Iron deficiency anemia
| Classification according to ICD-10 | |
|---|---|
| D50.- | Iron deficiency anemia |
| D50.0 | Iron deficiency anemia after blood loss (chronic)
Posthemorrhagic anemia (chronic) |
| D50.1 | Sideropenic dysphagia
|
| D50.8 | Other iron deficiency anemia |
| D50.9 | Iron deficiency anemia, unspecified |
| ICD-10 online (WHO version 2019) | |
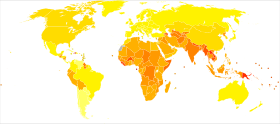
The iron deficiency anemia (previously in relation to the symptoms as chlorosis or anemia called) is a by iron deficiency caused and worldwide the most common form of anemia and probably the most common deficiency disease at all. Its prevalence is estimated at around 600 million people worldwide. The iron deficiency disrupts the production of the red blood pigment, hemoglobin . People with iron deficiency anemia often feel tired and limp, and have a pale complexion.
Most common causes
The most common causes of iron deficiency anemia are malnutrition and bleeding . However, iron deficiency can also arise from an increased requirement during growth or as part of an absorption disorder in the small intestine. In addition to insufficient intake of nutrients such as vitamin C , the intake of iron absorption inhibitors are often the cause of anemia. The list of inhibitors includes phytates (e.g. in bran, peanuts, legumes), dairy products, eggs and coffee.
Laboratory values and diagnosis
| modification | parameter |
|---|---|
| humiliated | Hemoglobin, Ferritin Transferrin Saturation , MCV, MCHC |
| elevated | Transferrin, RDW, zinc protoporphyrin |
Iron deficiency anemia is a microcytic hypochromic anemia. H. Hemoglobin is decreased (about Hb <13.5 g / dl in men and <12.0 g / dl in women; the normal values vary slightly depending on the source) and the erythrocytes (red blood cells) are smaller and contain less hemoglobin than normal. In laboratory terms, this is expressed by the parameters MCV ( mean individual erythrocyte volume ) and MCHC ( mean corpuscular hemoglobin concentration ), both of which are then reduced. However, if there is also a vitamin B12 or folic acid deficiency (often e.g. with high alcohol consumption ), MCV and MCHC may be normal. Another indication of iron deficiency anemia is a significantly increased variation in the size of the red blood cells (RDW) in the blood count ( anisocytosis ). Iron in the serum is subject to strong nutrition-dependent fluctuations and is therefore unsuitable as the sole parameter for confirming a diagnosis. However, the iron value can usually be used to tell whether a patient actually took the iron tablets prescribed - in high doses that are sometimes poorly tolerated - on the day before the blood sample was taken. A low ferritin value, on the other hand, always indicates an iron deficiency. A normal or even increased value does not exclude it, however, since ferritin, as an acute phase protein , can be released to a greater extent in the course of an inflammatory reaction. The transferrin saturation , which is calculated from the transferrin level and the iron level and which is lowered in the case of iron deficiency, is more reliable . Anemia without iron deficiency points to other causes such as a deficiency in vitamin B6 , B12 or folic acid or an erythropoietin deficiency ( renal anemia ), which are necessary for blood formation (see anemia ). Thalassemia , which is rare in Central Europeans , should also be considered, especially in people from the Mediterranean and Southeast Asia .
Symptoms
The following symptoms are considered typical:
- Initial stage:
- Loss of performance and physical weakness
- fatigue
- a headache
- Nails: brittleness, grooving, koilonychia
- Angular cheilitis (ICD Code: K13.0)
- Progressive clinical picture:
- impaired heart functions
- Difficulty concentrating
- Feeling dizzy ( vertigo )
- Balance disorder
- Faint
treatment
Basically, iron deficiency anemia is treated like iron deficiency in general and there are two main treatment modalities 1. Change in diet, 2. Drug iron therapy (either orally or intravenously).
In addition to the treatment options mentioned above, there is a specific option for treating iron deficiency anemia, namely the administration of blood transfusions (to be precise, red cell concentrates ). If a severe, u. If life-threatening anemia is present, blood transfusions must be administered in order to bring about a rapid change in this condition. In principle, however, the iron deficiency should be compensated for and blood transfusions should be administered as little as necessary. A consistent and timely compensation of an iron deficiency can "save" blood transfusions. Frequently repeated blood transfusions (from about 20–50) lead to an increased iron intake and the risk of iron overload, as the body can only excrete the iron to a limited extent. This can cause organ damage. Iron overload can be counteracted by iron chelators. These bind the iron in the body and carry it away.
Individual evidence
- ↑ From the 16th to the 19th century, “chlorosis” was also an independent clinical picture that was not necessarily related to iron deficiency anemia; see. e.g. I. Loudon: The Diseases Called Chlorosis. In: Psychol. Med. Volume 14, 1984, pp. 27-36.
- ↑ Horst Kremling : On the development of clinical diagnostics. In: Würzburger medical history reports 23, 2004, pp. 233–261; here: p. 249.
- ↑ In the case of inflammation, ferritin can also be “false-normal”
- ↑ Mortality according to WHO estimates in 2002. (xls; 3.0 MB) In: World Health Organization. 2002, accessed December 23, 2010 .
- ↑ Lothar Thomas u. a .: New parameters for the diagnosis of iron deficiency states: Conclusion. (PDF, 35 kB) In: Dtsch Arztebl 2005; 102 (42), pp. A-2878. German Medical Association, August 25, 2009, accessed on August 11, 2010 : "The serum iron value (is) obsolete for the diagnosis of iron deficiency anemia"
- ^ A. Nilsson, M. Foerster: Symptoms and risks of anemia. 2013.
- ^ E. Litton, J. Xiao, KM Ho: Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomized clinical trials. In: BMJ. 347, 2013, pp. F4822 – f4822, doi: 10.1136 / bmj.f4822 .