Spirometry
The spirometry , today with or as spirography , is a medical procedure for measuring and recording of the lungs - or tidal volume and the air flow rates for the assessment of lung function . Spirometry is the most commonly used procedure in pulmonology .
The entire lung volume and individual parts as well as its changes in the course of the breathing cycle can be determined. These so-called ventilation sizes can be e.g. B. measured using a spirometer .
Spirometry is divided into resting spirometry and occupational spirometry (spiroergometry).
history
→ See history of spiroergometry
Structure and functionality
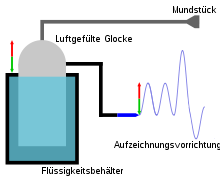
Described as a model, the person whose respiratory volumes are to be determined breathes in and out of a closed container via a mouthpiece-hose system. This container is freely movable in height because it is in a liquid such. B. Water floats. The spirometry container is connected to a recorder via a system of pulleys, which graphically records the change in altitude in the form of a spirogram . In order not to breathe back too much carbon dioxide after expiration and thus to prevent hypercapnia , an absorber container (e.g. soda lime container) is usually placed in the hose system.
The breathing process now changes the volume in the spirometry container. During expiration (exhalation), volume is pressed from the lungs into the container. Since air is lighter than water, the container rises. The recorder needle is lowered by means of the deflection via the roller system and there is a negative deflection on the ordinate . The lungs now lack the expiratory volume.
Conversely, air is withdrawn from the spirometry container during inspiration (inhalation), so it no longer swims so high up. The container sinks and the recorder needle deflects upwards via the pulleys. The lungs have gained volume.
Modern spirometers usually only measure the flow velocity and can then deduce the lung volumes via integration.
The most common techniques used to measure respiratory flow are:
BTPS correction
In order to correctly deduce the lung volume from the respiratory flow, the "BTPS" measured values must be corrected. BTPS conditions ("body temperature, pressure, saturated with water vapor") describe the conditions inside the body. The air in the lungs has body temperature (37 ° C) and is 100% saturated with water. When you exhale, the air cools down and loses moisture, which means that the spirometer calculates smaller volumes than are actually available. High-quality spirometers must therefore always have a measurement of at least temperature and ideally also humidity in order to be able to correct this error.
Diagnostic significance
If ventilation values deviate from the respective norm at rest, this can indicate lung diseases. A comparison with expected values is carried out for this purpose. Patients with COPD and asthma sufferers often have regular spirometry tests for lung function. The spiroergometry is mainly carried out to record physical performance.
early detection
For people with breathing difficulties, spirometry is a health insurance benefit. For people without breathing difficulties, it is a self-pay service (IGeL). In 2017, the IGeL monitor of the MDS ( Medical Service of the Central Association of Health Insurance Funds ) examined whether the examination is useful or harmful in this case and rated the spirometry for checking lung function as "tending to be negative". Because the scientists found no studies on the benefits or harm of spirometry in people without symptoms. The most important sources are two reviews. According to the IGeL-Monitor, it is unclear whether one gains more life or more quality of life if asthma or COPD are detected and treated early. However, there are indications of damage, as early detection can treat diseases that would not have caused any problems. Four international, high-quality guidelines either do not recommend spirometry for early diagnosis or even advise against it.
Procedure and measurement parameters
During the measurement the software of the spirometer should display the spirogram . For this purpose, the volume is plotted against time and a flow-volume curve is created, for which the flow velocity is shown over the volume that is breathed.
The Tiffeneau or FVC test is performed during the examination. The patient first breathes out as deeply as possible. This is followed by a maximum possible and brisk inhalation, whereupon the patient exhales as quickly, strongly and again to the maximum extent possible.
The somewhat complex maneuver shows that the success of the examination also depends on the patient's motivation and cooperation. The patient should be given clear instructions prior to the examination. In addition, the examination should be repeated and the parameters should not deviate by more than 5% with good cooperation. Non- cooperation- independent methods such as oscillometry are rarely used in practice.
The most important parameters are:
- Flow parameters
- One-second capacity (FEV1)
- Peak Flow (PEF)
- Volume parameters
- Vital capacity (VC) and forced vital capacity (FVC)
- Tidal volume
- inspiratory reserve volume (IRV), describes the volume that can be additionally inhaled after normal inspiration
- Expiratory reserve volume (ERV), describes the volume that can still be exhaled after normal expiration
- FEV1% (quotient of FEV1 and FVC)
The vital capacity is calculated from the amplitude of the inspiratory and expiratory volume. Residual volume (RV), i.e. the amount of air that remains in the lungs after maximum exhalation, and the total lung capacity (TLC) cannot be determined with spirometry. A body plethysmograph must be used for this.
literature
- Robert E. Hyatt et al .: Interpretation of Pulmonary Function Tests: A Practical Guide. 4th edition. Wolters Kluwer, Philadelphia 2014, ISBN 978-1-4511-4380-5 .
- S2k guidelines for spirometry of the German Society for Pneumology and Respiratory Medicine (DGP). In: AWMF online (as of 2015)
Web links
- Spirometry on Vimeo (examination procedure / German Respiratory League eV )
- Recommendations of the German Respiratory League for Spirometry Year of publication: 2006 (PDF; 1.1 MB)
- Martin Bösch, Martin Thalmann: Practice website
- Dynamic Measurement Technologies: Online calculator for calculating the BTPS correction factor, age-specific expected values and other calculations.
Individual evidence
- ↑ IGeL-Monitor: Spirometry to check lung function , accessed on March 14, 2019. More on the justification for the assessment in " Detailed evidence ", accessed on March 14, 2019.
- ↑ Eisenmann et al .: Effectiveness of a COPD screening using spirometry , Quick Assessment, 2010, and Guirguis-Blake et al .: Screening for chronic obstructive pulmonary disease: A systematic Evidence Review for the US Preventive Service Task Force , 2016, Agency for Healthcare Research and Quality; Evidence Synthesis Number 130; AHRQ Publication No. 14-05205-EF-1. 2016
- ↑ Süddeutsche Zeitung, Many self-payer health services do more harm than good , February 16, 2017.
- ^ 1 .: US Preventive Services Task Force (USPSTF), Siu, AL et al. Screening for Chronic Obstructive Pulmonary Disease: US Preventive Services Task Force Recommendation Statement . Jama, 2016; 315 (13): 1372-137. 2 .: American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Diagnosis and Management of Stable Chronic Obstructive Pulmonary Disease , 2011. 3rd: Global initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease . 2016. 4th: The Royal Australian College of General Practitioners (RACGP). Guidelines for preventive activities in general practice . 2012. List also in " Evidence in detail ", p. 21f