Spinal anesthesia
A spinal anesthesia (from latin spinalis to the spinal column / spinal cord properly, and anesthesia ) or lumbar (from Latin lumbalis to loin duly) is a neuraxial form of regional anesthesia . By injecting a local anesthetic (and possibly other drugs) into the cerebral water space ( subarachnoid space ) at the level of the lumbar spine, the transmission of signals to the nerves from the spinal cord is inhibited. This creates a temporary, reversible blockade of the sympathetic nervous system , the sensitivity and the motor skills of the lower half of the body. Possible side effects include circulatory fluctuations, nausea, and back pain and post-puncture headaches that can occur in the days following the procedure. Serious complications (bruises or infections near the spinal cord, nerve damage) are rare.
The method, which was introduced into clinical practice at the end of the 19th century, lost its importance with advances in the field of anesthesia (general anesthesia). In the 20th century, discoveries about the advantages of regional anesthesia in certain patient groups led to a renaissance of this technique. As a standard method of anesthesia spinal anesthesia will be held today use in a variety of operations on the lower abdomen, the pelvis, the lower extremity and in the obstetrics and provides these procedures as an alternative to other neuraxial regional techniques such as epidural anesthesia (syn. Epidural ) and general anesthesia represent.
Overview of the procedure
Anatomical principles and principles of spinal anesthesia

The human spine consists of 24 vertebrae that ensure the mechanical stability of the body axis. These are connected by firm ligaments and each consist of a vertebral body, a vertebral arch that surrounds the spinal cord (1 in the figure) and its membranes, as well as two transverse processes and a spinous process on the backward ( dorsal ) side. Spinal nerves emerge between the vertebrae , which innervate the body segmentally and thus enable motor skills and sensitivity , and also guide fibers of the autonomic nervous system .
As part of the central nervous system , the spinal cord is surrounded by the meninges . From the inside out, these are the soft meninges ( pia mater ), which lies directly on the spinal cord, the spider skin ( arachnoid ) and, as the outer boundary, the hard spinal cord skin ( dura mater ). Between the pia mater and the arachnoid there is the cerebral water space ( subarachnoid space , liquor space), in which the cerebrospinal fluid ( liquor cerebrospinalis ) circulates.

In spinal anesthesia, this CSF space is punctured with a thin cannula, whereby the needle penetrates the skin, the ligamentous apparatus between the spinous processes of the vertebrae ( ligamentum supraspinal , ligamentum interspinale , ligamentum flavum ), the peri-or Epidural space (3 in the figure), which penetrates the dura and the arachnoid and comes to rest with the tip in the liquor space (2 in the figure). Local anesthetics are injected into this ( intrathecally ) , which act on the anterior and posterior roots of the spinal nerves and temporarily suspend their ability to transmit nerve impulses.
During human development, the spinal column grows faster than the spinal cord, so that the spinal cord (in adults) ends at the level of the first / second lumbar vertebra in the conus medullaris , but the associated spinal nerves extend further towards the foot ( caudal ) and emerge from the spinal canal. They form the horse's tail ( cauda equina ). This allows a puncture at the level of the middle lumbar vertebrae without injuring the spinal cord.
Differentiation from other procedures
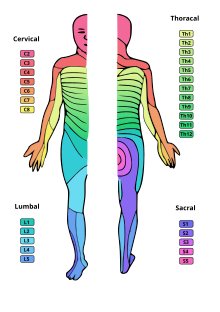
In spinal anesthesia, the needle penetrates the hard meninges (dura mater) so that the injected local anesthetic can spread freely in the cerebrospinal fluid of the subarachnoid space and nerve fibers are numbed there. With epidural anesthesia, on the other hand, the dura mater is not pierced. The inserted catheter comes to lie outside of the same in the epidural space, so that the local anesthetic acts mainly outside of the meninges on the spinal nerves branching out from the spinal cord. While in spinal anesthesia all nerve fibers below the puncture site and thus the entire lower half of the body are numbed through the distribution of the medication, in epidural anesthesia the anesthesia is emphasized in the corresponding dermatomes of the puncture height.
With a lumbar puncture , the CSF space is punctured in the same way as with spinal anesthesia. It is used for CSF pressure measurement and diagnostic CSF removal , which is carried out in the event of suspected infections of the central nervous system, metastasis and for antibody diagnostics . As part of chemotherapy , cytostatics are also injected intrathecally by means of a lumbar puncture .
variants
The spinal anesthesia is usually carried out as a single injection (single shot) . Depending on the extent of the sensory blockade, a distinction is made between deep (below dermatome / segment Th 12, level of the groin ), medium-high (up to segment Th 10, level of the navel ) and high (up to segment Th 4, level of the nipples ) spinal anesthesia. A special form of spinal anesthesia is the saddle or sacral block , in which the expansion is limited to the sacral spinal nerves, which mainly supply the genital area (S2–5).
By inserting a catheter , in contrast to a single puncture, drugs can be continuously introduced (applied) (continuous spinal anesthesia, CSA). Another variant is the combination of a spinal with an epidural anesthesia ( combined spinal and epidural anesthesia , CSE). A spinal needle is pushed through the lying epidural needle and spinal anesthesia is performed. An epidural catheter is then inserted into the epidural space. The lying catheter enables the dosage of medication as required and also an effective postoperative pain therapy.
Determinants of the dispersion height
The effective level of the spinal anesthesia depends on the spread of the injected active ingredients in the CSF space. This is primarily determined by the total dose and the density ( baricity ) of the local anesthetics. A distinction is made between isobaric solutions, which have the same density as the liquor, and hyperbaric preparations, which achieve a higher density through the addition of glucose . Isobaric solutions mostly remain in the area of the puncture site. The density is, however, slightly dependent on temperature, so that the spreading is more difficult to predict due to the warming in the body than with hyperbaric local anesthetics. The latter sink downwards (caudally) following the force of gravity, which means that the patient's position can control the spread. By lying flat, a spread comparable to the isobaric application can be achieved, by sitting a saddle block, by lying sideways, the anesthesia can be emphasized on one side. The use of hypobaric solutions with low density occurs only in exceptional cases.
Further factors (determinants) that influence the spread are the individually strongly fluctuating amount of CSF and the spatial conditions in the CSF space. The latter are influenced by the patient's stature: with increased pressure in the abdominal cavity, such as obesity ( obesity ), pregnancy or ascites , the liquor space is compressed and the dose must be reduced accordingly. The speed of the injection, the total volume injected and the deliberate multiple swirling of the local anesthetic with the liquor (barbotage) have less of an impact .
Pharmaceuticals used
The duration of the effect of the spinal anesthesia depends on the substances used. Local anesthetics are the standard medication for performing spinal anesthesia. They diffuse into the nerves , block sodium channels in the cell membrane and thereby reduce the influx of sodium ions. In this way the formation of action potentials is prevented and signal transmission in nerves is no longer possible.
Lidocaine was the standard for spinal anesthesia for a long time due to its short attack time and a medium-long duration of action of 60–90 minutes, but is rarely used after reports of temporary and permanent nerve damage. Bupivacaine is a widely used drug with a longer duration of action, for which, in contrast to lidocaine, only low rates of nerve damage have been described. Both isobaric and hyperbaric solutions exist. Mepivacaine , prilocaine and ropivacaine are other alternatives used. Procaine is used in the United States, but little used in Europe. The duration of action of prilocaine and mepivacaine is relatively short at around one hour, which makes it attractive to use for short and outpatient procedures . As a local anesthetic of the amino ester type , however, procaine has a higher risk of an allergic reaction than the other substances that belong to the amino amides.
By combining them with other drugs ( "adjuvants" ), the effect of the local anesthetics should be prolonged and side effects reduced. This is achieved, for example, through the often practiced addition of opioids . For this purpose, their fat-soluble forms, such as fentanyl or sufentanil , are used, which act via opioid receptors located in the dorsal horn of the spinal cord. Typical opioid side effects such as itching, nausea or reduced respiratory drive ( respiratory depression ) can occasionally occur. Water-soluble derivatives such as morphine cause much more severe respiratory depression and must therefore be dosed with caution and the patient should possibly be monitored for longer. The use of clonidine or ketamine is practiced less often. Adrenaline , which is added to the effect of other regional anesthesia procedures, is not suitable for use in spinal anesthesia.
Indications and contraindications
application areas
Spinal anesthesia is a standard method of anesthesia that is relatively easy to carry out, takes effect quickly and completely eliminates pain. It represents an alternative to anesthesia and epidural anesthesia, which can be used for surgical interventions on the lower abdomen ( e.g. inguinal hernia operations), gynecological and urological operations in the pelvic area, and orthopedic , trauma surgery or vascular surgery on the lower extremity . The continuous spinal anesthesia also offers the possibility of continued postoperative pain therapy . Spinal anesthesia, on the other hand, is unsuitable for operations on the upper abdomen and higher regions of the body.
In obstetrics , spinal anesthesia is used for a caesarean section (Caesarean section). In addition to epidural anesthesia, it is a standard procedure there, as anesthesia is avoided if possible due to the increased risk of aspiration . However, this is preferably used for emergency deliveries, in which the time until the epidural / spinal anesthesia fully takes effect cannot be waited for.
Spinal anesthesia is a way of avoiding such a complication in patients with a tendency to malignant hyperthermia , since the substances are not triggers for the disease. Spinal anesthesia can be given preference over general anesthesia, even if difficulties in securing the airway are to be expected and patients are not fasting . Patients with obstructive airways diseases ( bronchial asthma , COPD ) also benefit from not using anesthesia.
There are indications that the anesthesia procedures close to the spinal cord can reduce the rate of various complications ( leg vein thrombosis , pulmonary embolism , blood loss, pulmonary complications) and possibly also the mortality rate, but the data are not sufficient for a final assessment. The question of whether the spinal cord-related procedures offer advantages for patients with severe cardiac or pulmonary pre-existing diseases (diseases of the heart or lungs) is also controversial. A superiority over general anesthesia has not yet been shown.
Contraindications
Absolute contraindications are intolerance to the anesthetics used, local infections in the area of the puncture site, untreated body-wide infectious diseases ( bacteremia ), untreated volume deficiency ( hypovolemia ), increased intracranial pressure and a manifest tendency to bleed due to genetically determined coagulation disorders or therapeutic coagulation inhibition (see table ). Such treatment with anticoagulants must be paused for four hours with unfractionated heparin before performing spinal anesthesia , and twelve (prophylactic low dose) or 24 hours (therapeutic dose) with low molecular weight heparins. Clopidogrel must be discontinued seven days , ticlopidine ten days beforehand, after taking coumarins ( phenprocoumon and others) an INR <1.4 must be achieved. Treatment with low dose acetylsalicylic acid alone (up to 100 mg per day) no longer requires a break in treatment (recommendations of the German Society for Anesthesia and Intensive Care Medicine ).
A lack of blood platelets ( thrombocytopenia ) increases the risk of a bleeding complication. An absolute lower limit up to which spinal anesthesia can be performed has not been specified by the specialist societies. Rather, the overall coagulation situation must be taken into account. The transfusion of platelet concentrates to increase the platelet count in the blood before spinal anesthesia is recommended from a value of less than 50,000 / μl, so that this can be used as a guide for the lower limit. For epidural anesthesia, where thicker needles are usually used, a transfusion is recommended for less than 80,000 / μl.
Relative contraindications are chronic back pain, systemic infection under antibiotic treatment, ankylosing spondylitis , significant aortic stenosis or other heart valve defects , syringomyelia and pulmonary hypertension . In these conditions, the benefits of spinal anesthesia must be weighed against the risks.
| substance | Before puncture or catheter removal | After puncture or catheter removal |
|---|---|---|
| Unfractionated heparin (UFH) | 4-6 h | 1 h |
| Low molecular weight heparin LMWH prophylaxis | 12 h | 4 h |
| Low molecular weight heparin LMWH therapy | 24 hours | 4 h |
| Fondaparinux | 36-42 h | 6-12 h |
| Vitamin K antagonists | INR <1.4 | after catheter removal |
| Clopidogrel | 7 days | after catheter removal |
| Prasugrel | 7-10 days | 6 h |
| Ticlopidine | 10 days | after catheter removal |
| Abciximab | 48 h | 4 h |
| Tirofiban | 8 h | 4 h |
| Prostacyclin (PGI 2 ) | 0.5 h | immediately |
| Dabigatran etexilate | > 34 h | 4-6 h |
| Rivaroxaban | 22-26 h | 4-6 h |
| Apixaban | 26-30 h | 4-6 h |
| Ticagrelor | 5 days | 6 h |
| Cilostazol | 42 h | 5 h |
| Dipyridamole plus ASA | 48 h | immediately |
procedure
preparation
As with other anesthetic procedures a place in advance informed consent discussion between the patient and anesthesiologist instead. Sobriety must be observed on the day of the operation , as the procedure may have to be changed to anesthesia in the event of complications or insufficient effect. Often a soothing and tension-relieving agent ( sedative ) is administered as a premedication before the procedure .
Spinal anesthesia is performed on the patient while sitting or lying on their side. In a sitting position, the patient is supported from the front by an assistant. A venous access should be safe places, are emergency equipment. The patient is continuously monitored by means of basic monitoring (ECG monitoring, pulse oximetry , blood pressure measurement ).
execution
To apply spinal anesthesia, a spinal cannula is used to puncture between the second and third (L2 / L3) or third and fourth lumbar vertebrae (L3 / L4). After multiple disinfection and local anesthesia, the cannula is inserted between two spinous processes under sterile conditions. It is possible to puncture straight from the rear (median) in the plane of the spinous processes or with a slight lateral deviation of 10 ° (paramedian) . Alternatively, the lateral Taylor approach can be used, in which the puncture is made at an angle of 45 ° from the side and below.
The cooperation of the patient is important because he can increase the distance between the spinous processes by rounding the back ("cat hump"). Ossified ligaments prevent the needle from advancing, especially in older people. For this reason, a larger-lumen guide cannula (introducer) is often used. Once this has penetrated the ligament structures, the actual, thin puncture needle is inserted through it and the subarachnoid space is punctured. If the needle touches a nerve root, paresthesia may briefly occur in the legs during the puncture . After passing through the dura, the clear cerebrospinal fluid drips out of the needle and shows the doctor performing the procedure that the needle is correctly positioned.
The clear liquor can be recognized by the formation of streaks in the attached syringe with the local anesthetic. If the CSF is bloody (puncture of a blood vessel) or if there is no CSF backflow, the cannula must be removed and re-inserted. After injecting the dose of local anesthetic adapted to the patient, the effect sets in almost immediately and begins with a sensation of warmth in the legs or buttocks. In a matter of minutes, numbness and painlessness set in, as well as restricted mobility. By positioning the patient when using hyperbaric local anesthetics, the spread of the anesthetized area can be influenced (medium-high spread, sacral block, one-sided stressed anesthesia).
After injection of the anesthetic, depending on the substance used, a period of 1–2.5 hours is available for the surgical procedure . Often the patient is sedated by the intravenous administration of appropriate drugs (mostly benzodiazepines such as midazolam ) to reduce stress . During the entire duration of action, the patient must be monitored by specialist staff and technical monitoring, since earlier concepts of a "fixation time" of spinal anesthesia are now considered obsolete and complications can occur due to the rising of the injected anesthetics in the CSF. Once the operation has been completed, monitoring continues in the recovery room until the spinal anesthesia has receded significantly.
Side effects and complications
Relatively common side effects of spinal anesthesia are blood pressure fluctuations , cardiac arrhythmias , back pain , nausea and vomiting, as well as postoperative post-puncture headache and urinary retention . Due to the continuous monitoring, these problems are usually quickly recognized by the anesthetist and treated without consequences.
Serious complications such as severe circulatory disorders or permanent nerve damage from direct damage, infection, or bleeding are rare events. The frequency is difficult to determine; Problems are a lack of studies with a sufficient number of patients, imprecise and deviating (heterogeneous) definitions of the damage in these investigations as well as the delimitation of other possible damage mechanisms such as the surgical procedure itself, positioning, existing (possibly unknown) diseases or spontaneously occurring events (bleeding, infections ), which is often difficult to achieve.
Circulatory disorders
A drop in arterial blood pressure ( hypotension ) is the most common side effect of spinal anesthesia, affecting up to a third of patients. It is created by numbing the sympathetic nervous system ( sympathicolysis ) of the lower half of the body, which widens the vessels ( vasodilation ) and reduces the circulating blood volume and thus the return flow to the heart. The higher the spread of the spinal anesthesia, the more pronounced the hypotonic effect. It is sometimes accompanied by a slow heart rate ( bradycardia ) and nausea.
The decrease is particularly pronounced in patients with a lack of fluids, which is why electrolyte solutions are administered prophylactically as an infusion before spinal anesthesia is carried out in order to compensate for such a deficit. Blood loss, positioning maneuvers and releasing a congestion when the blood is empty also promote hypotension. Hypotension is treated with volume administration by infusion, by a slight head-down position ( Trendelenburg position , only slightly affects the spread of the local anesthetic up to about 10 °) and by administering medication, if necessary. Here are catecholamine derivatives as cafedrine / Theodrenalin (Akrinor) or less frequently norepinephrine used in bradycardia and atropine or Orciprenalin . While disorders of blood pressure or heart rate can usually be treated effectively, severe forms up to cardiac arrest rarely occur (approx. 3 / 10,000).
Post-spinal headache
→ Main article: Post-puncture headache
The post- puncture or post-spinal headache ( postdural puncture headache , PDPH) is one of the unpleasant side effects of spinal anesthesia, but usually has a good prognosis. A CSF loss syndrome through the perforation site of the hard meninges is postulated as the origin . Liquor escapes through this leak, with negative pressure developing in the CSF space if the loss exceeds the rate of new formation. A stretching of pain-sensitive structures of the brain (meninges, vessels, falx cerebri ), a compensatory widening of the vessels (vasodilation) and possibly increased intracranial pressure due to a reduced venous outflow of the cerebral vessels result in the development of headache. The syndrome was already mentioned in August Bier's description of spinal anesthesia (1899, see below).
The headache occurs in 0.5–18% of patients, depending on the spinal needle used , and usually begins on the second day after the puncture. The symptoms improve when lying down, while sitting and standing, shaking the head and increasing abdominal pressure, worsening the symptoms. The post-puncture headache can be accompanied by nausea, vomiting, dizziness, neck stiffness, back pain, sensitivity to light and noise, appearance of double vision and visual disturbances (due to irritation of the third , fourth and sixth cranial nerves ) as well as decreased hearing or tinnitus (due to irritation of the eighth cranial nerve ) .
Treatment is primarily conservative through bed rest, adequate fluid intake and pain medication . If these measures are unsuccessful, various invasive therapy methods are used; the epidural blood patch is the method of choice . Here, sterile blood from the patient is injected into the epidural space at the level of the puncture site. This compresses and closes the perforation of the meninges.
The most important measure for the prophylaxis of a post-puncture headache is the use of the thinnest possible puncture needles with an atraumatic tip (pencil point tip) , which have far lower rates of headache (0.5–1%) than needles with a larger diameter and cutting, oblique sharpened tip (e.g. Quincke needle ). The atraumatic tip of the Sprotte cannula introduced in 1979 was developed by the anesthetist and pain therapist Günter Sprotte (* 1945) in collaboration with the Pajunk company
Neurological Complications
In the case of damage to nerves, a distinction can be made between damage primarily caused by spinal anesthesia and damage developed secondarily. Mechanical injuries from the needle or toxic effects of the injected solutions are possible as primary damage mechanisms , as are secondary infections and bleeding with a space-occupying character (see below), which can cause damage through pressure on the nerves (compression).
Nerve damage that occurs after a surgical procedure is rarely caused by needle injuries from spinal anesthesia, but is often the result of positioning , surgery or independent factors such as previous illnesses. The incidence of damage to spinal nerves from spinal anesthesia is estimated at 3.8 / 10,000, a large part of which is reversible.
As transient neurological symptoms (TNS) is called symmetric, in the legs radiating back pain without sensory deficits, which typically begin within a few hours after the anesthesia and disappear without consequences within days. They are caused by the toxicity of local anesthetics and occur in around one percent of patients. However, if lidocaine is used, the rate is significantly higher.
The cause of the rarely occurring cauda equina syndrome (0.02–0.16 / 10,000) is also based on the neurotoxicity of the local anesthetics. Weakness of the lower extremities , problems with urination and bowel movements as well as sensitivity disorders in the genital area ( breeches anesthesia ) are clinical signs. This damage is often permanent.
Bleeding
Damage to blood vessels when the needle is advanced into the spinal canal can cause bleeding in the epidural and spinal spaces. However, space-occupying bruises ( hematomas ) only very rarely occur in this way; their frequency is estimated at 1: 220,000. Patients who suffer from coagulation disorders or who are taking anticoagulant medication have a slightly higher risk (approx. 1: 40,000). Clinically, a failure of the reflexes ( areflexia ), muscle weakness and sensory disturbances below the level of compression are in the foreground, typically after the effect of the spinal anesthesia has primarily subsided. Since bleeding close to the spinal cord can cause permanent nerve damage, an MRI scan must be performed to confirm the diagnosis in suspected cases . If a bleeding-related compression of the nerves is identified, surgical relief ( laminectomy ) must be performed immediately . To avoid bleeding, certain time intervals (see above) must be observed between the administration of anticoagulant drugs and punctures near the spinal cord.
Infections
Infectious complications after a single spinal anesthesia are very rare. Possible causes are the spread of germs from an existing infection or an introduction through a contaminated needle or insufficiently sterile work, whereby pathogens can penetrate the spinal and epidural spaces. Possible manifestations are inflammation of the meninges ( meningitis ) and the formation of an abscess (purulent mass) in the epidural space (between the dura and periosteum). Reliable figures on frequency are not available; While the risk for catheter procedures is estimated to vary widely from 1: 1000 to 1: 100,000, an occurrence after a single injection is a rarity. A differentiation from spontaneously occurring abscesses (0.2–1.2: 10,000) is difficult. The most common pathogens are staphylococci , the occurrence of which in the skin flora shows the importance of thorough disinfection of the puncture site and strictly sterile execution of the puncture.
Meningitis typically manifests itself after 24–48 hours with fever, stiff neck ( meningism ), headache and photophobia . If there is any suspicion, a diagnostic lumbar puncture must be carried out in order to determine the pathogen by means of a CSF examination and to be able to treat it with targeted antibiotic therapy. Aseptic meningitis is a special form in which no pathogen detection is possible.
A serious complication is the formation of an abscess of the epidural space. Symptoms are variable and include fever, back pain, and neurological failures. The pioneering diagnostics include, in particular, imaging methods (MRT). Antibiotics are used therapeutically; in most cases, early surgical relief is necessary. Serious nerve damage remains in a third of the cases and slight nerve damage in a further third. Mortality from developing sepsis is around 10-15%.
Other side effects
Nausea and vomiting occur in up to 15% of spinal anesthesia. Back pain is reported by around 10% of patients, and it is difficult to assign the cause to anesthesia procedure, surgery or positioning. A urinary retention occurs in 1.5-3% of patients, the surgery no indwelling catheter into the bladder get engaged. The cause is an imbalance between the inhibiting influence of the sympathetic and the promoting influence of the parasympathetic on emptying the bladder. Sterile, single-use catheterization may be required for treatment .
A serious side effect is spinal anesthesia that ascends too high, as can occur if the medication is inadvertently overdosed. If these are distributed throughout the spinal space, one speaks of total spinal anesthesia . Loss of consciousness , respiratory and circulatory arrest can result and must be treated with endotracheal intubation and ventilation , catecholamine therapy and, if necessary, with resuscitation measures . With adequate therapy, complete regression ( restitutio ad integrum ) is usually possible.
A technical failure of the spinal anesthesia (impossibility to perform, needle bending, very rarely needle breakage) is directly dependent on the diameter of the spinal needle. With standard needles ( 25 gauge ) this rate is less than five percent, but increases with thinner needles. Since a larger needle size is associated with a higher rate of post-puncture headache, needle selection is a compromise.
Historical aspects
The first punctures of the lumbar liquor space were performed in 1891 by Heinrich Irenaeus Quincke in Kiel , but for the diagnostic removal of liquor. To this end, he developed a beveled puncture needle (Quincke needle) .
On August 24, 1898, the surgeon August Bier (1861–1949) and his assistant August Hildebrandt (1868–1954) also successfully performed spinal anesthesia in a mutual attempt in Kiel. By injecting cocaine, "a strong blow with an iron hammer against the shin" and "strong pressure and pulling on the testicle" were no longer perceived as painful. As a result, both of them developed a very pronounced post-spinal headache with nausea and vomiting.
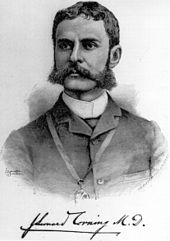
The American James Leonard Corning had already made similar attempts in 1885 and injected cocaine into structures near the spinal cord. It is controversial whether spinal anesthesia was successful or whether the substances were only applied to the ligament structures. Following the publication of August Bier, controversy arose over the first successful anesthetic procedure of its kind, which both Bier and Corning claimed for themselves. As a result, Bier fell out with his assistant Hildebrandt, who was dissatisfied because Bier had not listed him as a co-author. Today, Corning is credited with creating the experimental and theoretical prerequisites for spinal anesthesia, and Bier with the successful application and subsequent establishment of the method in the clinic. The first Americans to use spinal anesthesia include F. Dudley Tait, Guido E. Caglieri and the vascular surgeon Rudolph Matas (1860–1957), who performed it in 1899 with the help of Felix A. Larue, Hermann B. Gessner and Carroll Allen . Physicians as Pierre Marie , Georges Charles Guillain and Charles Achard applied the subarachnoid injection of cocaine also used to treat nerve pain in the lumbar region and legs as in sciatica or lumbago at (lumbago).
At the beginning of the 20th century, spinal anesthesia was established in obstetrics. In the 1930s, however, publications on deaths from spinal anesthesia for caesarean section brought this application into disrepute; Instead, the pregnant women were encouraged to use “natural birth procedures” and “psychoprophylaxis”. Due to the neglect of pain therapy during childbirth, this period is also known as the “dark years of obstetric anesthesia”. It was not until the 1950s that this perspective changed again. Today, spinal anesthesia is a standard procedure when performing a caesarean section.
In 1951 Whitacre and Hart developed pencil point cannulas . Their introduction into clinical practice led to a significant reduction in the rate of postspinal headache that had previously occurred in the majority of patients.
The first continuous spinal anesthesia with the spinal needle left in place during the operation at the puncture site was performed as early as 1907 by the surgeon Dean . However, the establishment of this procedure through the development of sufficiently thin catheters, through which acceptably low rates of postspinal headache could be achieved, did not take place until the second half of the 20th century.
literature
- D. Jankovic: Regional blockades and infiltration therapy. 3. Edition. Abw Wissenschaftsverlag, 2003, ISBN 3-936072-16-7 .
- R. Rossaint, C. Werner, B. Zwißler: The anesthesiology: General and special anesthesiology, pain therapy and intensive medicine. 2nd Edition. Springer, 2008, ISBN 978-3-540-76301-7 .
- F. Gerheuser, D. Craß: Spinal anesthesia. In: Anaesthesiologist. 2005 Dec; 54 (12), pp. 1245-1267. Review. PMID 16317479 .
- Michael Heck, Michael Fresenius: Anesthesiology revision course. 5th edition. Springer, 2007, ISBN 978-3-540-46575-1 .
Individual evidence
- ↑ Rossaint et al. a. 2008, pp. 620-624; Jankovic 2003, pp. 263-271; Gerheuser and Craß 2005, pp. 1246-1248.
- ↑ F. Gerheuser, A. Roth: epidural. In: Anaesthesiologist. Volume 56, No. 5, May 2007, pp. 499-523, doi: 10.1007 / s00101-007-1181-1 , PMID 17431551 .
- ↑ Diagnostic CSF puncture ( Memento of the original dated December 15, 2007 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. - Guideline of the German Society for Neurology, 2005.
- ^ NM Denny, DE Selander: Continuous spinal anesthesia. In: Br J Anaesth. 1998 Oct; 81 (4), pp. 590-597. PMID 9924237
- ↑ B. Neruda: Development and current status of the combined spinal-epidural anesthesia. In: Anasthesiol Intensivmed Emergency Med Schmerzther. 2005 Aug; 40 (8), pp. 459-468. PMID 16078156
- ↑ a b Rossaint u. a. 2008, p. 636f.
- ↑ a b G. Hocking, JA Wildsmith: Intrathecal drug spread. In: Br J Anaesth. 2004 Oct; 93 (4), pp. 568-578. PMID 15220175
- ↑ D. Zaric, C. Christiansen, NL Pace, Y. Punjasawadwong: Transient neurologic symptoms (TNS) following spinal anesthesia with lidocaine versus other local anesthetics. In: Cochrane Database Syst Rev. 2005 Oct 19; (4), S. CD003006. PMID 16235310
- ↑ Rossaint et al. a. 2008, p. 639f.
- ↑ MA Chaney: Side effects of intrathecal and epidural opioids. In: Can J Anaesth. 1995 Oct; 42 (10), pp. 891-903. PMID 8706199
- ↑ Dorothee H. Bremerich: Comments on the letter to the editor Is the intrathecal mixture of bupivacaine + sufentanil + morphine obsolete for her SPA during cesarean section? In: Anaesthesiology & Intensive Care Medicine. Volume 60, 2019, pp. 578–581, here: p. 580, Table 1: Internationally required monitoring intervals after application of morphine near the spinal cord .
- ↑ N. Elia, X. Culebras, C. Mazza, E. Schiffer, MR Tramèr: Clonidine as an adjuvant to intrathecal local anesthetics for surgery: systematic review of randomized trials. In: Reg Anesth Pain Med. 2008 Mar-Apr; 33 (2), pp. 159-167. PMID 18299097
- ↑ K. Govindan, R. Krishnan, MP Kaufman, R. Michael, RJ Fogler, J. Gintautas: Intrathecal ketamine in surgeries for lower abdomen and lower extremities. In: Proc West Pharmacol Soc. 2001; 44, pp. 197-199. PMID 11793982
- ↑ Gerheuser and Craß 2005, p. 1257.
- ↑ a b Jankovic u. a. 2003, p. 272f.
- ^ V. Hempel: Spinal anesthesia for caesarean section. In: Anasthesiol Intensivmed Emergency Med Schmerzther. 2001 Jan; 36 (1), pp. 57-60. PMID 11227314
- ↑ A. Rodgers, N. Walker, S. Schug, A. McKee, H. Kehlet, A. van Zundert, D. Sage, M. Futter, G. Saville, T. Clark, S. MacMahon: Reduction of postoperative mortality and morbidity with epidural or spinal anesthesia: results from overview of randomized trials. In: BMJ. 2000 Dec 16; 321 (7275), p. 1493. PMID 11118174
- ↑ E. Tziavrangos, SA Schug: Regional anesthesia and perioperative outcome. In: Curr Opin Anaesthesiol. 2006 Oct; 19 (5), pp. 521-525. PMID 16960485
- ^ F. Wappler, K. Bangert: Perioperative management in cardiac risk patients. In: Anasthesiol Intensivmed Emergency Med Schmerzther. Volume 40, No. 5, May 2005, pp. 284-291. PMID 15902608 .
- ↑ a b Rossaint u. a. 2008, p. 631f.
- ^ A b W. Gogarten, H. Van Aken, J. Büttner, H. Riess, H. Wulf, H. Bürkle: Regional anesthesia close to the spinal cord and thromboembolism prophylaxis / antithrombotic medication . ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice. (PDF; 216 kB) 2nd revised recommendation of the German Society for Anesthesiology and Intensive Care Medicine. In: Anästh Intensivmed. 2007; 48, pp. S109-S124
- ↑ Implementation of analgesia and anesthesia procedures in obstetrics . 2. Revised recommendations of the German Society for Anesthesiology and Intensive Care Medicine and the Professional Association of German Anesthetists in cooperation with the German Society for Gynecology and Obstetrics. In: Anästh. Intensivmed. , 50, 2009, pp. S490-S495
- ↑ Cross-sectional guidelines (BÄK) on therapy with blood components and plasma derivatives. 4th revised and updated edition 2014, Deutsches Ärzteblatt, vol. 112, issue 6, February 6, 2015
- ^ Wiebke Gogarten, Hugo K Van Aken: Perioperative thrombosis prophylaxis - platelet aggregation inhibitors - importance for anesthesia. In: AINS - Anesthesiology • Intensive Care Medicine • Emergency Medicine • Pain Therapy. Issue 04, April 2012, pp. 242-254, doi: 10.1055 / s-002-23167 .
- ↑ SA Kozek-Langenecker, D. Fries, M. Gütl, N. Hofmann, P. Innerhofer, W. Kneifl, L. Neuner, P. Perger, T. Pernerstorfer, G. Pfanner u. a .: Locoregional anesthesia with anticoagulant medication. Recommendations of the Perioperative Coagulation Working Group (AGPG) of the Austrian Society for Anaesthesiology and Intensive Care Medicine (ÖGARI). In: The anesthesiologist. Volume 54, Number 5 (2005), pp. 476-484, doi: 10.1007 / s00101-005-0827-0 .
- ↑ Jankovic 2003, pp. 273-278; Rossaint et al. a. 2008, pp. 634-642; Gerheuser and Craß 2005, p. 1253 f.
- ↑ a b Rossaint u. a. 2008, p. 643f; Jankovic 2003, pp. 285f.
- ^ A b c R. Brull, CJ McCartney, VW Chan, H. El-Beheiry: Neurological complications after regional anesthesia: contemporary estimates of risk. In: Anesth Analg. 2007 Apr; 104 (4), pp. 965-974. Review: PMID 17377115
- ↑ EM Pogatzki-Zahn, M. Wenk, H. Wassmann, WL Heindel, H. Van Aken: Severe complications from regional analgesic procedures - symptoms, diagnosis and therapy. In: Anasthesiol Intensivmed Emergency Med Schmerzther. 2007 Jan; 42 (1), pp. 42-52. Review: PMID 17253336
- ↑ Jankovic 2003, p. 285.
- ↑ SL Kopp, TT Horlocker, ME Warner, JR Hebl, CA Vachon, DR Schroeder, AB Gould Jr, J. Sprung: Cardiac arrest during neuraxial anesthesia: frequency and predisposing factors associated with survival. In: Anesth Analg. 2005 Mar; 100 (3), pp. 855-865, PMID 15728079
- ↑ P. Kessler, H. Wulf: Duraperforation - post-puncture headache - prophylaxis and therapy options. In: Anästhesiol Intensivmed Emergency Med Schmerzther. 2008; 43, pp. 346-353. PMID 18464211 , doi: 10.1055 / s-2008-1079107 .
- ↑ DK Turnbull, DB Shepherd: Post-dural puncture headache: pathogenesis, prevention and treatment. In: Br J Anaesth. 2003 Nov; 91 (5), pp. 718-729. doi: 10.1093 / bja / aeg231 , PMID 14570796 .
- ↑ 40 years of Sprotte®. A success story for four decades. In: Anaesthesiology & Intensive Care Medicine. Volume 61, January 2020, spine.
- ↑ a b c d H. Ohnesorge, H. Beck: Neurological complications after regional anesthesia. In: Anasthesiol Intensivmed Emergency Med Schmerzther. 2003 Jul; 38 (7), pp. 472-475, PMID 12822119 .
- ↑ LH Eberhart, AM Morin, P. Kranke, G. Geldner, H. Wulf: Transient neurological symptoms after spinal anesthesia: A quantitative systematic overview (meta-analysis) of randomized controlled trials. In: Anaesthesiologist. 2002 Jul; 51 (7), pp. 539-546. PMID 12243039
- ^ D. Zaric, C. Christiansen, NL Pace, Y. Punjasawadwong: Transient neurologic symptoms after spinal anesthesia with lidocaine versus other local anesthetics: a systematic review of randomized, controlled trials. In: Anesth Analg. 2005 Jun; 100 (6), pp. 1811-1816. PMID 15920219
- ↑ Rossaint et al. a. 2008, pp. 627-630.
- ^ S. Grewal, G. Hocking, JA Wildsmith: Epidural abscesses. In: Br J Anaesth. 2006 Mar; 96 (3), pp. 292-302. PMID 16431882 .
- ↑ Rossaint et al. a. 2008, pp. 625-627, p. 648.
- ↑ Robert Schmidt: Physiology of humans with pathophysiology; with 85 tables; with removable revision course . Springer-Medizin-Verl, Heidelberg 2010, ISBN 978-3-642-01650-9 .
- ↑ Gerheuser and Craß 2005, p. 1266.
- ^ HI Quincke: The lumbar puncture of the hydrocephalus. In: Berl Med Wochenschr. 1891; 28, pp. 929-933.
- ↑ A. Bier: Experiments on the cocainization of the spinal cord. In: Dtsch Z Chir. (1899); 51, pp. 361-368.
- ^ A b Peter Oehme: Spinal cord anesthesia with cocaine: The priority controversy on lumbar anesthesia. In: Dtsch Arztebl. 1998; 95 (41), pp. A-2556-A-2558.
- ^ JL Corning: Spinal anesthesia and local medication of the cord. In: New York State Med J. (1885); 42, p. 483.
- ↑ Rudolph Matas, Felix A. Larue, Hermann B. Gessner, Carroll Allen: Intraspinal Cocainization. In: Journal of the American Medical Association. Volume 33, (December 30) 1899, p. 1659 ( Medical News ).
- ^ Merlin D. Larson: Tait and Caglieri: The First Spinal Anesthetic in America .
- ^ Albert Faulconer, Thomas Edward Keys: Rudolph Matas. In: Foundations of Anesthesiology. Charles C Thomas, Springfield (Illinois) 1965, p. 858.
- ^ Jean-Athanase Sicard: The Extradural Injection of Agents by the Sacrococcygeal Route. (Translation of Les injections médicamenteuses extradurales par voie sacrococcygienne. In: Comptes rendus hebdomadaires des séances et mémoires de la Société de biologie. Volume 53, (April 20) 1901, pp. 396-398.) In: Albert Faulconer, Thomas Edward Keys: Foundations of Anesthesiology. Charles C Thomas, Springfield (Illinois) 1965, pp. 921-923, here: 921 f.
- ^ W. Gogarten, H. Van Aken: A century of regional analgesia in obstetrics. In: Anesth Analg. 2000 Oct, 91 (4), pp. 773-775. PMID 11004024
- ^ JR Hart, RJ Whitacre: Pencil-point needle in prevention of postspinal headache. In: J Am Med Assoc. 1951 Oct 13; 147 (7), pp. 657-658, PMID 14873528
- ↑ HP Dean: Discussion on the Relative Value of Inhalation and Injection Methods of Inducing Anesthesia. In: Br Med J. 1907; 5, pp. 869-877.