Allostatic load
The allostatic load refers to the effects of overuse and wear and tear that occur in an organism after repeated or chronic exposure to stress . The term was coined by McEwen and Stellar in 1993 . It depicts the physiological consequences of chronic exposure to a fluctuating or increasing neurogenic or neuroendocrine fight-or-flight response .
Regulation model
The term allostatic load expresses so-called "wear and tear" reactions that occur as a result of chronic or repeated exposure to stress . It was first coined by McEwen and Stellar in 1993 .
The theory is derived from the regulation model of allostasis , which describes a predictive regulation or stabilization of internal processes and sensations depending on stimuli , usually regulated by the brain . It is a generalization of the concept of homeostasis . "Predictive regulation" here stands for the ability of the CNS to foresee situations of need and to react to them before they arise.
An essential aspect of an efficient regulation is the reduction of uncertainty (and thus of entropy in the sense of message theory ). Due to the uncertainty that occurs through the feeling of inevitable surprise, the organism is constantly looking for ways to reduce the uncertainty of future developments. Allostatic mechanisms help by predicting needs and by predictive compensation. However, this predictive regulation leads to a considerable consumption of energy, so that the situation, especially if the uncertainty cannot be eliminated, can end in a chronic accumulation of allostatic load.
The concept of allostatic load postulates that neuroendocrine, cardiovascular , neuroenergetic and emotional responses remain constantly activated, so that turbulence in the blood flow in the coronary arteries and the arteries supplying the brain, high blood pressure, atherogenesis , cognitive dysfunction and depression accelerate the progression of the disease. In this way, an allostatic load can lead to permanent changes in the brain architecture and other systemic pathophysiological effects.
Ultimately, the allostatic load can even reduce the organism's ability to cope with future uncertainty.
Types of allostatic load
McEwen and Wingfield have proposed two types of allostatic load, which have different causes and consequences:
A Type 1 allostatic load arises from an adaptive response when energy consumption exceeds available energy. This leads to an emergency reaction ("emergency life history stage"). This ensures survival, leads to a positive energy balance and subsequently reduces the allostatic load again. Typical situations that lead to a type 1 allostatic reaction are hunger , hibernation and critical illness. Severe general illnesses can be both the cause and the consequence of the allostatic (overload) load.
An allostatic load of type 2 occurs when the energy supply is sufficient but is associated with social conflicts or other forms of social dysfunction (i.e. the expected energy consumption is high). This can be in human society as well as in animals, e.g. B. in captivity, the case. In all cases, the secretion of glucocorticoids and other allostasis mediators such as the activity of the autonomic nervous system flood in and out with the allostatic load. Diseases result from chronically increased allostatic loads or from allostatic overloads .
While both types of allostatic load are associated with increased secretion of cortisol and catecholamines , thyroid homeostasis reacts differently: The concentration of the thyroid hormone T3 is reduced in type 1 allostasis ( low T3 syndrome ), but increased in type 2 Allostasis ( high T3 syndrome ).
Measurement
The allostatic load is usually determined by index variables in the sense of sum scores, which include indicators for cumulative stress in various organs and tissues as well as primary biomarkers for neuroendocrine, cardiovascular, immunological and metabolic organ systems.
The indices used are heterogeneous, so that different studies usually use different methods based on different biomarkers and calculation methods. On the other hand, the allostatic load is not specific to humans , but can also be used, for example, to evaluate chronic stress effects in non-human primates .
In the endocrine system, high levels of stress lead to an increased release of the corticotropin-releasing factor or corticotropin-releasing hormone ( CRH ), which increases the target value of the HPA axis , the central stress response system. Persistent stress can lead to decreased cortisol concentrations in the morning and increased concentrations in the afternoon and evening, which is associated, among other things, with an overall increased cortisol release and consecutively increased blood sugar levels as well as decreased bone density .
In the nervous system , chronic stress can lead to structural and functional changes and abnormalities. The dendrites of neurons shorten during stress . This is seen as the reason for a reduced alertness with allostatic load. In addition, chronic stress can lead to an increased fear response to news.
Despite the increased cortisol concentration, chronic stress in the immune system leads to increased inflammation . The cause is an increased activation of the sympathoadrenergic system .
The reactions mentioned can be quantitatively recorded as primary stress mediators together with secondary biomarkers of the allostatic reaction and summarized in a total score for the allostatic load.
Relationship to allostasis and homeostasis
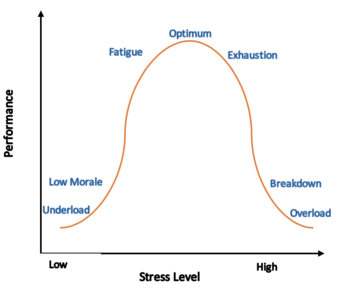
Stress is the main contributing factor to the allostatic load. Basically, allostasis is a mechanism that expands the possibilities of homeostasis. Homeostatic systems regulate the state in the body and the external environment with a constant set point . The difference between pure homeostasis and allostasis lies in the concept of prediction. The latter can stimulate the release of mediators such as cortisol, TSH , prolactin, etc. Excessive mediator concentrations can lead to allostatic burden and fear.
Three physiological processes can increase the allostatic load:
- Frequent stress: The level and frequency of the stress response determines the level of the allostatic load.
- Failure to "switch off": The body's inability to relax while stress mediators are at high levels, such as increasing blood pressure.
- Inadequate answer: the body's inability to respond to stresses such as inflammation from glucocorticoids .
A lack of coordination between homeostatic and allostatic mechanisms can ultimately lead to allostatic overload via an allostatic load , which causes illnesses through decompensation. This can also be quantified by indicators of the allostatic load.
The DOREMI R package is available for statistical purposes, with which the dynamics of a homeostatic system can be modeled under the influence of external influences.
Risk reduction
By taking structural and psychological factors into account, the allostatic load can be reduced and controlled individually. These include, for example, the social environment and access to health services. Behavioral factors include lebensstilmodifizierende measures such as diet , exercise and tobacco waiving one. Early intervention can therefore prevent the development of chronic diseases.
A low socio-economic status increases the allostatic burden, so that measures to reduce social polarization and to improve social contacts and psychological boundary conditions can reduce the allostatic burden at the population level.
Interventions can also consist of educational measures for improved sleep quality and quantity, a healthy lifestyle and other social support.
The relationship between stress and allostatic load differs according to the sex, age and social status of the person concerned, so that personalized measures are useful, which should also include educational measures and the design of workplaces.
See also
Web links
- Bruce McEwen lecture on the concept of the allostatic load
- Brief explanation of the concept in German
Individual evidence
- ↑ Jane Ogden: Health Psychology: A textbook, 3rd edition . Open University Press - McGraw-Hill Education, 2004, ISBN 978-0-335-21471-6 , p. 259.
- ^ BS McEwen, E. Stellar: Stress and the individual. Mechanisms leading to disease. . In: Archives of Internal Medicine . 153, No. 18, September 27, 1993, pp. 2093-101. doi : 10.1001 / archinte.153.18.2093 . PMID 8379800 .
- ↑ a b P. Sterling: Allostasis: a model of predictive regulation. . In: Physiology & Behavior . 106, No. 1, April 12, 2012, pp. 5-15. doi : 10.1016 / j.physbeh.2011.06.004 . PMID 21684297 .
- ↑ a b c d H.M. Schenk, BF Jeronimus, L. van der Krieke, EH Bos, P. de Jonge, JG Rosmalen: Associations of Positive Affect and Negative Affect With Allostatic Load: A Lifelines Cohort Study . In: Psychosomatic Medicine . 80, No. 2, 2017, pp. 160–166. doi : 10.1097 / PSY.0000000000000546 .
- ↑ a b c d A. Danese, BS McEwen: Adverse childhood experiences, allostasis, allostatic load, and age-related disease. . In: Physiology & Behavior . 106, No. 1, April 12, 2012, pp. 29-39. doi : 10.1016 / j.physbeh.2011.08.019 . PMID 21888923 .
- ↑ a b c d e A. Peters, BS McEwen, K. Friston: Uncertainty and stress: Why it causes diseases and how it is mastered by the brain. . In: Progress in Neurobiology . 156, September 2017, pp. 164-188. doi : 10.1016 / j.pneurobio.2017.05.004 . PMID 28576664 .
- ^ AL Brame, M Singer: Stressing the obvious? An allostatic look at critical illness. . In: Critical care medicine . 38, No. 10 Suppl, October 2010, pp. S600-7. doi : 10.1097 / CCM.0b013e3181f23e92 . PMID 21164403 .
- ↑ JM Cuesta, M Singer: The stress response and critical illness: a review. . In: Critical care medicine . 40, No. 12, December 2012, pp. 3283-9. doi : 10.1097 / CCM.0b013e31826567eb . PMID 22975887 .
- ↑ a b A Chatzitomaris, R Hoermann, JE Midgley, S Hering, A Urban, B Dietrich, A Abood, HH Klein, JW Dietrich: Thyroid Allostasis-Adaptive Responses of Thyrotropic Feedback Control to Conditions of Strain, Stress, and Developmental Programming. . In: Frontiers in endocrinology . 8, 2017, p. 163. doi : 10.3389 / fendo.2017.00163 . PMID 28775711 .
- ^ BS McEwen, JC Wingfield: The concept of allostasis in biology and biomedicine. . In: Hormones and behavior . 43, No. 1, January 2003, pp. 2-15. PMID 12614627 .
- ^ A b Ashley Edes, Douglas Crews: Allostatic load and biological anthropology . In: American Journal of Physical Anthropology . 162, January 1, 2017, pp. 44–70. doi : 10.1002 / ajpa.23146 . PMID 28105719 .
- ↑ a b c BS McEwen: Stress, adaptation, and disease. Allostasis and allostatic load. . In: Annals of the New York Academy of Sciences . 840, May 1, 1998, pp. 33-44. doi : 10.1111 / j.1749-6632.1998.tb09546.x . PMID 9629234 .
- ^ McEwen BS: Allostasis and allostatic load: implications for neuropsychopharmacology . In: Neuropsychopharmacology . 22, No. 2, 2000, pp. 108-24. doi : 10.1016 / S0893-133X (99) 00129-3 . PMID 10649824 .
- ↑ DOREMI cran.r-project.org
- ↑ M Kristenson, HR Eriksen, JK Sluiter, D Starke, H Ursin: Psychobiological mechanisms of socioeconomic differences in health . In: Social Science & Medicine . 58, No. 8, April 2004, ISSN 0277-9536 , pp. 1511-1522. doi : 10.1016 / s0277-9536 (03) 00353-8 . PMID 14759694 .
- ^ A b Robert-Paul Juster, Bruce S. McEwen, Sonia J. Lupien: Allostatic load biomarkers of chronic stress and impact on health and cognition . In: Neuroscience & Biobehavioral Reviews . 35, No. 1, September 2010, ISSN 0149-7634 , pp. 2-16. doi : 10.1016 / j.neubiorev.2009.10.002 . PMID 19822172 .