Cross match (medicine)
In the case of blood transfusions , a cross match , or correctly actually serological compatibility test , is an in vitro test of the compatibility of donor and recipient blood . Crossmatches are used to rule out intolerances due to different blood groups . Both intolerances due to AB0 blood groups and other reasons, such as rhesus intolerance , are excluded. After mixing, it can be examined macroscopically and with a light microscope whether clumping (agglutination) has occurred.
The in vitro testing
The serological compatibility test is intended to investigate and determine whether there are antibodies in the blood to be transfused (the " blood reserve ") and / or in the patient's or recipient's blood which trigger a hemolytic transfusion reaction. The serological tolerance test or cross match consists of three stages:
Table salt test (1st stage)
Represents the actual cross match and is carried out in physiological sodium chloride solution .
Large cross sample (major sample)
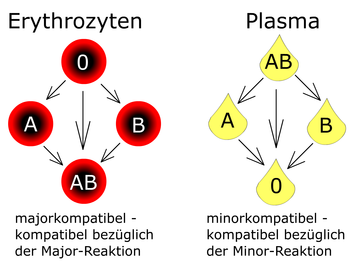
In the major reaction (“large cross match”), the donor's erythrocytes separated from the serum are mixed with the recipient's blood serum . If the recipient's serum contains antibodies against the donor's erythrocyte antigen, agglutination occurs . Agglutination is an absolute contraindication to blood transfusion .
Small cross sample (minor sample)
In the minor reaction (“small cross match”), the recipient's erythrocytes are mixed with the donor's blood serum. If the minor sample is positive and the major reaction is negative , a blood transfusion can still be carried out, as the donor's antibodies are greatly diluted in the recipient's blood. This type of cross match is rarely used today, as the blood stored is mostly red cell concentrates .
Albumin test (2nd stage)
Search for incomplete antibodies that do not cause agglutination in the physiological salt environment. For this purpose, the samples are mixed with a bovine albumin solution (30% albumin solution, also BSA , in English b ovine s erum a lbumin ), incubated for about 40 minutes at 37 ° C. and then centrifuged. Complete antibodies are antibodies of the IgM type, such antibodies are large enough that their Fab binding sites ( Fab fragments ) can bridge the natural distance between the erythrocytes. Therefore they are able to agglutinate the erythrocytes without further additives. In contrast to this, the incomplete antibodies are antibodies of the IgG type. Since these antibodies are smaller than the complete IgM antibodies, they are not able to bridge the gap between the erythrocytes without the addition of a Coombs or anti-human globulin serum. Without such an addition of serum, there is no detectable agglutination despite an antigen-antibody reaction, which means that serological detection in the test mixture is not possible. This is only possible by adding the Coombs serum.
Direct Coombs test (3rd level)
With the direct Coombs test , immunohematological evidence can be provided as to whether the patient's erythrocytes are loaded with incomplete antibodies (immunoglobulins or complement factors). If it is irregular antibodies of the immunoglobulins of the IgM class , agglutination will already occur at this stage . The direct Coombs test is carried out when a positive self-sample in the indirect Coombs test is available.
The indirect Coombs test detects circulating antibodies in the serum. The incomplete antibodies, so-called non-bound antibodies of the IgG type circulating in the serum, can only lead to agglutination when the Coombs or anti-human globulin serum is added. Without the addition of the Coombs serum, the detection of irregular antibodies of the immunoglobulins of the IgG class cannot be successful, as they lack the bridging character and so the individual erythrocytes cannot agglutinate. The test is particularly important for the detection of incomplete antibodies in the serum, antibody search test . The indirect Coombs test is carried out in two laboratory clinical steps. In the first step, the blood plasma to be examined is incubated with defined test erythrocytes . If the examined patient serum contains antibodies, binding to the test erythrocytes occurs, but not agglutination. Only in the second step, when the Coombs serum is added to the previously treated (incubated) test erythrocytes, does agglutination occur if the result is positive.

literature
- Reinhold Eckstein: Immunohematology and Clinical Transfusion Medicine: Theory and Practice. Elsevier, Munich 2010, ISBN 3-4372-10343
Web links
- Transfusion medicine. University Medicine. Georg-August-University Goettingen. Center for Hygiene and Human Genetics. Transfusion Medicine Department
- Laboratory methods in transfusion medicine DI (FH) Adelheid Weidinger, BMA
Individual evidence
- ↑ a b c Adolf Faller, Michael Schünke: The human body . 15th edition. Georg Thieme Verlag, Stuttgart 2008, ISBN 978-3-13-329715-8 , p. 302 f .
- ↑ Standard work instructions. Serological tolerance (cross match)
- ↑ Michael Heck, Michael Fresenius: Repetitorium Anaesthesiologie: Preparation for the anesthesiological specialist examination and the European diploma for anesthesiology. Springer-Verlag, Heidelberg / Berlin / New York 2013, ISBN 3-6621-2917-5 , p. 764
- ↑ Coombs test immunohematological laboratory analysis. Institute for Clinical Transfusion Medicine and Hemotherapy. University Hospital Würzburg