Oropharyngeal cancer
| Classification according to ICD-10 | |
|---|---|
| C09 | Tonsil carcinoma |
| C10 | Malignant neoplasm of the oropharynx |
| ICD-10 online (WHO version 2019) | |
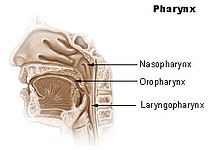
The oropharyngeal carcinoma (German, rarely used translation: oral throat cancer ) is a cancer of the oral pharynx ( pars oralis pharyngis , oropharynx or also called mesopharynx ). Together with hypopharyngeal carcinoma and nasopharynx carcinoma , oropharyngeal carcinoma belongs to the group of pharyngeal cancers , which in turn belong to the class of head and neck tumors . It is mostly squamous cell carcinoma . In addition, there are malignant lymphomas , adenoid-cystic and adenocarcinomas , and mucodermoid carcinomas.
Oropharynx
The oropharynx includes the areas from the soft part of the palate , the tonsils and the base of the tongue (the area where the tongue has grown). The tonsils are most frequently affected by the development of cancer ( tonsil carcinoma ).
Epidemiology
The incidence of oropharyngeal carcinoma is between 0.5 and 2 per 100,000 population per year. Men get sick about three to four times as often as women. The disease usually breaks out between the ages of sixty and seventy.
etiology
Lifestyle, environmental and genetic factors play a major role in the development of oropharyngeal cancer. Most patients with oropharyngeal were many years carcinogenic , that is exposed to carcinogenic substances ( exposed ). For tobacco consumption in the form of cigarettes , pipe tobacco and cigars, there is a direct dose-effect relationship. It significantly increases the risk of developing cancer in the throat and pharynx. An increased consumption of alcohol and tobacco was found in 85 percent of the patients suffering from head and neck cancer .
Alcohol abuse in particular is a cofactor in the development of oropharyngeal carcinoma. The mechanism of action of alcohol is not yet fully understood. Different models are currently being discussed: an accumulation of carcinogens on the mucous membranes and systemic effects of alcohol abuse, such as general immunodeficiency and damage to the liver. Outside of Europe, the consumption of chewing tobacco still plays a significant role in the development of oropharyngeal cancer.
Whether poor oral hygiene or poorly fitting dentures have an influence on the development of oropharyngeal cancer has not yet been proven.
Obviously there is also a connection with infections with the HP virus . A case-control study found a previous infection with an HP virus (type 16 and others) in patients suffering from oropharyngeal cancer significantly more often than in the non-infected control group. The relationship was independent of alcohol or tobacco consumption. The study concludes that HPV infection is "highly associated with the occurrence of oropharyngeal cancer in patients with or without the known risk factors of tobacco or alcohol consumption."
diagnosis
Oropharyngeal carcinoma can often be diagnosed by a mirror examination . As a rule, a pan endoscopy of the entire pharynx is also performed with anesthesia . Small tissue samples are taken from the patient by biopsy , which are examined in fine tissue to confirm the diagnosis .
Imaging methods such as sonography (ultrasound), computed tomography (CT) or magnetic resonance imaging (MRT) are used for tumor staging and therapy planning . While sonography provides a good overview of any possible involvement of the lymph nodes, the two other imaging methods can also determine the extent of the tumor in depth and infiltration of other structures such as B. the neck vessels are assessed. To examine for distant metastases , an X-ray or CT scan of the lungs and an ultrasound examination of the liver are usually done. Scintigraphy can be performed to rule out daughter tumors in the bone .
Oropharyngeal carcinoma is classified according to the size of the tumor in its greatest extent as follows:
- T1 tumor 2 cm or smaller
- T2 tumor larger than 2 cm but not larger than 4 cm
- T3 tumor larger than 4 cm in its greatest dimension
- T4 tumor infiltration into surrounding structures, such as bones , soft tissues of the neck or deep muscles of the tongue, regardless of the size of the tumor
A blood test cannot be used to establish or exclude a diagnosis.
therapy
The position of the tumor is decisive for the treatment of oropharyngeal cancer. Carcinomas of the tonsils (tonsils) are primarily operated on. Radiation therapy is usually carried out for larger tumors . In the case of cancer of the palate or tongue, high-dose radiation therapy is often the method of choice. It usually takes place five times a week over a period of seven weeks. The effectiveness of the therapy is significantly increased by additional chemotherapy .
Various surgical forms of dissection and en bloc resection are used to treat the regional lymph nodes .
forecast
The prognosis is essentially determined by the metastatic behavior of the tumor. With appropriate treatment, the following average five-year survival rates are achieved:
- Stage I: 90%
- Stage II: 75%
- Stage III: 45 to 75%
- Stage IV: <35%
Patients over the age of 70 usually have a worse survival rate than young patients.
Patients in whom HPV has been detected in the tumor have a better prognosis after surgery and radiation therapy (sometimes chemotherapy at the same time) than without HPV detection in the tumor. Instead of detecting high-risk HPV DNA, p16 can also be used as a surrogate parameter.
Individual evidence
- ^ NC Gellrich et al.: Head and neck tumors - recommendations for diagnosis, therapy and aftercare. ( Memento of July 14, 2006 in the Internet Archive ) 1st edition. Tumor Center Freiburg, April 2004.
- ↑ www.gesundheitpro.de, throat cancer , accessed on December 28, 2007 ( Memento from June 14, 2006 in the Internet Archive )
- ↑ MT Canto, SS Devesa: Oral cavity and pharynx cancer incidence rates in the United States, 1975-1998. In: Oral Oncol . 6/2002, pp. 610-617.
- ↑ a b J. A. Brennan et al .: Association between cigarette smoking and mutation of the p53 gene in squamous-cell carcinoma of the head and neck. In: N Engl J Med . 11/1995, pp. 712-717.
- ^ PA Newcomb, PP Carbone: The health consequences of smoking. In: Cancer Med Clin North Am. 76/1992, pp. 305-331.
- ↑ Jaber et al.: Risk factors for oral epithelial dysplasia - the role of smoking and alcohol. In: Oral Oncol. 35/1999, pp. 151-156.
- ↑ H. Maier et al .: Chronic alcohol consumption - the key risk factor for pharyngeal cancer. In: Otolaryngology - Head and Neck Surgery . 110/1994, pp. 168-173.
- ^ TM Perkins, I. Perkins: Chronic alcoholism: a common risk factor in oral cancer and alcoholic cirrhosis. In: Compend Contin Educ Dent. 2001, pp. 49-51.
- ^ DM Winn et al .: Snuff dipping and oral cancer among women in the southern United States. In: N Engl J Med. 304/1981, pp. 745-749.
- ↑ B. Singh et al .: Chromosomal aberrations in patients with head and neck squamous cell carcinoma do not vary based on severity of tobacco / alcohol exposure. In: BMC Genet. 3/2002, p. 22.
- ↑ W. Thumfart et al .: Chronic mechanical trauma in the etiology of oro-pharyngeal carcinoma. In: J Maxillofac Surg. 1978, pp. 217-221.
- ↑ Silke Tribius, Markus Hoffmann: Human papilloma viruses - a risk factor for oropharyngeal carcinoma. In: HIV & more. 2/2013.
- ↑ G. D'Souza et al: Case-Control Study of Human Papillomavirus and Oropharyngeal Cancer. In: The New England Journal of Medicine . 356/2007, pp. 1944-1956.
- ^ Health North Hesse: What is throat cancer? ( Memento from May 28, 2013 in the Internet Archive )
- ↑ M. Bremke: Value of the planned neck dissection after primary radio-chemotherapy of oropharyngeal and hypopharyngeal carcinomas in stage IV. Dissertation . Philipps University of Marburg, 2007. (PDF; 1.1 MB)
- ↑ ( Page no longer available , search in web archives: Clinic Third Order, Munich Nymphenburg, throat cancer treatment ), accessed on December 28, 2007
- ^ W. Millesi et al.: Regional diagnosis and therapy for squamous cell carcinoma of the oral cavity and the oropharynx. In: European Surgery. 30/1998, pp. 299-304. ISSN 1682-8631
- ↑ J. Pericot et al: Survival evaluation of treatment modality in squamous cell carcinoma of the oral cavity and oropharynx. In: J Craniomaxillofac. 2000, pp. 49-55.
- ^ RK de Cassia Braga et al .: Perioperative complications, comorbidities, and survival in oral or oropharyngeal cancer. In: Arch Otolaryngol Head Neck. 129/2003, pp. 219-228. PMID 12578453
- ↑ Gregor Heiduschka, Anja Grah, Felicitas Oberndorfer, Lorenz Kadletz, Gabriela Altorjai: Improved survival in HPV / p16-positive oropharyngeal cancer patients treated with postoperative radiotherapy . In: Radiation Therapy and Oncology . tape 191 , no. 3 , 2015, ISSN 0179-7158 , p. 209–216 , doi : 10.1007 / s00066-014-0753-7 ( springer.com [accessed August 18, 2019]).
literature
- I. Baumann et al.: Quality of life in patients with oropharyngeal cancer. In: ENT. 54/2006, pp. 376-381, ISSN 0017-6192 .
- MCL Seibolt: Retrospective study on health-related quality of life after primary operated and adjuvant irradiated oropharyngeal cancer. Dissertation . University of Tübingen, 2005.
- P. Koivunen et al .: Incidence and survival in patients with pharyngeal cancer in northern Finland. In: Eur Arch Otorhinolaryngol. 259/2002, pp. 543-546.
- MD Mignogna ua: Costs and effectiveness in the care of patients with oral and pharyngeal cancer: analysis of a paradox. In: Eur J Cancer Prev . 11/2002, pp. 205-208.