Tonsillectomy
Tonsillectomy ( tonsil operation ), abbreviated TE , is the complete surgical removal of the tonsils ( tonsillae palatinae ). The tonsillectomy is one of the most frequently performed procedures in the operative ENT area.
history
Operations on the tonsils have been known for a long time. However, until the introduction of the real tonsillectomy in 1890 by Edwin Pynchon, only a partial removal of the tonsils was carried out using fingernails or knives, which is now known as tonsillotomy . The oldest references can be found in the Atharvaveda and are dated to 700 BC. Estimated. Further descriptions can be found in the Corpus Hippocraticum (400 BC), in Celsus in his work De Medicina (approx. 30 AD) Aetius von Amida described in the 6th century in a very differentiated way: “The part that protrudes, d. H. about half of the enlarged gland may be removed. Those who extirpate the whole gland also remove completely healthy structures and can then cause dangerous bleeding ”. Only the development of improved instruments and the introduction of intubation anesthesia made the complete removal of the organ possible. The technique of TE, which was initially carried out in two separate operations, was changed at the turn of the century by William Lincoln Ballenger (1897) and Ovidus Arthur Griffin (1906) so that the simultaneous removal of both tonsils in one operation was made possible.
indication
The indication for tonsil surgery is subject to constant change. The tonsillotomy was initially intended to remove foci of infection or abscesses , but after the introduction of TE as a result of the focus theory and in the absence of antibiotics, this operation was carried out very often. In 1928, J. Zarniko spoke of an "industrially minted surgical frenzy". The TE was very often carried out prophylactically in order to avoid spreading of the bacterial foci in the tonsils . Scarlet fever in particular, with the dreaded consequences of heart and kidney damage , has long been in the foreground. In 1941 (in the pre-antibiotic period) Kaiser gave a lecture on the reduction of throat infections in children after TE, so that until the 1960s, when penicillin was available for oral use in children , TE was almost regular in childhood. It was not until 1984 that Paradise published a study on tonsillitis in children, in which rules of indication for TE were established, which are essentially still valid today: ≥ 7 episodes in the last year, or ≥ 5 episodes annually in the last 2 years, or ≥ 3 episodes annually for the past 3 years. The episodes must clearly be tonsillitis and be documented by a doctor, as well as include at least one of 4 additional symptoms in addition to the "sore throat" symptom (temperature> 38.8 ° C, cervical lymph nodes (painful to pressure or> 2 cm), tonsil exudate ("white plaque “), Detection of β-hemolytic streptococci A). In 2013, Gysin added that only about 15% of sore throats in children were caused by streptococcal tonsillitis, the rest by viral pharyngitis , which led to the conclusion that a differentiation should be made on the basis of a scheme modified by Centor for children in order to to differentiate real tonsillitis from general, uncomplicated sore throat. This also applies to adults in order to be able to make a clear indication for surgery. As new antibiotics were introduced in the 1960s and 1970s, the indication for TE became increasingly restrictive. In the following decades, the surgical therapy of sleep apnea by means of greatly enlarged tonsils increasingly came to the fore, which then brought about a renaissance of the tonsillotomy since the late 1990s, since a complete removal of the tonsils is not justified when enlarged. Two meta-studies by Stuck (2008) and Gysin (2013) deal with studies on the question of TE in childhood. It was found that the term “chronic tonsillitis” was not validly defined, so it would be better to speak of “recurrent inflammation”. Stuck formulates that there is no study that proves "that a tonsillectomy for so-called" focus restoration "could somehow positively influence the course of allergic diseases, autoimmune diseases, dermatological or rheumatic diseases". As things stand today, no indication for TE is justified for the prophylaxis of rheumatic fever or for focussing before organ transplantation .
An obligatory indication for tonsillectomy is suspected malignancy (e.g. tonsil carcinoma , lymphoma ). In the case of a peritonsillar abscess , a decision should be made on a case-by-case basis on the basis of first occurrence, recurrence and general symptoms. An incision drainage or needle puncture represents a treatment variant with few complications in the uncomplicated first event according to Herzon. In 2003, Johnson did not find any superiority of the two methods incision or TE in his evidence-based literature evaluation. Based on a meta-analysis of studies, Windfuhr (2005) recommends an incision first if the picture is uncomplicated, otherwise an immediate tonsillectomy, and antibiotics for at least 1 week for both procedures. In the case of mononucleosis , TE is only indicated if there is a vital indication (shortness of breath, pronounced swallowing disorder). According to more recent findings, an adeno-tonsillectomy (removal of the pharynx and both palatine tonsils in one session) can have a positive effect on the course of the disease in PFAPA syndrome .
Guidelines
Recommendations for the indication have been drawn up in various states, often based on the Paradise criteria. In Germany there has been an S2k guideline on tonsillitis and its therapy since September 2015 (deviating from the Paradise criteria), as well as an S3 guideline drawn up by general practitioners on the subject of "sore throats". Sweden has a "tonsil register" which records all tonsil procedures. The guidelines were revised in 2010 as a result of new knowledge gained from the data collected. A 2013 survey in Italy showed that the ENT clinics surveyed hardly paid any attention to the guidelines drawn up in 2003 and revised in 2008 in their everyday clinics.
| country | Year of 1st publication | Year of revision |
|---|---|---|
| Germany | 2015 | |
| Austria | 2007 | |
| Italy | 2003 | 2008 |
| Croatia | 2009 | |
| Netherlands | 2009 | |
| Scotland | 2010 | |
| Sweden | 2007 | 2010 |
| United States | 2011 | |
| France | 2012 | |
| Australia | 2008 |
frequency
The frequency of tonsillectomies changed with the changing indications for surgery. In Germany, for example, a declining frequency can be observed, but an increase in tonsillotomy (operative partial removal of the palatine tonsil). According to the Federal Statistical Office, the number of operations in Germany (TE without adenotomy, OPS code 5-281.0) in 2005 was 77,765 operations and fell continuously to 58,955 in 2013. If the number of operations is differentiated according to patient age, there is an increase in primary school age (3,790 in 2013 aged 5-10 years) and a second peak in adolescent age (7,099 male and 15,266 female patients aged 15-25 in 2013). Long-term observation in Denmark from 1980 to 2001 also found a significant accumulation of female adolescent patients for which no explanation was possible. Spicker examined PD patients with regard to psychological peculiarities and found, in addition to an accumulation of female patients between the ages of 10 and 20, increasingly conspicuous results for this group in the Freiburg Personality Inventory (FPI-R) (subscales “social orientation” and “aggressiveness”) in one Third even a noticeable personality profile (with correlations to the subscales “physical complaints”, “excitability” and “aggressiveness”). He suspects that psychological complaints in this age and gender group could increasingly manifest themselves somatically in the throat area.
Surgical procedure
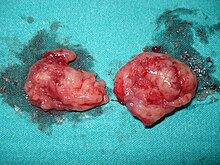
At the beginning of the "modern" tonsil removal, extended tonsillotomies were first performed using guillotine-like cutting knives (e.g. Ph. S. Physick (1828), Morrel Mackenzie (1880)). The problem arose from the remaining tonsil tissue, since the tonsil capsule was not dissected. The first real complete removal, using caustic (called “hot” TE), was performed in Chicago in 1890 by Edwin Pynchon. He recommended a separate removal of the tonsils with two operations two weeks apart. At the same time, techniques of removal using special scissors were developed, in which some authors first performed a tonsillotomy and then removed the remains of the tonsil by dissecting the tonsil capsule. The technique of "cold TE" with a representation of the tonsil capsules, which is still practiced today in a very similar form, was first described in 1906 by William Lincoln Ballenger and Ovidus Arthur Griffin. In the course of the next few decades, further and new developments of TE instruments were presented around the world, which, such as the self-retaining tongue depressor, enabled a significantly better overview of the operating theater area. The standard procedure ("cold" TE) recommended in operating room instructions in German-speaking countries first describes the severing of the mucous membrane in the area of the anterior palatal arch. Then the tonsil capsule is found and the tonsil is peeled off along the capsule with a toothed raspatory (rarely blunt with the finger) and, if necessary, sharply with scissors if there is scarring. The tonsil is cut off at the lower pole with a tonsil stringer (e.g. according to Brünings ). Bleeding is brought to a standstill by compressing the swab and, if necessary, using electrocautery or ligatures.
There are also other surgical procedures, some with laser, some with different thermal cutting processes, whereby significant advantages - in particular a lower rebleeding rate - have not yet been clearly demonstrated. This is discussed controversially in medical journals.
The procedure is usually performed under anesthesia , only rarely under local anesthesia. The surgery itself usually takes 20 to 30 minutes.
In Germany and Austria, tonsillectomy is usually carried out under inpatient conditions and is associated with a hospital stay of five to eight days. In Great Britain, the TEs are carried out on an outpatient or inpatient basis with one to two nights, depending on the hospital operator and patient-related factors. An overview by the OECD , based on information on individual countries from 2008 to 2013, shows that TE is mainly carried out in an inpatient setting in most member countries: Only in Belgium (29.4%), Canada (25.2%), Finland (16.0%), the Netherlands (31.7%), Sweden (36.8%) and the USA (3.0%) the rates of inpatient TEs are below 40%, with 100% the highest in Slovenia and Hungary, in Austria to 99.9%, in Germany to 96.4%.
Risks and Complications
The most common complication after a tonsillectomy is rebleeding. It occurs with a frequency of 1 to 6%, usually on the first or second and on the fifth or sixth postoperative day. An age-specific recording of the rebleeding rate in 2010 by the Federal Statistical Office shows an age-related increase in the rebleeding rate up to the age of 15 of 2.8% for under 5 year olds, over 4.4% for 5-10 year olds up to 5.3% for 10-15 year olds. While the number of female PD patients aged> 15 years only increases minimally to 6%, otherwise it is more or less the same, the rebleeding rate in male patients increases to 11.4% in the group of 25-30 year olds , only then falls slightly continuously. The rebleeding rate over all ages was 7.02% for men and 5.02% for women. The data for 2013 are almost identical. In children in particular, careful monitoring is required if there is a bleeding, possibly including re-admission to hospital. In the case of smaller accumulations of blood, measures such as putting on an ice tie are sufficient; in the case of heavier bleeding, surgical hemostasis must be carried out by vascular ligature or electrocoagulation; in extremely rare cases, secondary bleeding can be life-threatening and possibly fatal. Then a ligature of the external carotid artery and / or its branches, possibly including foreign blood transfer, is necessary. In the case of recurrent bleeding that cannot be surgically cured, after angiography of the carotid artery, embolization of the terminal branch concerned can also take place.
Injuries or damage to the tongue, soft palate, uvula and teeth are rare complications.
Damage to the soft palate can lead to open nostrils and the leakage of food and liquids from the nose. This usually subsides after a while.
If a piece of almond remains after the operation, inflammation can occur again (so-called residual tonsillitis). The pressure of the tongue spatula, which is inserted during the operation to keep the mouth level open, can damage the sensitive tongue nerve (lingual nerve) and lead to temporary, very rarely permanent, taste disturbances or numbness of areas of the tongue. In the extremely rare injury of the motoric tongue nerve (hyopglossus nerve), movement restrictions of the tongue and possibly speech disorders can result. There are seldom temporary, even more seldom permanent, taste disturbances and the lumpy and nasal sound of speech. The intervention can change the vocal sound temporarily or permanently by changing the resonance space. Patients with vocal or speaking professions should therefore inform the doctor about their profession before the operation.
Before a tonsil operation, the doctor must carefully take a medical history to avoid bleeding complications. Particular attention should be paid to whether medication is being taken that may cause a tendency to bleed (e.g. aspirin) or whether there are blood disorders in the family (haemophilia). A blood sample from children, however, is not absolutely necessary.
In Austria in 2007, after several deaths, the Austrian Society for Otorhinolaryngology, Head and Neck Surgery and Pediatric and Adolescent Medicine issued a joint recommendation on tonsillectomies in children before the age of six, after which only the indication of frequent tonsillitis TE should be performed, tonsillotomy for tonsil hyperplasia (enlarged tonsils) .
According to a cohort study published in 2018, tonsillectomy in childhood is associated with an increased long-term risk of respiratory , infectious and allergic diseases . It was u in this study. a. found a 2 to 3-fold increase in upper respiratory disease after tonsillectomy.
Pain
Most adults perceive wound pain as severe to very severe. Often these do not occur immediately after the operation, but rather after a delay of a few days. They last about two weeks, in rare cases up to four weeks, and can radiate into the ears, tongue and rows of teeth. According to a study from 2015, tonsillectomy is one of the most painful surgical interventions, even when compared to much larger operations. Metamizole (e.g. Novalgin) or Diclofenac (e.g. Voltaren) are often used to combat pain . Due to the high pain intensity, however, these active ingredients are often not sufficient to achieve a tolerable level of pain for the patient, so that the use of stronger opioid analgesics, such as tramadol , tilidine or even morphine in individual cases, may be necessary. Several studies criticize the fact that the pain intensity after tonsillectomy is underestimated by many doctors, which can lead to patients not receiving adequate pain therapy. Acetylsalicylic acid-containing agents such as aspirin should be avoided at all costs before and after the operation, as these agents can greatly increase the risk of rebleeding due to their anticoagulant effect. In general, it is recommended to take the prescribed pain medication regularly, and not only when pain occurs, in order to avoid pain peaks. For the first pain relief, especially in children, ice cream is used.
Aftercare
After the operation, depending on the healing process and professional activity, an inability to work of around three weeks can be expected. During this time, the patient should take it easy and avoid physical activity, as this would increase blood pressure and thus increase the risk of rebleeding. Strong physical exertion, such as sport or lifting heavy loads, should be avoided for at least three, better four weeks.
You should avoid any kind of sour, spicy, hard or hot food within the first two postoperative weeks, as these can cause severe pain. Fruit acids should also be avoided; tomatoes are particularly aggressive. Applesauce and other canned fruit are generally well tolerated, and grated pears and mango are also well tolerated. Cold drinks should be preferred for drinks, carbonated drinks can also cause severe burns to the wound. No fruit juices may be drunk. In spite of the severe pain, however, regular consumption of food is absolutely necessary so that the incrustations can be abraded and healing can begin more quickly.
Showering and shampooing is not recommended for up to a week after surgery. Even afterwards, care should be taken to ensure that the water is not too warm in order to avoid any secondary bleeding that could result from the increased blood flow to the body when showering. The teeth should be brushed with particular caution in the first week without using toothpaste. Until the wound has healed completely, toothpaste containing menthol should be avoided, as it is very irritating to the wound.
See also
Individual evidence
- ↑ a b c d Jochen Windfuhr: Differentiated tonsil surgery . In: ENT information . No. 3 , 2013, p. 97-100 .
- ↑ J. Stadler: About the tonsillotomy, its indications and dangers. Dissertation. Munich 1889.
- ↑ a b JA Koempel: On the origin of tonsillectomy and the dissection method . In: Laryngoscope . tape 112 , no. 9 , 2002, p. 1583-1586 , PMID 12352667 .
- ↑ Albert D. Kaiser: Effect of Tonsillectomy on Respiratory Infections in Children . In: Bull NY Acad Med . tape 18 , no. 5 , 1942, pp. 338-346 , PMID 19312269 , PMC 1933797 (free full text).
- ↑ JL Paradise, CD Bluestone, RZ Bachman, DK Colborn, BS Bernard, FH Taylor, KD Rogers, RH Schwarzbach, SE Stool, GA Friday ao: Efficacy of tonsillectomy for recurrent throat infection in severely affected children. Results of parallel randomized and nonrandomized clinical trials . In: New England Journal of Medicine . tape 310 , no. 11 , 1984, pp. 674-683 , PMID 6700642 .
- ↑ RM Centor, JM Witherspoon, HP Dalton, CE Brody, K. Link: The diagnosis of strep throat in adults in the emergency room . In: Med Decis Making . tape 1 , no. 3 , 1981, p. 239-246 , PMID 6763125 .
- ↑ J. Aalbers, KK O'Brien, WS Chan, GA Falk, C. Teljeur, BD Dimitrov, T. Fahey: Predicting streptococcal pharyngitis in adults in primary care: a systematic review of the diagnostic accuracy of symptoms and signs and validation of the Centor score . In: BioMed Central . tape 1 , no. 9 , 2011, p. 67 , PMID 21631919 , PMC 3127779 (free full text).
- ^ GN Grob: The rise and decline of tonsillectomy in twentieth-century America . In: J Hist Med Allied Sci . tape 62 , no. 4 , 2007, p. 383-421 , PMID 17426070 .
- ^ GP Garrod: The relative antibacterial activity of four penicillins . In: Br Med J . tape 10 , 1960, p. 1695-1696 , PMID 13703756 , PMC 2098302 (free full text).
- ↑ YES Koempel, CA Solares, PJ Koltai: The evolution of tonsil surgery and rethinking the surgical approach to obstructive sleep-disordered breathing in children. In: J Laryngol Otol . tape 120 , no. 12 , 2006, p. 993-1000 , PMID 16618912 .
- ↑ a b Boris A. Stuck, Jochen P. Windfuhr, Harald Genzwürker, Horst Schroten, Tobias Tenenbaum, Karl Götte: The tonsillectomy in childhood . In: Deutsches Ärzteblatt . tape 105 , no. 49 , 2008, p. 852-860 , PMID 19561812 ( online article [accessed September 29, 2013]).
- ↑ C. Gysin: Indications of pediatric tonillectomy . In: ORL . tape 75 , no. 3 , 2013, p. 193-202 .
- ↑ FS Herzon: Peritonsillar abscess: incidence, current management practices, and a proposal for treatment guidelines. In: Laryngoscope . tape 105 , 8 Pt 3 Suppl 74, 1995, p. 1-17 , PMID 7630308 .
- ^ RF Johnson, MG Stewart, CC Wright: An evidence-based review of the treatment of peritonsillar abscess . In: Otolaryngology - Head and Neck Surgery . tape 128 , no. 3 , 2003, p. 332-343 , PMID 12646835 .
- ↑ Kenneth Tyson Thomas, Henry M. Feder Jr, Alexander R. Lawton, Kathryn M. Edwards: Periodic fever syndrome in children . In: Journal of Pediatrics . tape 135 , 1999, pp. 1–5 , doi : 10.1016 / S0022-3476 (99) 70316-1 ( only abstract free [accessed November 20, 2016]).
- ↑ Greg Licameli, Maranda Lawton, Margaret Kenna, Fatma Dedeoglu: Long-term Surgical Outcomes of Adenotonsillectomy for PFAPA Syndrome . In: Arch Otolaryngol Head Neck Surg . tape 138 , no. 10 , 2012, p. 902-906 , doi : 10.1001 / 2013.jamaoto.313 , PMID 23069819 .
- ↑ a b Guideline "Inflammatory diseases of the tonsils / tonsillitis, therapy" available as a PDF document
- ↑ Guideline sore throat
- ^ E. Hultcrantz, E. Ericsson: Factors Influencing the Indication for Tonsillectomy: A Historical Overview and Current Concepts . In: ORL . tape 75 , no. 3 , 2013, p. 184-191 .
- ↑ Giovanni Motta, Sergio Motta, Pasquale Cassano, Salvatore Conticello, Massimo Ferretti, Bruno Galletti, Aldo Garozzo, Gennaro Larotonda, Nicola Mansi, Emilio Mevio, Gaetano Motta, Giuseppe Quaremba, Agostino Serra, Vincenzo Tarantino, Paolo Tavormina, Claudio Vicini, Maurizio Vicini Giovanni Vigili, Domenico Testa: Effects of guidelines on adeno-tonsillar surgery on the clinical behavior of otorhinolaryngologists in Italy . In: BMC Ear Nose Throat Disord . tape 13 , no. 1 , 2013, PMC 3545732 (free full text).
- ↑ a b Joint recommendation of the Austrian Society for Otorhinolaryngology, Head and Neck Surgery and Pediatrics and Adolescent Medicine for the removal of tonsils (PDF; 238 kB)
- ↑ Sistema Nazionale Linee Guida: Appropriateness and safety of tonsillectomy and / or adenoidectomy . ( online in English and Italian [accessed October 4, 2013]).
- ↑ AT Andrasević, T. Baudoin, D. Vukelić, SM Matanović, D. Bejuk, D. Puzevski, M. Abram, G. Tesović, Z. Grgurev, G. Tomac, I. Pristas: [ISKRA guidelines on sore throat: diagnostic and therapeutic approach - Croatian national guidelines] Article in Croatian . In: Lijec Vjesn . tape 131 , no. 7-9 , 2009, pp. 181-191 , PMID 19769278 .
- ↑ HP Verschuur, CJ Raats, CJ Rosenbrand: [Practice guideline 'Adenoid and tonsil disorders in secondary care'] Article in Dutch . In: Ned Tijdschr Geneeskd . tape 153 , 2009, p. B295 , PMID 19818185 .
- ^ Scottish Intercollegiate Guideline Network: Management of sore throat and indications for tonsillectomy . 2010 ( PDF text [accessed on October 3, 2013]).
- ^ The National Board of Health and Welfare: Tonsillit, faryngit, peritonsillit . ( online in Swedish [accessed February 23, 2015]).
- ^ Reginald F. Baugh et al: Clinical practice guideline - Tonsillectomy in Children . In: Otolaryngol Head Neck Surg . tape 144 , 1 (Suppl.), 2011, pp. S1-S30 , doi : 10.1177 / 0194599810389949 ( free online article and PDF [accessed on November 20, 2016]).
- ↑ E. Lescanne, B. Chiron, I. Constant, V. Couloigner, B. Fauroux, Y. Hassani, L. Jouffroy, V. Lesage, M. Mondain, C. Nowak, G. Orliaguet, A. Viot, French Society of ENT (SFORL), French Association for Ambulatory Surgery (AFCA), French Society for Anesthesia, Intensive Care (SFAR): Pediatric tonsillectomy: Clinical practice guidelines . In: European Annals of Otorhinolaryngology, Head and Neck Diseases . tape 129 , no. 5 , 2012, p. 264-271 .
- ↑ a b c d e JP Windfuhr: Tonsillectomy: official figures and trends in Germany . In: Laryngo-Rhino-Otol . tape 95 , 4 (Suppl.), 2016, pp. S88-S109 , PMID 27128406 .
- ^ H. Vestergaard, J. Wohlfahrt, T. Westergaard, C. Pipper, N. Rasmussen, M. Melbye: Incidence of tonsillectomy in Denmark, 1980 to 2001 . In: Pediatr Infect Dis J . tape 26 , no. 12 , 2007, p. 1117-1121 , PMID 18043448 .
- ↑ E. Spicker, H.-J. Schultz-Coulon: On tonsillectomy accumulation in young women . In: ENT . tape 52 , no. 3 , 2004, p. 219-226 , PMID 15007515 .
- ↑ H. Feldmann: 2000 years of history of the tonsillectomy . In: Laryngo-Rhino-Otology . tape 76 , no. 12 , 1997, p. 751-760 , doi : 10.1055 / s-2007-997520 , PMID 9487490 .
- ↑ Jürgen Theissing, Gerhard Rettinger, Jochen Alfred Werner: ENT Operationslehre . Thieme, Stuttgart / New York 2006, ISBN 3-13-463704-9 .
- ^ National Prospective Tonsillectomy Audit . 2005 ( PDF document [accessed January 19, 2016]).
- ↑ R. Leuwer, S. Petri, F. Schulz, K. Püschel: Deaths after tonsillectomy and adenotomy. In: Laryngorhinootologie. 77, 1998, pp. 669-672.
- ↑ D. Baburi, G. Schlöndorff: Life- threatening and fatal tonsillectomy secondary bleeding. Dissertation. Techn. Hochsch. Aachen, 2009.
- ↑ J. Strauss, K. Becke, J. Schmidt: Coagulation disorders: It depends on the anamnesis. In: Deutsches Ärzteblatt. 103, issue 28-29, July 17, 2006, p. A1948.
- ↑ Sean G. Byars, Stephen C. Stearns, Jacobus J. Boomsma: Association of Long-Term Risk of Respiratory, Allergic, and Infectious Diseases With Removal of Adenoids and Tonsils in Childhood. In: JAMA Otolaryngol Head Neck Surg. , doi : 10.1001 / jamaoto.2018.0614 .
- ↑ a b W. Meißner: Pain intensity and therapy after various surgical interventions . In: Current knowledge for anesthetists . tape 41 , 2015 ([www.ai-online.info/abstracts/pdf/dacAbstracts/2015/2015-11-RC203.1.pdf] [PDF]).
- ↑ FU Metternich, T. Brusis, F. Parandeh-Shab: Pain therapy after tonsillectomy in adults . In: ENT . tape 46 , no. 1 , 1998, doi : 10.1007 / s001060050196 .