Osteomyelofibrosis
| Classification according to ICD-10 | |
|---|---|
| D47.4 | Osteomyelofibrosis ICD-O 9961/3 |
| ICD-10 online (WHO version 2019) | |
The myelofibrosis ( OMF ), and primary myelofibrosis ( PMF ), chronic idiopathic myelofibrosis ( CIMF ), idiopathic myelofibrosis ( IMF ) or osteomyelosclerosis ( OMS ), belongs to the group of myeloproliferative neoplasms and provides a progressive malignant (malignant) diseases of the blood-forming bone marrow It is characterized by an increasing connective tissue remodeling ("fibrosis") of the bone marrow.
Other forms of bone marrow fibrosis, the "secondary" myelofibrosis, which arise as a result of another disease and are not necessarily malignant diseases , must be distinguished from OMF .
frequency
Osteomyelofibrosis is a rare condition that affects women more often. The peak of manifestation is between the ages of 50 and 60. The incidence is around 1.5: 100,000 / year or around 1200 cases per year in Germany.
causes
Possible causes for the OMF are:
- Primary OMF: “randomly” acquired genetic defects
- Secondary OMF:
- Reaction to the effects of chemical or physical noxae , e.g. B. ionizing rays
- Secondary disease due to another disease that changes the bone marrow, e.g. B. in polycythemia vera and in essential thrombocythemia
- other unknown causes
In the case of the secondary forms, too, it is partly assumed that these are caused by acquired genetic defects (all malignant diseases, i.e. tumor diseases are genetically determined diseases), but these genetic defects did not appear “sporadically”, but rather due to a clearly definable previous damage.
Word origin
The word osteomyelofibrosis is formed from the following components: os (ancient Greek ὀστέον ostéon , the "bone"), myelon (ancient Greek μύελος myelos ), the "marrow" and fibrous (neo-Latin fibrosus , "fiber-rich") with the suffix -ose (ancient Greek - ωσις, "-heit", "-keit"; in medicine as an ending for mostly non-inflammatory diseases and conditions).
Pathogenesis
| gene | approximate frequency |
|---|---|
| JAK2 | ~ 50% |
| Calreticulin ( CALR ) | ~ 25% |
| MPL | ~ 5% |
| Others (most common: ASXL1 , EZH2 , TET2 , IDH1 / IDH2 , SRSF2 , SF3B1 , U2AF1 ) and unknown |
together > 20% |
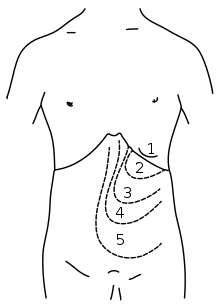
In OMF there is a progressive fibrosis (sclerosing) of the blood-forming bone marrow tissue . The blood formation is disturbed. Presumably, the changed blood cells and their precursors release substances that cause increased fiber formation in the bone marrow tissue. The formation of blood is therefore to a certain extent displaced from the bone marrow and increasingly takes place in the liver and spleen. The result is an enlarged spleen and possibly also a liver.
In the majority of patients, specific genetic defects were identified as the main cause of the disease. Most frequently (around 50%) there is a point mutation in the JAK2 gene ("Janus kinase 2"), which leads to an amino acid exchange V617F (exchange of the amino acid valine at position 617 for phenylalanine ). The second most common (about 25%) mutations in the gene CALR observed (calreticulin) and about 5% of cases, a mutation in MPL , the gene for thrombopoietin - receptor prior to (almost always is mutated here W515, that tryptophan at position 515). However, since these mutations are also found in other, related diseases (all in essential thrombocythemia, the JAK2 mutation in polycythemia vera), it is assumed that further mutations, which have not yet been very well characterized, will be added to the clinical phenotype of osteomyelofibrosis cause. These genetic defects are acquired , i.e. not inherited and also not inheritable, since the germ line cells are not affected (the genetic defects are only found in the cells of the blood-forming system).
Clinic / symptoms
At the beginning of the disease, the patients remain asymptomatic, the disease is only diagnosed after a long time. Symptoms can be:
- anemia
- Thrombocytopenia , possibly associated with a tendency to bleed
- Leukocytosis with left shift of the blood count (appearance of immature precursors of blood cells in the peripheral blood)
- increased leukocyte alkaline phosphatase
- Erythrocytes with " teardrop shape " (= dacryocytes, teardrop -poikilocytosis) in the blood smear
- Displacement symptoms in the abdomen with a large enlargement of the spleen: loss of appetite, irregular bowel movements, abdominal pain, diarrhea, feeling of tension
- Night sweats, weight loss, unexplained fever (so-called " B symptoms ")
- General symptoms: Feeling weak, poor performance, tiredness
Diagnosis
- History : fatigue and weight loss (see symptoms)
- Blood count shows leukocytosis and shift to the left (appearance of immature precursors of blood cells in the peripheral blood; see also erythrocyte distribution range )
- Clinical examination, as well as ultrasound examination of the spleen and liver, possibly computed tomography or MRI of the abdominal cavity
- Confirmation of the diagnosis by bone marrow puncture (KMP) with histological and cytological processing and differentiation from other myeloproliferative neoplasms. During bone marrow puncture, it is often impossible to aspirate liquid bone marrow due to the fibrosis ( punctio sicca , “dry puncture”).
- Bone marrow and blood tests for the presence of a JAK2 V617F mutation or calreticulin ( CALR ) and MPL mutations. These genetic tests should ideally be carried out from (EDTA) bone marrow aspirate. If this is not possible, (EDTA) blood can also be used.
Differential diagnoses
- other myeloproliferative diseases, particularly chronic myeloid leukemia (CML), should not be overlooked
- Myelodysplasias
- Bone marrow cancer
- toxic damage to the bone marrow
therapy
OMF is a chronic and demanding disease and should be treated by a haematologist. With OMF, a combination of symptomatic treatments to alleviate the symptoms, as well as medicinal and, if necessary, radiation therapy measures can be used:
- with pronounced leukocytosis: drug therapy with hydroxyurea ; Disadvantages: the leukocytosis can be reduced, but the rest of the blood formation (erythropoiesis, thrombopoiesis) is also dampened, which is undesirable; Treatment with hydroxyurea does not affect the course of the disease, it does not prevent the disease from progressing.
- in severe anemia: transfusion of red blood cell concentrates ("blood transfusion")
- with pronounced thrombocytopenia or bleeding tendency: transfusion of platelet concentrates
- In the case of pronounced splenomegaly with associated symptoms: either drug therapy or local spleen irradiation (results in a temporary reduction in size of the spleen, but the effect usually only lasts for a short time, rarely performed today)
- Interferon alpha: IFNa is a cytokine that must be administered subcutaneously and is effective in some cases of myelofibrosis; IFNa is not a cytostatic agent , but it still has some side effects that limit its uses.
- Ruxolitinib : A relatively specific drug for the treatment of OMF has been approved since 2012: ruxolitinib, a JAK2 tyrosine kinase inhibitor that is taken as a tablet. Ruxolitinib is administered to both patients with and without the JAK2 V617F mutation, since the JAK2 signal transduction pathway is also increased in the latter group of patients . The target dose is 2 × 20 mg daily. If the platelet count is low, start with a lower dose.
The only curative form of treatment is allogeneic blood stem cell or bone marrow transplantation . In many cases, however, this cannot be performed on OMF patients because they are too old and no longer physically “fit” enough for such a demanding treatment. The mortality of allogeneic transplants is significant and is around 20–30%.
forecast
Since the prognosis depends on many factors (primary or secondary disease, other diseases), there are no generalized results. The median survival after diagnosis is between 4 and 7 years, depending on the study, although long-term survivors up to 20 years have also been described. The most important causes of death are severe infections (due to the weak bone marrow) and the transformation into an aggressive form of acute leukemia.
Web links
- Expert group CMPE Information on idiopathic myelofibrosis / osteomyelofibrosis
- Internet pages of the German Leukemia & Lymphoma Aid (DLH)
- New guidelines of the DGHO (German Society for Hematology and Oncology)
- Information about myelofibrosis On the MPN Self Help Forum website
See also
Individual evidence
- ↑ In the WHO classification of hematological diseases, which is the standard internationally, the term "primary myelofibrosis" is used.
- ↑ Duden: Medical terms, page 524, entry "Myelon"
- ↑ Duden: Large Foreign Dictionary, page 456, entry "fibrous"
- ↑ Martin Grießhammer, Gabriela M. Baerlocher, Heinz Gisslinger, Eva Lengfelder, Petro E. Petrides: Primary Myelofibrosis (PMF). DGHO, accessed September 17, 2016 .