Lentigo maligna
As lentigo maligna (synonyms: melanoma in situ , melanotic precancer , Melanosis circumscripta praeblastomatosa Dubreuilh , Crohn Dubreuilh or Dubreuilh disease) is an intraepidermal (in the epidermis preferred) neoplastic proliferation of atypical melanocytes , respectively. Lentigo maligna typically occurs after the age of 50; men are affected about twice as often as women.
Emergence
Long-term UV exposure is suspected to be the originating mechanism; areas regularly exposed to light such as the head, neck, forearms or lower legs are particularly affected, but it can occur in all parts of the body. Damage to the DNA of the melanocytes is suspected , which leads to a malignant cell clone in the epidermis. Such a malignant degeneration is called a melanoma in situ , and tumor growth can result in a lentigo maligna melanoma.
Clinic / diagnosis
The lentigo maligna precedes the lentigo maligna, which has developed over the years gray-brown to black pigmented foci with blurred borders and different sizes. It is important to distinguish it from senile lentigo . In addition to the clinical assessment, the histopathological confirmation of the diagnosis is required. In addition to lentigo senilis, lentigo simplex , seborrheic keratosis and superficial spreading melanoma (SSM) are possible differential diagnoses .
pathology
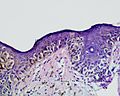
There is a mostly broad-based proliferation of atypical melanocytes , which are irregularly distributed individually or lined up in a chain-like manner along the dermoepidermal border (border between epidermis and dermis ), whereby they can appear to be arranged like palisades perpendicular to the skin surface. Occasionally, atypical melanocytes rise within the epidermis (upper skin) in its upper cell layers. A spread along follicular structures and ducts of the sweat glands can typically be observed. In long-standing lesions, melanocytic nests or multinucleated giant cells also predominantly form along the dermoepidermal border.
The cell nuclei of the melanocytes are hyperchromatic (excessively colored), irregularly contoured and pleomorphic (variable in shape and size). The cytoplasm often appears to be very wide or vacuolated due to a retraction artifact, often showing strong pigmentation of the neighboring keratinocytes (cells of the epidermis) down to the horny layer due to a high melanin content . Amelanotic (non-pigmented) lesions are rare.
Signs of UV damage are atrophy (narrowing) of the corresponding epidermis and solar elastosis (UV-related degeneration of the elastic fibers) of the underlying dermis (dermis). The latter also often shows an increase in small blood vessels and an inflammatory cell infiltrate from lymphocytes and melanophages.
therapy
Therapy usually consists of excision in toto, a complete surgical removal with a lateral safety margin. In the case of very numerous and / or poorly located foci, laser treatment or X-ray irradiation with a maximum of 100 Gy radiation dose can be carried out. If there has already been a degeneration into a lentigo maligna melanoma, X-ray irradiation may no longer be carried out.
forecast
With timely, adequate treatment (excision in healthy tissue), the chances of recovery are almost 100%. If a lentigo maligna melanoma has already developed, the prognosis in stage I is> 90%.
literature
- W. Kempf, M. Hantschke, H. Kutzner, W. Burgdorf: Dermatopathology. Steinkopff, Darmstadt 2007, ISBN 978-3-7985-1647-2 .
- Eggert Stockfleth: skin cancer. A practical Guide. UNI-MED-Verlag, Bremen et al. 2007, ISBN 978-3-89599-207-0 ( UNI-MED Science ).
- Ingrid Moll: Dermatology. 6th completely revised and expanded edition. Thieme, Stuttgart 2005, ISBN 3-13-126686-4 ( dual series ).
Individual evidence
- ^ WH Clark, MC Mihm: Lentigo maligna and lentigo-maligna melanoma . In: The American Journal of Pathology . tape 55 , no. 1 , April 1969, ISSN 0002-9440 , pp. 39-67 , PMID 5776171 , PMC 2013384 (free full text).
- ↑ Farah Rukhsana Abdulla, Mary Jo Kerns, Diya F. Mutasim: Amelanotic lentigo maligna: a report of three cases and review of the literature . In: Journal of the American Academy of Dermatology . tape 62 , no. 5 , May 2010, ISSN 1097-6787 , p. 857-860 , doi : 10.1016 / j.jaad.2009.06.017 , PMID 19766347 .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. [Edinburgh, Scotland?], ISBN 978-0-7020-7552-0 , pp. 1315 f .