Medulloblastoma
| Classification according to ICD-10 | |
|---|---|
| C71 | Malignant neoplasm of the brain |
| C71.6 | cerebellum |
| ICD-10 online (WHO version 2019) | |
The medulloblastoma is a malignant embryonic tumor of the cerebellum . It occurs preferentially in toddlers and children and is the most common malignant brain tumor in this age group. It is classified as grade IV according to the WHO classification of tumors of the central nervous system .
Epidemiology
Boys are more often affected than girls; the age peak is between 1-9 years or 4-8 years, depending on the literature. However, around one fifth of medulloblastomas also occur after puberty, with an age peak in the third decade of life.
Symptoms
Medulloblastomas infiltrate both cerebellar hemispheres and can also metastasize into the liquor space ("drip metastases"). Clinically, disorders of the cerebellar function (e.g. tendency to fall and ataxia ) as well as signs of increased intracranial pressure with headache , lethargy and morning vomiting are in the foreground. The increased intracranial pressure arises on the one hand from the tumor tissue-related increase in intracranial volume itself, on the other hand from the rapidly developing occlusive hydrocephalus. If the fundus is reflected, a congestive papilla can be recognized as a sign of increased intracranial pressure. The entrapment of parts of the cerebellum and compression of the medulla oblongata (which in turn is the seat of the vital respiratory and circulatory center) often caused the death of the young patients.
Imaging
In computed tomography and magnetic resonance tomography (MRT), medulloblastomas appear as solid masses with inhomogeneous contrast medium uptake. They usually grow from the floor of the 4th ventricle into the cerebellar worm. The tumor is slightly hypodense on native CT and hyperdense after contrast administration. Due to its inhomogeneous, symmetrical position in the cranio-caudal extent with a hypointense signal in T1 and a hyperintense signal in T2 (because it is more watery), the tumor can be clearly identified on MRI. Often there is obstruction of the ventricles; as a result, hydrocephalus occurs. In very young patients, this can be shown by widened calotte sutures (cloud skulls), which diverge as a consequence of increasing intracranial pressure.
pathology
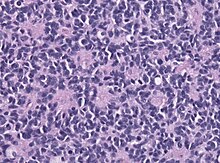
The medulloblastoma is an undifferentiated embryonic tumor derived from embryonic pluripotent cells. Fine tissue, medulloblastomas are cell-dense, small, round and blue-cell tumors. The tumor cells have round to oval nuclei and can be arranged in rosette formations. Immunohistochemically, expression of neuronal markers ( synaptophysin , neurofilament , NeuN) is typical, but glial proteins such as GFAP can also be expressed in small areas. Different variants are desmoplastic medulloblastoma, anaplastic medulloblastoma and medulloblastoma with extensive nodularity.
genetics
The first detection of a p53 mutation in a medulloblastoma came in the early 1990s. Medulloblastomas are currently divided into the following four subgroups based on their genetic profile:
- WNT : mostly children, rarely adults: monosomy chromosome 6, CTNNB1 mutations , mostly classic medulloblastomas, rarely large-cell / anaplastic medulloblastomas. This group has the best prognosis.
- SHH ( Sonic hedgehog ): Small children (mostly desmoplastic / nodular) and adults (classic or large cell / anaplastic): PTCH / SMO / SUFU mutations, GLI2 amplifications .
- Group 3 : mostly children, classic medulloblastomas, often metastasizing, MYC amplification, chromosomal losses on 5q and 10q. This group has the worst prognosis.
- Group 4 : mostly children, more often male, often isochromosome 17q. Chromosomal losses on 8 and X.
therapy
Current treatment concepts for children and adolescents with a medulloblastoma include neurosurgical tumor removal, chemotherapy and radiation therapy . Instead of conventional radiation therapy, proton therapy can also be used, which has an even more targeted and gentle effect and is therefore becoming increasingly important in the treatment of tumors in children and adolescents. Whenever possible, a complete tumor resection should always be sought. Often this is only possible to a limited extent due to the location or the infiltration of vital structures, so that only partial resection is possible. However, this can also be used to restore the CSF passage.
forecast
The course of the disease depends, among other things, on the size of the tumor, the extent to which the tumor has been removed, any colonization of tumor cells along the CSF pathway and the age of the patient. The type of tissue differentiation can also play a prognostic role, although the course of the disease is more favorable in patients with a so-called desmoplastic medulloblastoma.
In clinical trials, patients are divided into low, standard, and high risk groups:
- In patients in the low-risk group (usually WNT-activated), cure rates of up to 100% are achieved, depending on the study. The current efforts are therefore moving in the direction of reducing the intensity of the therapy and thus the negative long-term consequences, while at the same time confirming the high healing rates.
- In the HIT-SIOP PNET 4 study, in which 340 children and adolescents from the standard risk group aged four to 21 years from several European countries took part, the 5-year survival rate was between 85% and 87%, depending on randomization . Around 78% of the patients did not relapse for 5 years and are therefore considered cured. After a relapse, the prognosis was very poor. Five years after a relapse, only four of 66 patients were alive despite intensive treatment.
- A US study enrolled 161 patients between the ages of three and 21 years with a high-risk profile . Depending on the randomization, half of the patients also received carboplatin daily during the irradiation . The 5-year survival rate for patients with carboplatin was 82% and for those without 68%. The European SIOP PNET 5 study is currently taking place until April 2024, attempting to confirm the promising results with carboplatin during irradiation in the standard risk group.
In the case of newborns and toddlers under three years of age, due to the enormous side effects, radiation is usually avoided or postponed with the help of chemotherapy until the patient reaches the age of four. In a clinical study in which 62 patients participated, the 5-year survival rate was 66% in children who had only received intensive chemotherapy after diagnosis. After complete removal of the tumor, a 5-year survival rate of 93% was achieved. After incomplete removal of the tumor or colonization of tumor cells along the CSF pathways, the 5-year survival rates were 56% and 38%, respectively.
literature
- DD Louis, H. Ohgaki, O. Wiestler et al. (Eds.): World Health Organization classification of tumors. Pathology and genetics of tumors of the nervous system. IARC Press, Lyon 2007, ISBN 978-92-832-2430-3 .
- S1 guideline medulloblastoma in children and adolescents of the German Society for Child and Adolescent Medicine (DGKJ). In: AWMF online (as of 2008)
Web links
Individual evidence
- ↑ H. Ohgaki, RH Eibl, OD Wiestler, MG Yasargil, EW Newcomb, P. Kleihues: p53 mutations in brain tumors nonastrocytic human. In: Cancer Research. 1991 Nov 15; 51 (22), pp. 6202-6205. PMID 1933879 full text
- ↑ MD Taylor, PA Northcott, A. Korshunov, M. Remke, YJ Cho, SC Clifford, CG Eberhart, DW Parsons, S. Rutkowski, A. Gajjar, DW Ellison, P. Lichter, RJ Gilbertson, SL Pomeroy, M. Kool, SM Pfister: Molecular subgroups of medulloblastoma: the current consensus. In: Acta neuropathologica. Volume 123, Number 4, April 2012, pp. 465-472, ISSN 1432-0533 . doi: 10.1007 / s00401-011-0922-z . PMID 22134537 . PMC 3306779 (free full text).
- ↑ Proton therapy for brain tumors at the WPE | WPE-UK.de. In: West German Proton Therapy Center Essen (WPE). Retrieved on August 5, 2019 (German).
- ↑ Medulloblastoma (brief information). Retrieved August 5, 2019 .
- ↑ B. Timmermann: Radiation therapy for cancer in childhood. In: https://www.kinderkrebsstiftung.de . German Children's Cancer Foundation, August 29, 2018, accessed on August 5, 2019 (German).
- ^ Identifying Low-Risk Medulloblastoma to De-escalate Therapy. Retrieved December 29, 2019 .
- ↑ International Society of Pediatric Oncology (SIOP) PNET 5 Medulloblastoma - Full Text View - ClinicalTrials.gov. Retrieved December 29, 2019 .
- ↑ Birgitta Lannering, Stefan Rutkowski, Francois Doz, Barry Pizer, Göran Gustafsson: Hyperfractionated Versus Conventional Radiotherapy Followed by Chemotherapy in Standard-Risk Medulloblastoma: Results From the Randomized Multicenter HIT-SIOP PNET 4 Trial . In: Journal of Clinical Oncology . tape 30 , no. 26 , July 30, 2012, ISSN 0732-183X , p. 3187-3193 , doi : 10.1200 / JCO.2011.39.8719 ( ascopubs.org [accessed December 29, 2019]).
- ↑ Magnus Sabel, Gudrun Fleischhack, Stephan Tippelt, Göran Gustafsson, François Doz: Relapse patterns and outcome after relapse in standard risk medulloblastoma: a report from the HIT-SIOP-PNET4 study . In: Journal of Neuro-Oncology . tape 129 , no. 3 , September 2016, ISSN 1573-7373 , p. 515-524 , doi : 10.1007 / s11060-016-2202-1 , PMID 27423645 , PMC 5020107 (free full text).
- ↑ Regina I. Jakacki, Peter C. Burger, Tianni Zhou, Emiko J. Holmes, Mehmet Kocak: Outcome of Children With Metastatic Medulloblastoma Treated With Carboplatin During Craniospinal Radiotherapy: A Children's Oncology Group Phase I / II Study . In: Journal of Clinical Oncology . tape 30 , no. 21 , July 20, 2012, ISSN 0732-183X , p. 2648–2653 , doi : 10.1200 / JCO.2011.40.2792 , PMID 22665539 , PMC 4559602 (free full text).
- ↑ International Society of Pediatric Oncology (SIOP) PNET 5 Medulloblastoma - Full Text View - ClinicalTrials.gov. Retrieved December 29, 2019 .
- ↑ Rutkowski et al .: Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. In: N Engl J Med. 2005; 352, pp. 978-86. PMID 15758008 full text

