abscess
| Classification according to ICD-10 | |
|---|---|
| L02.- | Skin abscess, boils and carbuncles |
| L02.0 | Skin abscess, boils and carbuncles on the face |
| L02.1 | Skin abscess, boils and carbuncles on the neck |
| L02.2 | Skin abscess, boils and carbuncles on the trunk |
| L02.3 | Skin abscess, boils and carbuncles on the buttocks |
| L02.4 | Skin abscess, boils and carbuncles on extremities |
| L02.8 | Skin abscesses, furuncles and carbuncles in other locations |
| L02.9 | Skin abscess, furuncle and carbuncle, unspecified |
| L73.2 | Hidradenitis suppurativa |
| ICD-10 online (WHO version 2019) | |
An abscess is a collection of pus in an unpreformed body cavity, which is caused by inflammatory tissue melting. The melting of the tissue is known as abscess formation (in the case of pulmonary tuberculosis, it is also known as “cavernization”).
The subphrenic abscess (under the diaphragm located), the perityphlitische abscess (next to the appendix located) and the Douglasabszess are pathologically seen (as opposed to intra-abdominal abscesses ) no abscesses, but encapsulated empyema in the abdominal cavity .
Diagnosis
- clinical signs :
- Laboratory: increasing inflammation values ( CRP , leukocytes )
- diagnostic imaging: circumscribed fluid accumulation
- in ultrasound
- in computed tomography or magnetic resonance tomography (density determination also possible)
- Puncture:
- visible pus
- positive bacterial culture (and resistogram)
root cause
Abscesses can occur with no apparent external cause. But they can also be the result of an operation , an injection , a foreign body or a weak immune system in the person concerned.
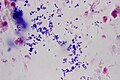
The majority of abscesses by an infection with bacteria caused. The chronic pathogen is often a form of Staphylococcus aureus . There are seldom sterile abscesses (so-called cold abscesses ) from whose pus no pathogens can be isolated.
The superficial abscesses show a typical inflammatory reaction with warming (hyperthermia) in the area. However, there are seldom cold abscesses without one, which is typical in tuberculosis . The body builds a protective wall of granulation tissue around an abscess , the so-called abscess membrane. The body concentrates defense cells in this edge wall. Since antibiotics in the blood usually do not diffuse through this membrane in sufficient concentration into the abscess cavity , antibiotic treatment alone is often not sufficient.
Multiple and recurring abscesses can indicate PVL- forming staphylococcus .
Causes in the mouth, jaw and face area
Bacterial inflammation that originates from teeth or the tooth holding apparatus is called odontogenic infections . They can be the cause of the formation of an (odontogenic) abscess in this area of the body.
Causes in the chest and rib cage area
A breast abscess can arise from puerperal or non-puerperal mastitis or as a result of a postoperative wound healing disorder .
As a result of severe (and necrotizing) pneumonia , after aspiration and in patients with weakened immune systems, a lung abscess (a localized and encapsulated suppuration within a lung area) can develop. Lung abscesses are usually treated surgically (with abscess drainage ) and antibiotics. The melting (abscessing) of lung tissue that sometimes occurs in the case of pulmonary tuberculosis is known as cavernization .
Causes in the spine area
Spinal anesthesia or epidural anesthesia can cause a spinal abscess in the spinal canal or an epidural abscess between the dura and periosteum if there is bacterial contamination.
Causes in the area of the abdomen
Intra-abdominal abscesses are often polymicrobial infections with evidence of anaerobes, Enterobacteriaceae, streptococci and enterococci. Special abscesses of the abdomen are the pus-forming liver abscess , the spleen abscess, retroperitoneal abscess and pancreatic abscess .
Causes in the area of the genitourinary system
Here, for example, renal abscesses (abscesses in the area of the kidneys) come into question, which are treated with antibiotics and, if necessary, drainage.
Other causes
There are several more disease-related causes of abscesses. For example, furuncolosis or pyoderma should be mentioned here. But acne inversa ( hidradenitis suppurativa ) can also be the cause of recurring abscesses in the large flexion regions of the body, such as armpits , groin or buttocks . Not every abscess, however, means such a severe chronic inflammatory dermatosis .
pathology
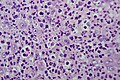
Histologically (when examined under a light microscope ) there is a circumscribed and dense accumulation of neutrophilic granulocytes (the largest subgroup of white blood cells ), which break down the local tissue through the release of enzymes and thereby form the abscess cavity. Depending on the location and cause of the inflammation, trapped hair shaft parts (ruptured folliculitis ), foreign bodies ( trauma ) or concretions (in the case of kidney abscesses from kidney stones ) can also be found. Fragments of submerged and not completely decomposed tissue can also lie freely in the abscess cavity as sequesters .
The abscess cavity is limited to the surrounding tissue by the pyogenic membrane ( abscess membrane ). Further neutrophils migrate into the abscess cavity via this wall of granulation tissue . In addition, the pyogenic membrane contains mononuclear macrophages (phagocytes) and - especially in the case of foreign material it contains - multinucleated giant cells that resorb the cave contents . Foreign materials can be highlighted under the microscope, depending on their nature, by examining them with polarized light , and pathogens contained in the cave contents by special coloring.
Outwardly, the abscess membrane is bordered by a seam-like fibrosis zone, within which activated fibroblasts (cells that form connective tissue) cause the formation of a pseudocapsule that locally limits the inflammation. If the inflammation can finally be contained by the immune system or appropriate therapy, the abscess cavity is first replaced by granulation tissue and finally connective tissue. Granulomas made of foreign material and accumulated aggregates of multinucleated giant cells can remain within or on the edge of this scar area .
The abscess-forming purulent inflammation in the context of a phlegmon must be differentiated from the abscess . Here, a dense infiltrate of neutrophilic granulocytes spreads diffusely in the tissue without being limited by an abscess membrane.
Complications
If an abscess is not treated adequately or improperly, it can empty through the skin in a fistulous manner, break into body cavities (e.g. into the lungs or as exudate in the pleural space ) or hollow organs or spread through the bloodstream, cause a brain abscess or other organ abscesses or in the worst case of sepsis ("blood poisoning") lead to the death of the person concerned.
therapy
Therapy consists of opening and draining the pus. This is done in the form of an operation in which after opening (or splitting the abscess) and emptying or clearing the abscess cavity is rinsed and a percutaneous drain is inserted. In the case of inaccessible abscesses, which often occur in the abdominal cavity or in the retroperitoneum , a percutaneous puncture and drainage are performed under sonographic or CT control . In the case of larger or poorly accessible abscesses, the operation is carried out under anesthesia ( anesthesia , spinal anesthesia or regional anesthesia ). In exceptional cases, soft tissue abscesses are opened using local infiltration anesthesia, which, however, carries the risk of spreading germs and is less effective than other anesthetic methods.
The sucked pus is examined bacteriologically to determine which pathogens caused the inflammation.
As a rule, and especially in the case of sepsis, treatment with one or more antibiotics is also an option . If PVL-forming staphylococci are found in the throat, a four-week therapy with an antibiotic in the form of a nasal ointment is recommended. Intensive hygiene measures such as cooking the bed linen and towels are also required.
Quote
The Latin quote still applies without restriction to the treatment of the abscess:
" Ubi pus, ibi evacua ."
"Where there is pus, there evacuate (him)."
See also
literature
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , passim.
Web links
- Patient information on oral abscess
- Treatment of abscesses with medicinal leeches
- Charité Berlin project on PLV-forming staphylococcus
Individual evidence
- ^ Bernhard Weigel, Michael L. Nerlich: Praxisbuch Unfallchirurgie . Springer-Verlag, October 7, 2011, ISBN 978-3-642-10789-4 , p. 870.
- ↑ Diethelm Wallwiener, Walter Jonat, Rolf Kreienberg, Klaus Friese, Klaus Diedrich, Matthias W. Beckmann: Atlas der gynäkologische Operations , 2008, Georg Thieme Verlag, ISBN 978-3-13-159517-1 , p. 652 ( limited preview in Google Book Search).
- ↑ Joachim Frey : Diseases of the respiratory organs. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 599-746, here: pp. 686-689 ( lung abscess ).
- ↑ Marianne Abele-Horn (2009), p. 96 f. ( Lung abscess ).
- ^ Klaus Holldack, Klaus Gahl: Auscultation and percussion. Inspection and palpation. Thieme, Stuttgart 1955; 10th, revised edition ibid 1986, ISBN 3-13-352410-0 , p. 88 f.
- ↑ Gerd-Gunnar Hanekop, Dietmar Beck: Spinal cord near pharmacotherapy. In: Eberhard Aulbert, Friedemann Nauck, Lukas Radbruch (eds.): Textbook of palliative medicine. With a foreword by Heinz Pichlmaier. 3rd, updated edition. Schattauer, Stuttgart 2012, ISBN 978-3-7945-2666-6 , pp. 208-223, here: pp. 213-216.
- ↑ Marianne Abele-Horn (2009), p. 68 ( subdural empyema, epidural abscess ).
- ↑ Marianne Abele-Horn (2009), pp. 126–129 ( intra-abdominal abscesses ).
- ↑ Marianne Abele-Horn (2009), p. 138.
- ↑ Max Eder, Peter Gedigk (ed.): General pathology and pathological anatomy . 33., rework. Springer, Berlin 1990, ISBN 0-387-51899-1 , pp. 138 .
- ↑ Berthold Jany, Tobias Welte: Pleural effusion in adults - causes, diagnosis and therapy. In: Deutsches Ärzteblatt. Volume 116, No. 21, (May) 2019, pp. 377-385, here: p. 379.