Rapidly progressive glomerulonephritis
| Classification according to ICD-10 | |
|---|---|
| N01.- | Rapid progressive nephritic syndrome |
| ICD-10 online (WHO version 2019) | |
When rapidly progressive glomerulonephritis ( Engl. Rapidly progressive glomerulonephritis , shortly RPGN ) is it is an intermittently occurring extracapillary glomerulonephritis associated with a rapid loss of renal function associated. If left untreated, kidney failure can occur within weeks to months . Further synonyms for this disease are rapidly progressive glomerulonephritis and crescentic glomerulonephritis (German crescent-shaped glomerulonephritis ), as well as necrotizing intra- / extracapillary-proliferating glomerulonephritis with crescent formation.
Epidemiology
Incidence: <1 / 100,000 / year
pathology
Pathogenesis
It is in the RPGN an immune complex glomerulonephritis or Antibasalmembran -Glomerulonephritis. RPGN can occur for no apparent reason (idiopathic) or more frequently in systemic diseases such as granulomatosis with polyangiitis , Goodpasture's syndrome or microscopic polyangiitis .
Macroscopically
The kidneys may be slightly enlarged and show some punctiform bleeding.
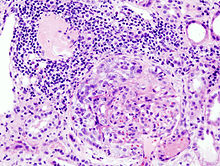
Microscopic
The histological picture is colorful because the disease progresses in stages. The pronounced crescent formation in the glomeruli is typical . Individual monocytes can also be found. The area around the glomerulus is usually infiltrated by inflammation . In the electron microscope image, the loops of the gomerulus are ruptured and the capsular space of the glomerulus is filled with fibrin . A certain staining method, immunofluorescence , can be used to detect the attachment patterns of the immunoglobulins . This is used to distinguish the different forms of RPGN (see below).
The ANCA-associated rapidly progressive glomerulonephritis is classified according to the proportion of glomeruli with inflammatory crescent moons and the proportion of scarred glomeruli (global sclerosis):
| class | Inclusion criteria |
|---|---|
| Focal | ≥ 50% normal glomeruli |
| Crescent formation | ≥ 50% glomeruli with cellular crescent moons |
| Mixed | <50% normal, <50% sclerotic <50% glomeruli with crescent moons |
| Sclerotic | ≥ 50% completely scarred glomeruli |
This classification allows an estimation of the prognosis: Patients with focal ANCA-associated glomerulonephritis have the best prognosis. Patients with predominantly crescent formation have a highly acute early stage of the disease, but the chance that the disease will respond to immunosuppressive therapy is relatively good. The prognosis of the mixed form is worse. Patients with a high percentage of scarred glomeruli are already at an advanced stage of the disease and the chance that this will respond to treatment is low.
Classification
A distinction is made between three forms of RPGN:
- Antibasalmembran-RPGN (10-20%), detection of antibodies to glomerular basement membrane serum, histological evidence of immunoglobulins type G and C 3 - complement in linear arrangement to the basement membrane.
- without lung involvement, very rarely
- with lung involvement = Goodpasture syndrome , often men before the age of 40
- Immune complex RPGN (30-40%), accumulation of immune complexes in heaps (so-called "humps"), e.g. B. in lupus erythematosus
- ANCA -associated vasculitis (40-50%), e.g. B. as a renal form of granulomatosis with polyangiitis
- Mixed type of 1 and 3
clinic
- Rapid onset, hypertension,
- Renal failure to dialysis within weeks sonographically not enlarged kidneys,
- Proteinuria with possible nephrotic syndrome ,
- Pulmonary bleeding in Goodpasture syndrome
diagnosis
The clinic and rapidly increasing retention values, immunological diagnostics (see above). Kidney biopsy with the following histology can confirm the diagnosis. The differential diagnoses are acute kidney failure (anamnesis of the triggering event) and acute abacterial nephritis, in which case the medication intake should be inquired about.
The exact determination of anticytoplasmic antibodies against neutrophil granulocytes (ANCA) with the corresponding distribution patterns enables the cause of the RPGN to be differentiated. In granulomatosis with polyangiitis, c-ANCA are found. With the p-ANCA type, microscopic polyangiitis should be considered.
therapy
According to the immunopathogenesis, the therapy consists of high-dose immunosuppression with steroids in combination with cyclophosphamide . Goodpasture's syndrome is treated in combination with plasma separation .
The renal insufficiency that occurs must be treated with dialysis .
Course and prognosis
The course and prognosis depend on the start of therapy. The presence of renal insufficiency requiring dialysis or fibrosis of the interstitium are prognostically unfavorable.
In Goodpasture's syndrome (antibodies against the basement membranes of the lung alveoli and glomeruli), pulmonary and renal symptoms can occur together, but also separately. Pulmonary infiltrates, coughing up blood, microcytic anemia and progressive kidney failure occur.
If left untreated, Goodpasture syndrome leads to death within a few days. With early diagnosis and therapy, the prognosis has improved significantly.
Complications
Development of terminal renal insufficiency with pulmonary edema, hypertension, hyperkalaemia, possibly pulmonary bleeding.
literature
- Riede, Schäfer: Pathology . ISBN 3-13-683303-1
- Herold: Internal Medicine . 2016 (epidemiology)
- Internal Medicine Dual Series, 2012
Web links
- Rapidly progressive glomerulonephritis pathology - Pathopic image database of the University of Basel - PathoPic instructions (PDF; 2.2 MB)
Individual evidence
- ^ Herbert Renz-Polster, Steffen Krautzig, Jörg Braun: Basic textbook internal medicine , 4th edition, Urban & Fischer / Elsevier, March 7, 2008, ISBN 3-437-41053-9 .
- ↑ Annelies E Berden et al .: Histopathologic classification of ANCA-associated glomerulonephritis . In: Journal of the American Society of Nephrology . 21, No. 10, October 2010, ISSN 1533-3450 , pp. 1628-1636. doi : 10.1681 / ASN.2010050477 . PMID 20616173 .