitals do not receive an additional flat rate per case if a patient has to be admitted to the hospital again within a certain period because of the same illness or complication.
Because the sum of the flat-rate services determines the contribution margin that can be achieved, individual institutions shift their interest to the lucrative cases, while the degree of care available decreases in the less lucrative cases. A case flat rate system offers incentives to specialize in the most “simple” or standardized cases within case groups. The supply of more complex cases is restricted locally or shifted to other providers with supply mandates. These so-called extreme cost cases then accumulate in maximum care clinics, which cause deficits worth millions there and bring these clinics to the brink of economic survival.
There is a disadvantage for occupational groups that are not relevant to revenue, such as care and housekeeping. These positions have been reduced, which has accordingly worsened patient care and increased the workload.
Coding quality
The DRG are generated with the help of a computer program (" grouper ") certified by the Institute for the Remuneration System (InEK) in the hospital from the diagnosis and procedure catalogs (ICD-10-GM and OPS) as well as additional case-related variables (e.g. age of the patient , Length of stay, number of hours of mechanical ventilation, etc.). The inclusion and exclusion criteria of the individual ICD and OPS codes as well as the German coding guidelines (DKR) of InEK GmbH must be observed.
- The effort involved in coding and checking is not insignificant.
- There is no uniform system for the suggestions for coding immediately after the admission diagnosis, this is only supplemented by business records.
- A clear (subjective) assignment is possible at any time on the basis of clinical pathways, operational procedures and medically oriented classifications.
If the coding quality is poor, not all of the information required for the case is used for coding, so that the optimum and correct relative weight for the case is not achieved. On the other hand, entering superfluous diagnoses and procedures that do not correspond to the DKR can lead to an excessively high relative weight.
Especially in the field of internal medicine with old and multimorbid patients (ie patients with several diseases), the system is not suitable for ensuring a consistently comprehensible image. Many inconsistencies in the ICD-10 also contribute to this. Studies in several German clinics have shown that the rate of different codings for the same information about a clinical picture is considerable; up to 40% of the codes differ considerably from one another.
The coding and the encryption by specialized but not medically trained personnel, which are often not carried out promptly, make the coding process the goal of billing optimization, regardless of its formal quality.
It can be seen that the coding does not initially provide an objective, revision-proof billing basis. This can be seen in the large number of responses from the medical service of the health insurance companies to billing clinics. Statistics on this response rate are not published.
Especially in certain areas (trauma surgery, paediatrics, palliative medicine, etc.), the DRG do not yet reflect the actual treatment in a sufficiently differentiated manner, so that the resulting remuneration is not in line with the expenditure.
Increasingly with each new DRG version, DRGs are not defined according to the underlying diagnosis, but only according to the procedure carried out (the main intervention). This creates an incentive to carry out and bill for complex procedures, regardless of whether the patient in question required this procedure. The Australian system, with its severity classification, offered a suitable set of instruments against this; however, these advantages are being used less and less.
Upcoding
Upcoding in the German DRG system refers to any increase in CMI that is not due to an average increase in severity, but to a change in coding behavior (mostly due to unjustified coding of secondary diagnoses to increase the PCCL ). In general, a CMI increase that is generated by better coding quality is not referred to as upcoding . A better coding quality, on the other hand, is desirable from all sides and is actively promoted.
Precision, timeliness
The DRG are not an aid for providing medical services, but merely an instrument for accounting for services. In this respect, the introduction of DRG accounting has slowed down the transition from retrospective order cost accounting based on cost center accounting to online process cost accounting, or even halted this development.
In German hospitals today, if at all process-oriented calculations are carried out, a classic process cost calculation on the basis of surveys of insufficient granularity with subsequent detailing is carried out. For this purpose, many cost elements are extracted from large cost blocks by means of a complex statistical analysis instead of being recorded online as automatically as possible when they arise.
authenticity
There is hardly a hospital in Germany that records costs and provides evidence that meets the wording of the requirements of Section 63 ff. SGB X and the principles of modern cost management. This is justified by reference to the wording of the legal text in a variety of and contradicting ways.
Change in medical thinking
In 2002, Helmut Schlereth wrote critically about the introduction of the DRGs: “This will change the medical way of thinking immensely. The unbearable stammering that the computer programs utter will creep into the doctors' brains, and pathophysiological thinking is bled out. [...] "
See also
- Base rate
- DRG Watchdog , a database that is accessible free of charge with a search mask for diagnostics relevant to remuneration.
- Hospital funding
literature
- InEK gGmbH (ed.): G-DRG case flat rate catalog 2008. ISBN 978-3-940001-11-5 .
- InEK gGmbH (Ed.): German Coding Guidelines Version 2008. ISBN 978-3-940001-12-2 .
- Boris Rapp: practical knowledge DRG - optimization of structures and processes. Kohlhammer-Verlag, 2007, ISBN 978-3-17-019396-3 .
Web links
- official coding guidelines according to DRG
- More information on the subject of ICD-10 and OPS keys
- Webgrouper
- myDRG - discussion forum u. Case mix - news
- Medinfoweb
- Criticism of the system and handling of the D-DRG system
- drg-server.de - All flat rate catalogs since 2003 with search function
- The patient and the flat rate case - a critical balance after ten years of DRG in Germany
Remarks
- ↑ see, for example, the specialty children's clinics that were particularly threatened in 2013. www.ichbinkeinefallpauschale.de
Individual evidence
- ↑ Final report: Further development of the aG-DRG system for 2020 by InEK from December 18, 2019, accessed July 11, 2020
- ↑ Falk Osterloh: Criticism of the DRG system. In: Falk Osterloh: Reform of the emergency care. Praise and criticism for the bill. In: Deutsches Ärzteblatt. Volume 117, Issue 3, January 17, 2020, pp. B 49 - B 55, p. B 54.
- ↑ Doctors and nurses are charged with flat rates per case on 11 July 2011.
- ↑ KPMG magazine 'Healthcare Check-Up, SwissDRG - Angekommen in der neue Welt' , p. 5, accessed on August 27, 2013.
- ↑ L. Kuntz, S. Scholtes, A. Vera: DRG Cost Weight Volatility and Hospital Performance. In: OR Spectrum. Volume 30 (2008), No. 2, p. 331 ff.
- ↑ Announcement in the Official Journal of the EU
- ↑ Plusminus: Incorrect hospital bills, March 28, 2008 ( Memento from June 12, 2008 in the Internet Archive )
- ↑ The Federal Health Reporting (GBE) ( Memento of the original from March 15, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. . In the "Expenses, Costs, Financing" area, the expenses for inpatient treatment have been available since 1992, but not linked.
- ↑ 2Drittel.de
- ↑ Publication 01.2013.
- ↑ FAQ page of the SwissDRG ( Memento of the original from October 2, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. , accessed August 27, 2013.
- ↑ Publication 01.2013.
- ↑ DGGÖ annual conference, Berlin 2010 (PDF; 1.0 MB)
- ↑ § 21 SGB X evidence
- ↑ § 67b SGB X consent
- ↑ § 78b SGB X data avoidance
- ↑ § 98 SGB X Execution of the contract
- ↑ § 101 SGB X Obligation of service providers to provide information
- ↑ Würzburg medical history reports 22, 2003, p. 611 f.