Sleep apnea syndrome
| Classification according to ICD-10 | |
|---|---|
| G47.3 | Sleep apnea |
| G47.30 | Central sleep apnea syndrome |
| G47.31 | Obstructive Sleep Apnea Syndrome |
| G47.38 | Other sleep apnea |
| G47.39 | Sleep apnea, unspecified |
| ICD-10 online (WHO version 2019) | |
The sleep apnea syndrome ( SAS ) is a complaint image obtained by periodic disordered breathing (apnea ( apnea ) and / or reducing ventilation of the lung (alveolar hypoventilation)) is caused during sleep. It is characterized by pronounced daytime sleepiness up to the need to fall asleep ( microsleep ) as well as a number of other symptoms and secondary diseases.
The respiratory arrests lead to a reduced oxygen supply with a simultaneous increase in the carbon dioxide content of the blood and as a result to repeated wake-up reactions (alarm reaction of the body). Most wake-up reactions do not lead to conscious waking up, but only to increased body functions, for example an accelerated pulse and the repeated release of stress hormones, which are to be assessed as an endogenous emergency survival program. This also affects the normal sequence of sleep phases, so that in addition to the somatic stressors, the recovery and regeneration function of night sleep is sometimes considerably reduced. Since these reactions still take place when they are asleep, they are usually not consciously perceived by those affected. The consequence of sleep apnea is chronic physical stress and non-restful sleep, which usually leads to the typical, pronounced daytime sleepiness with its further risks.
In the sleep medicine include the various forms of sleep apnea syndrome according to the classification system for sleep disorders ( International Classification of Sleep Disorders (ICSD)) to the "sleep disordered breathing".
The prevalence (frequency) of sleep apnea syndrome with an apnea-hypopnea index (AHI) of more than 15 is 9% in men and 4% in women, according to new studies.
pronunciation
The correct pronunciation is three-syllable "A-pno-e" ([ aˈpnoːə ]) due to the origin of ancient Greek ἄπνοια apnoia "non-breathing", also compare with apnea diving .
Forms and causes
The breathing is usually an involuntary process. The breathing stimulus is not - as is often assumed - triggered by a falling oxygen content (O 2 ) in the blood or tissue, but an increasing carbon dioxide (CO 2 ) content in the blood is the strongest breathing stimulus. If the partial pressure of the oxygen falls below an individual limit, people pass out . During an only temporary respiratory standstill, an apnea, the CO 2 partial pressure in the blood rises significantly, so that a so-called wake-up reaction is triggered before a fainting occurs .
A distinction is made between obstructive and central apneas. If both forms occur in a patient, one speaks of mixed apnea syndromes.
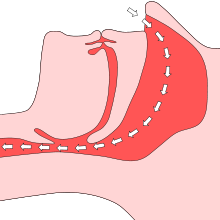
The most frequent, occurring at about 5-10% of the population is the form o bstruktive S chlaf a pnoe- S yndrom (OSAS). The direct cause of OSAS is a strong relaxation of the ring-shaped muscles around the upper airways during sleep. As a result, the nasal pharynx or the pharynx are no longer able to withstand the negative pressure created in the lungs and bronchi when inhaled. The upper part of the airways collapses and an obstruction occurs. Abnormal respiratory arrests last longer than ten seconds, as a result of which arterial oxygen saturation or the oxygen content of the blood falls ( hypoxemia ). This leads firstly to an insufficient supply of the tissues in the body and in the brain and secondly to an increased CO 2 level in the blood. As a result of the frustrating inhalation movement ( Müller maneuver ) and the rising CO 2 level, the body wakes up (“micro- arousal ”), which causes breathing to start again. Usually the patient does not remember this reaction. The physiological structure of sleep is destroyed and the recovery function is hindered. If the upper part of the airways only partially collapses, there is a short-term reduction in the respiratory volume , the so-called hypopneas . In the end, the oxygen content in the blood also drops , but not as much as in apnea. The number of apneas and hypopneas per hour is shown by the so-called AHI ( Apnea-Hypopnea Index ). When the upper respiratory tract collapses, many sufferers make snoring noises, so that many of the OSAS patients snore heavily. There is therefore an urgent suspicion of OSAS in those who snore and are very tired during the day. Snoring (rhonchopathy) alone and occasional, short breathing pauses are not harmful to health. In Germany, 1–2% of women and 2–4% of middle-aged men are affected by OSAS. Often the OSAS also triggers central breathing pauses, so that the mixed form is also very common.
The upper airway resistance syndrome (UARS) is a sub-form of sleep-disordered breathing, wherein the muscle tone in the upper respiratory tract is still sufficiently high to keep open a portion of the lumen of the airways. Increased wake-up reactions occur due to increased respiratory effort, even without a significant decrease in oxygen, and also arousals.
The pure such connotations of core S chlaf a pnoe- S yndrom (ZSAS) is rare. Damage in the central nervous system (CNS), especially in the respiratory center , causes the respiratory muscles to be insufficiently controlled - the brain "forgets" to breathe. Central apnea is usually hereditary, but can also result from neurological damage. Central sleep apnea is divided into five types: idiopathic central apnea, Cheyne-Stokes breathing , reduced breathing due to altitude sickness , disease-related and drug-related apnea.
OSAS has no single cause. The following risk factors can promote OSAS:
- Obesity ( overweight )
- possibly also an obstruction of nasal breathing due to polyps or curvature of the nasal septum or rhinitis vasomotorica
- enlarged tonsils (especially in children)
- constitutional relaxation of the pharynx muscles , disposition
- Alcohol consumption , sleeping pills, nicotine, ecstasy
- Dolichofacial face type: in the lateral cephalometric image of an adult, a large angle of the lower jaw can be seen - as a result, the pharyngeal muscles lie far against the back of the pharynx, the lumen is narrowed
- Congenital malformations and malpositions of the lower jaw ( Pierre Robin sequence , Goldenhar syndrome , craniometaphyseal dysplasia )
- Enlargement of the soft tissues (e.g. tongue) caused by acromegaly
- Connective tissue diseases such as B. Marfan's syndrome
The ZSAS can also benefit from the following factors:
- Heart problems: heart failure , stroke, or atrial fibrillation
- Brain tumor
- Life at great heights
- Respiratory drugs
Sleep apnea in children
Sleep apnea syndrome rarely occurs in infants and young children, but a single occurrence can lead to a life-threatening situation. In premature babies or nine-month babies who were born under difficult conditions, sleep apnea occurs most likely. It is believed that the brain is not yet fully transmitting the signals to the lungs . In infants, a distinction must be made between so-called periodic breathing, a normal phenomenon, and sleep apnea. With periodic breathing, breathing can stop for about ten seconds and then resume regularly. In babies , breathing is recorded with an apnea monitor. All breathing pauses that last too long are recorded and an alarm is triggered.
Breathing irregularly occurs in many older children, and it is often short and not life threatening. Usually polyps or enlarged tonsils are responsible for apnea-like sleep conditions in older children.
Symptoms
The relatives of OSAS patients usually report loud snoring , interrupted by breathing pauses, which are ended with a heavy, sighing breath or a snoring sound. Not every snorer suffers from OSAS, and not every OSAS patient is actually noticed by snoring. The described narrowing in the upper airways can in individual cases lead to an immediate closure so that no more snoring noises can arise.
Other symptoms of obstructive sleep apnea syndrome include:
- Apnea lasting at least 10 seconds to minutes
- Difficulty sleeping through the night
- Daytime sleepiness, tendency to fall asleep during the day
- Headache on awakening
- Dizziness , especially after getting up
- Dry mouth on awakening
- night sweats
- Nocturia (increased urination during sleep / urination at night)
- Microsleep attacks / imperative need to sleep, sometimes without warning signals
- Concentration disorders up to memory disorders
- depressive mood
- Impotence, erectile dysfunction
- restless sleep
consequences
As a consequence of untreated OSAS, other chronic health disorders usually occur, namely cardiovascular diseases such as high blood pressure , right heart failure , heart attacks and strokes . A sudden cardiac death can occur in untreated OSAS with increased probability. Are also described depression , brain damage and the increased occurrence of stress disease control such as stomach ulcer , tinnitus and sudden hearing loss . Diabetes mellitus, type 2 , has been associated with OSAS with increasing frequency since the beginning of 2002. There is a linear relationship between the apnea-hypopnea index (AHI) and insulin resistance. The more pauses in breathing per hour of sleep, the higher the blood sugar . After an initiated nCPAP therapy , the nocturnal generation of sugar ( gluconeogenesis ) can be significantly reduced and the morning blood sugar levels can drop. Patients whose OSAS was improved with treatment report reduced migraine attacks .
According to a recent study, the SAS is strongly associated with the occurrence of heart diseases that require a pacemaker .
Recently it has been increasingly pointed out that a sleep apnea patient who is tired or pathologically unable to concentrate is not allowed to drive a vehicle, in particular with passenger transport. Depending on the legal situation, there may even be criminal liability . Legal norms are here z. B. the driving license ordinance , the professional association investigation principle G25 and the guidelines of the Association of German Transport Companies . Many serious traffic accidents are likely the result of untreated sleep apnea. That is why early detection examinations are required for professional drivers . Fitness to drive is usually fully restored two to four weeks after starting regular nCPAP therapy. Regular follow-up examinations - including therapy acceptance - are necessary. Currently, only a few occupational health services of transport companies such as the Wuppertaler Stadtwerke examine their employees for the presence of sleep-related breathing disorders such as sleep apnea. If necessary, the nCPAP respiratory therapy devices must also be operated using the on-board network when the car or truck is idle.
In Germany, sleep apnea syndrome is also recognized as a disability by the pension offices:
- without the need for ventilation therapy (nCPAP, BiPAP) 0-10 degree of disability (GdB)
- with the need for ventilation therapy (nCPAP, BiPAP) 20 GdB
- if therapy / ventilation therapy cannot be carried out, at least 50 GdB
research
As part of a preliminary study by the American Academy of Neurology in 2019, researchers at the Mayo Clinic in Rochester, Minnesota, found that sleep apnea may be correlated with higher levels of tau protein , a biomarker in the brain associated with Alzheimer's disease in Is associated. The researchers recruited 288 older participants aged 65 and over for the study.
diagnosis
The typical history (obstructive snoring, breathing pauses and lack of restful night sleep) as well as information on sleep hygiene are important for the diagnosis . The diagnostics are initiated by a sleep diagnostic screening (so-called non-laboratory monitoring ), which is carried out mainly by ENT specialists or pulmonologists after appropriate training and approval . The examination with such non-laboratory monitoring systems (NLMS) is carried out by recording respiratory flow (nasal flow), breathing sounds, oxygen saturation in the blood by means of a pulse oximeter , heart rate, breathing movement of the chest and abdomen as well as the body position ( cardiorespiratory polygraphy ) during sleep At the patient's home. Various compact devices are available on the market for this purpose. Sleep apnea is likely if, in addition to the clinical symptoms in the polygraph, with a recording time of at least six hours, an average of more than five apnea / hypopnea phases per hour lasting over 10 seconds (pathological apnea / hypopnea index AHI:> 5) can be detected with the characteristic episodic drop in oxygen saturation of the blood. An AHI of 6 to 14 is classified as light / mild sleep apnea, an AHI of 15 to 30 as medium sleep apnea and an AHI of over 30 as severe sleep apnea.
In the case of an abnormal screening, the patient is referred to a sleep laboratory . There the need for treatment is further clarified with a polysomnography or a treatment is initiated and checked for effectiveness. In polysomnography, in addition to the parameters of polygraphy, an electroencephalogram (EEG), electrooculography (EOG), electromyography (EMG) in the area of the chin and leg muscles and an EKG are recorded and the blood pressure curve, in some cases also intrathoracic pressure fluctuations, continuously registered. During the nightly examination, the sleep behavior is documented with a video recording. The polysomnography shows the influence of the reduced oxygen supply, which manifests itself in the EEG as “sleep fragmentation”. Due to the lack of oxygen, which is repeated as a result of the breathing pauses, there are constant waking reactions (arousals) , so that the fractionation of sleep (compared to normal "sleep architecture") results in a pathological reduction in deep sleep and dream sleep phases .
With full polysomnography, the RDI can also be determined in addition to the AHI. The RDI, R espiratory D isturbance I ndex, involves the respiratory events on the occupied EEG sleep time and not just on the "bed time".
treatment
Conservative therapy
Depending on the severity and cause, various methods of treatment are recommended, such as weight reduction , abstaining from alcohol and nicotine, and possibly surgical treatment of airway obstruction. Strengthening the muscles of the mouth and throat can also bring about an improvement; there have been positive reports about the effect of regular music making with wind instruments, especially with a didgeridoo . Recent studies show that double-reed instruments also alleviate symptoms, while other musical instruments have no effect.
A treatment of OSAS is the CPAP therapy by CPAP flow generators ( C ontinuous P ositive A irway P ressure). These devices have a blower that is connected to an nCPAP mask via a hose, which is pressed onto the face using headbands around the nose (or around the mouth and nose). With the help of these masks, a slight overpressure of 5 to 20 millibars is generated in the airways during sleep . This prevents the airways from collapsing and thus prevents apneas and hypopneas. At the same time, snoring is prevented. This therapy is also called “pneumatic splinting” of the upper airways. There are several types of such masks. A distinction is made between “direct nasal”, “oral”, “nasal” and “full face masks”. After an acclimatization phase, most users report a significantly better quality of sleep and a decrease or disappearance of OSAS symptoms . In addition to alleviating the symptoms of OSAS, CPAP therapy can also help alleviate drug-resistant hypertension, which often occurs in connection with OSAS.
If CPAP therapy appears to be too strenuous for the patient, for example because of the counter pressure when exhaling, one usually switches to BIPAP ventilation . As a rule, the therapy must be used for life. Withdrawal of therapy may cause symptoms to return. Sleep becomes restful if the therapy is carried out regularly and constantly. Sometimes when the nasal mucous membrane dries out, it is necessary to prescribe a warm humidifier for the air you breathe. The CPAP devices are set in the sleep laboratory to the individually necessary ventilation pressure. The pressure can be checked and adjusted in sleep laboratories, as this can change in the course of the therapy. Another pressure may be required, for example, if the patient has lost or gained weight. Outpatient settings and checks are also possible. Lately, health insurances have often asked for proof of use of more than four hours per night if they are to continue paying for the treatment. For this purpose, the respiratory therapy device records the period of use on a memory card.
The vigilance-increasing drug Modafinil can be used if daytime sleepiness persists under CPAP ventilation , but is no longer approved for this indication in Germany (only for narcolepsy), as it very often causes severe side effects such as headaches, nausea, dizziness and diarrhea. The use of theophylline , which increases the central respiratory drive , is u. a. obsolete due to cardiac side effects.
Mandibular protrusion splint
The intra-oral mandibular protrusion splint has demonstrated its effectiveness in patients with mild to moderate obstructive sleep apnea syndrome . These are adjustable splint systems that are individually manufactured after an impression of the teeth, manufactured using laboratory technology. Wearing it reduces the constriction of the pharynx, the airways are kept open mechanically during sleep and the airway resistance decreases. The procedure is also used instead of CPAP in the case of intolerance or insufficient therapy compliance. Meta-analyzes have shown that protrusion splints lower blood pressure as much as CPAP ventilation and also effectively treat daytime sleepiness.
Operative therapy
CPAP is the most widely used therapy for sleep apnea syndrome and the internationally recognized "gold standard", but it is not a long-term therapy that can be carried out for all patients. There are therefore surgical treatment options for obstructive sleep apnea, especially in the case of intolerance to conservative therapies. A sensible goal of surgical interventions can be to improve nasal air passage to improve CPAP compliance; another starting point is unusually large palatine tonsils and adenoids . Surgical alternatives with interventions in the neck area have not caught on.
Uvulopalatopharyngoplasty
The Uvulopalatopharyngoplasty (UPPP) is surgery for the reduction and streamlining of the soft palate. This operation removes fat and connective tissue in the throat area that could block the airways during sleep. This includes parts of the soft palate muscles , the uvula (suppository) and the base of the tongue .
Maxillomandibular surgery
When bimaxillary (Operation English Maxillomandibular Advancement ), the physical causes of obstructive sleep apnea, which is too small or too far past the jaw and base of the tongue associated with it, which constricts the upper airways treated. During this procedure, the upper and lower jaws are moved forward to permanently widen the upper airways. According to guidelines for the treatment of breathing-related sleep disorders, a forward displacement of both jaws of at least 10 mm is necessary in order to achieve the success rate of cure sleep apnea (AHI ≤ 5) with a probability of over 90%. A distinction is made between the usual bimaxillary advancement and the bimaxillary advancement with CounterClockwise rotation. In the operation with simultaneous rotation (counterclockwise), the airways are widened significantly more than in pure bimaxillary advancement. The aim of the bimaxillary operation is to increase the oxygen concentration in the arterial blood and to improve the quality of sleep.
Bimaxillary operations are performed by specialized oral, maxillofacial and facial surgeons or by oral surgeons. In general, the risks of such an intervention, as with any surgical intervention, depend on the surgeon's experience with this operation, and risks such as wound healing disorders, infection, vascular and especially nerve injuries (especially the mandibular nerve running in the lower jaw ) and bleeding must be taken into account , about which each patient must be informed individually. Special mention should be made of the mostly reversible numbness in the area of the lower lip and the occurrence of disorders of the tooth position. Extensive swelling can occur immediately postoperatively, which disappears after about one to two weeks. Operation-related pain is minor. After the procedure, the patient should not chew for about 3–4 weeks and should only consume liquid and pureed food.
As the jaw moves forward, the shape of the face changes. Therefore, extensive information and advice from an experienced specialist is recommended in advance in order to achieve an aesthetically pleasing result in addition to the medically successful result. Overweight patients, patients with heart disease or diabetes also have an increased risk of surgery, which affects many patients with sleep apnea. Therefore, according to the guidelines valid in Germany, a safe therapy with air (CPAP) with a sufficient time window to get used to and with the support of experienced sleep specialists should always be tried, which then succeeds in most cases.
Stanford Protocol
An operation according to the Stanford protocol is much larger and consists of two separate operations. The first surgery is soft tissue surgery that includes tonsillectomy and uvulopalatopharyngoplasty. If there is still residual sleep apnea, the second operation, which consists of a maxillomandibular dysgnathia operation, takes place.
Hypoglossal stimulation
Another starting point is stimulation therapy . By stimulating the hypoglossal nerve , nocturnal apneas can be prevented by increasing the tone of the tongue muscles. The entire right-sided tongue musculature can be stimulated in synchronism with breathing during inhalation or continuously alternating different parts of the right-sided tongue musculature during inhalation and exhalation. Since both systems have been in use in Europe since 2013, respiration-synchronized stimulation has also been used in the USA since it was approved by the FDA in April 2014.
Surgical interventions are carried out by appropriately specialized oral surgeons and / or ENT specialists.
In life-threatening situations or when all other treatment methods fail, a tracheotomy (incision in the windpipe) is also performed. This drastic intervention always works because it bypasses the obstruction of the upper airway. In rare cases, a permanent tube is inserted into the patient's windpipe through which they can breathe while they sleep.
Alternative therapies
Numerous companies also offer "anti-snoring masks", nose clips, electrical warning devices, meditation courses, magnetic field mats, essential oils etc. for self-treatment. These products and methods have not yet been proven to be effective, and in some cases even interfere with night sleep. They also prevent or delay the start of effective sleep apnea treatments.
Another alternative is transcutaneous electrical stimulation of the suprahyoid muscles, which leads to an enlargement of the lumen in the pharynx. The tongue muscle training (ZMT ® ) must be carried out twice a day for two months. However, this method offers only limited success, also only in the case of mild sleep apnea syndrome, and can therefore not generally be viewed as an alternative to CPAP therapy.
No drugs are currently approved for the treatment of obstructive sleep apnea and there are no phase III studies in this area . However, a meta-analysis of seven drugs indicated a potential treatment success with acetazolamide .
Retired from the Bundeswehr
The sleep apnea syndrome is listed in health number 44 (lungs and mediastinum) of the central service regulation (ZDv) 46/1 :
- A proven sleep apnea syndrome with reduced physical and mental performance with the necessity of apparatus-based respiratory therapy is classified as grade VI, which leads to retirement.
- A proven sleep apnea syndrome without significant impairment of physical and mental performance leads to gradation IV, this has also led to a T5 (retirement) since October 1, 2004 following a change in the service regulations. Before that, this led to a T3 (usable with restrictions in basic training and for certain activities).
See Annex 3/46 of Central Service Regulation 46/1 of the Federal Ministry of Defense.
See also
literature
- Peter Spork : The snore book. Causes, risks, antidotes. Rowohlt Taschenbuch Verlag, Reinbek 2007, ISBN 978-3-499-62207-6 .
- Hans-Werner Gessmann : The tongue muscle training - an alternative treatment for sleep apnea and snoring. Publishing house of the Psychotherapeutic Institute Bergerhausen, Duisburg 2001, ISBN 3-928524-43-7 .
- Peter Hannemann: Sleep apnea syndrome and snoring. Causes, Symptoms, Successful Treatment. Jopp bei Oesch, Zurich 2000, ISBN 3-89698-113-7 .
- Jürgen Schäfer: Snoring, Sleep Apnea and Upper Airways. Thieme Verlag, Stuttgart 1996, ISBN 3-13-102111-X .
Web links
- S3 guideline (as of 2017) Non-restful sleep / sleep disorders - Chapter "Sleep-related breathing disorders" of the German Society for Sleep Research and Sleep Medicine (DGSM)
- S2 guideline therapy of obstructive sleep apnea in adults of the German Society for Ear, Nose and Throat Medicine, Head and Neck Surgery (DGHNOKHC). In: AWMF online (as of 2009)
- Obstructive sleep apnea - information at Gesundheitsinformation.de (online offer of the Institute for Quality and Efficiency in Health Care )
- C. Iber et al. a .: The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications . 1st edition. American Academy of Sleep Medicine, Westchester IL 2007
- Map of the DGSM with sleep laboratories in Germany
- Interactive map of the Sleep Apnea Forum for sleep laboratories and self-help groups
Individual evidence
- ↑ Hilmar Burchardi: Etiology and pathophysiology of acute respiratory failure (ARI). In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid 1994, ISBN 3-540-57904-4 , pp. 47-91, here: pp. 67 f.
- ↑ a b c S3 guideline for non-restful sleep / sleep disorders of the German Society for Sleep Research and Sleep Medicine (DGSM). In: AWMF online (as of 2009)
- ↑ Duden
- ↑ Apnea diving
- ↑ a b Riccardo A. Stoohs: resistance syndrome of the upper airways . In: Deutsches Ärzteblatt . Vol. 104, No. 12 , 2007, p. A784-A789 ( aerzteblatt.org [PDF; 336 kB ; accessed on February 4, 2013]).
- ^ UD McCann, FP Sgambati, AR Schwartz, GA Ricaurte: Sleep apnea in young abstinent recreational MDMA (“Ecstasy”) consumers. In: Neurology. December 2, 2009. PMID 19955499
- ↑ M. Kohler, E. Blair, P. Risby, AH Nickol, P. Wordsworth, C. Forfar, JR Stradling: The prevalence of obstructive sleep apnea and its association with aortic dilatation in Marfan's syndrome. In: Thorax. February 2009. PMID 18852161
- ↑ Sleep apnea in babies and young children. Retrieved July 25, 2017 .
- ^ Cardiovascular Consequences of Obstructive Sleep Apnea
- ↑ Basics of Sleep Apnea and Heart Failure ( Memento from February 21, 2014 in the Internet Archive )
- ↑ BM Sanner, M. Konermann, A. Sturm, HJ Müller, W. Zidek: Right ventricular dysfunction in patients with obstructive sleep apnea syndrome. (PDF) In: European Respiratory Journal. Volume 10, 1997, pp. 2079-2083.
- ↑ Breathing mask reduces brain damage in sleep apnea In: Ärzte Zeitung. September 21, 2011.
- ↑ PM Macey: Is brain injury in obstructive sleep apnea reversible? In: Sleep. Volume 35, number 1, January 2012, pp. 9-10, doi: 10.5665 / sleep.1572 . PMID 22215912 , PMC 3242693 (free full text).
- ↑ TT Dang-Vu: Prefrontal dysfunction in obstructive sleep apnea: a biomarker of disease severity? In: Sleep. Volume 36, number 5, May 2013, pp. 631–632, doi: 10.5665 / sleep.2610 . PMID 23633742 , PMC 3622645 (free full text).
- ^ W. Grimm, HF Becker. In: heart. 31 (3), 2006, pp. 213-218. PMID 16770557 , herz-cardiovascular-diseases.de ( Memento of the original from February 18, 2009 in the Internet Archive ; PDF) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ SLEEP APNEA MAY BE LINKED TO HIGHER LEVELS OF ALZHEIMER'S BIOMARKER IN BRAIN
- ↑ § 135 Abs. 2 SGB V
- ↑ Quality assurance agreement kvwl.de ( Memento of the original from January 5, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 63 kB)
- ↑ M. A Puhan: Didgeridoo playing as alternative treatment for obstructive sleep apnea syndrome: randomized controlled trial. In: BMJ (British Medical Journal). Volume 332, 2006, pp. 266-270, doi: 10.1136 / bmj.38705.470590.55 .
- ↑ Christopher P. Ward, Kaki M. York, John G. McCoy: Risk of Obstructive Sleep Apnea Lower in Double Reed Wind Musicians. In: Journal of Clinical Sleep Medicine. 8 (3), June 15, 1012, pp. 251-255, doi: 10.5664 / jcsm.1906 .
- ↑ Devin L. Brown, Darin B. Zahuranec, Jennifer J. Majersik, Patricia A. Wren, Kirsten L. Gruis, Michael Zupancic, Lynda D. Lisabeth: Risk of sleep apnea in orchestra members. In: Sleep Medicine. Volume 10, 2009, pp. 657-660, doi: 10.1016 / j.sleep.2008.05.013 .
- ^ PJC Wardrop, S. Ravichandran, M. Hair, SM Robertson, D. Sword: Do wind and brass players snore less? A cross-sectional study of snoring and daytime fatigue in professional orchestral musicians. In: Clinical Otolaryngology. Volume 36, 2011, pp. 134-138, doi: 10.1111 / j.1749-4486.2011.02297.x .
- ↑ MA Martínez-García, F. Capote, F. Campos-Rodríguez, P. Lloberes, MJ Díaz de Atauri, M. Somoza, JF Masa, M. González, L. Sacristán, F. Barbé, J. Durán-Cantolla, F. Aizpuru, E. Mañas, B. Barreiro, M. Mosteiro, JJ Cebrián, M. de la Peña, F. García-Río, A. Maimó, J. Zapater, C. Hernández, N. Grau SanMarti, JM Montserrat : Effect of CPAP on blood pressure in patients with obstructive sleep apnea and resistant hypertension: the HIPARCO randomized clinical trial. In: JAMA: the Journal of the American Medical Association. Volume 310, Number 22, December 2013, pp. 2407-2415, ISSN 1538-3598 . doi: 10.1001 / jama.2013.281250 . PMID 24327037 .
- ↑ Susanne Schwarting, Ulrich Huebers, Markus Heise, Joerg Schlieper, Andreas Hauschild: Position paper on the use of mandibular advancement devices in adults with sleep-related breathing disorders . In: Sleep and Breathing . Vol. 11, No. 2 , 2007, p. 125–126 , doi : 10.1007 / s11325-007-0116-z , PMID 17464519 , PMC 2211364 (free full text) - (English).
- ↑ DJ Bratton, T. Gaisl, AM Wons, M. Kohler: CPAP vs Mandibular Advancement Devices and Blood Pressure in Patients With Obstructive Sleep Apnea: A Systematic Review and Meta-analysis. In: JAMA. December 2015. PMID 26624827
- ↑ DJ Bratton, T. Gaisl, C. Schlatzer, M. Kohler: Comparison of the effects of continuous positive airway pressure and mandibular advancement devices on sleepiness in patients with obstructive sleep apnea: a network meta-analysis. In: Lancet Respir Med. December 2015. PMID 26497082
- ^ AA Hsu, C. Lo: Continuous positive airway pressure therapy in sleep apnea . In: Respirology . tape 8 , 2003, p. 447-454 , doi : 10.1046 / j.1440-1843.2003.00494.x .
- ↑ Thomas Verse, Karl Hörmann: Operative therapy of obstruction in sleep-related breathing disorders . In: Deutsches Ärzteblatt . Vol. 108, No. 13 , 2011, p. 216–221 , doi : 10.3238 / arztebl.2010.0216 ( aerzteblatt.org [PDF; 422 kB ; accessed on February 4, 2013]).
- ↑ T. Verse, BA Stuck: Modern modifications of uvulopalatopharyngoplasty . In: ENT . tape 65 , no. 2 , February 1, 2017, ISSN 1433-0458 , p. 90-98 , doi : 10.1007 / s00106-016-0300-1 .
- ↑ JR Prinsell: Maxillomandibular advancement surgery for obstructive sleep apnea syndrome . In: J Am Dent Assoc . tape 133 , 2002, pp. 1489-1497 ( utmb.edu [PDF]).
- ↑ German Society for Sleep Research and Sleep Medicine (DGSM): S3 guideline for non-restful sleep / sleep disorders - Chapter "Sleep-related breathing disorders" . Ed .: Springer Medizin Verlag Berlin.
- ↑ Dr. Robert-Marie Frey: Bimaxillary Advancement with CounterClockwise Rotation. Retrieved May 8, 2019 .
- ↑ KW Lye u. a .: Quality of life evaluation of maxillomandibular advancement surgery for treatment of obstructive sleep apnea . In: J Oral Maxillofac Surg . tape 66 , 2008, p. 968-972 ( joms.org ).
- ↑ MJ Zinser, S. Zachow, HF Sailer: Bimaxillary 'rotation advancement' procedures in patients with obstructive sleep apnea: a 3-dimensional airway analysis of morphological changes. In: Int. J. Oral Maxillofac. Surg. Vol. 42, Issue 5, pp. 569-578.
- ↑ Kasey K. Li, Nelson B. Powell et al. a .: Long-Term Results of Maxillomandibular Advancement Surgery. In: Sleep and Breathing. 4, 2000, p. 137, doi: 10.1007 / s11325-000-0137-3 .
- ↑ Patrick J. Strollo, Ryan J. Soose, Joachim T. Maurer, Nico de Vries, Jason Cornelius, Oleg Froymovich, Ronald D. Hanson, Tapan A. Padhya, David L. Steward, M. Boyd Gillespie, B. Tucker Woodson , Paul H. Van de Heyning, Mark G. Goetting, Oliver M. Vanderveken, Neil Feldman, Lennart Knaack, Kingman P. Strohl: Upper-Airway Stimulation for Obstructive Sleep Apnea. In: New England Journal of Medicine. 370, 2014, pp. 139–149, doi: 10.1056 / NEJMoa1308659 .
- ↑ Michael Friedman, Ofer Jacobowitz, Michelle S. Hwang, Wolfgang Bergler, Ingo Fietze, P. Rombaux, GB Mwenge, S. Yalamanchali, J. Campana, JT Maurer: Targeted hypoglossal nerve stimulation for the treatment of obstructive sleep apnea: Six- month results . In: The Laryngoscope . tape 126 , no. November 11 , 2016, ISSN 1531-4995 , p. 2618-2623 , doi : 10.1002 / lary.25909 , PMID 27010361 .
- ↑ Official approval of UAS therapy by the FDA .
- ↑ Th. Verse: Transcutaneous electrical stimulation therapy for obstructive sleep apnea . ( Memento of the original from December 5, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. In: MedReport. No. 32, 26th year, Blackwell Verlag, Berlin 2002.
- ↑ Winfried J. Randerath: Tongue muscle training through electrical stimulation in the therapy of obstructive sleep apnea syndrome. In: Somnology: Sleep Research And Sleep Medicine. 8, 1, 2004, p. 14.
- ^ A b Thomas Gaisl, Sarah R. Haile, Sira Thiel, Martin Osswald, Malcolm Kohler: Efficacy of pharmacotherapy for OSA in adults: A systematic review and network meta-analysis . In: Sleep Medicine Reviews . tape 46 , August 2019, ISSN 1532-2955 , p. 74-86 , doi : 10.1016 / j.smrv.2019.04.009 , PMID 31075665 .
- ↑ Elimination of the degree of use T3 ( Memento of the original from December 4, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 126 kB)
- ↑ Annex 3/45 of the central service regulation 46/1 of the Federal Ministry of Defense (PDF; 58 kB)