Polysomnography
The polysomnography (also polysomnography , shortly PSG) (of lat./griech. Much (times), sleep, write / record) is a diagnostic method for measuring physiological functions and provides the most comprehensive study of sleep is a person. With this technique, several different body functions continuously monitored throughout the night. Usually this is done in a stationary sleep laboratory . With the help of the recordings, an individual sleep profile can be created, which should enable a diagnosis of sleep disorders .
application
Typical complaints ( key symptoms ) that can justify an examination with the help of polysomnography are disturbances in falling asleep , waking up during the night or constant daytime sleepiness ; Likewise, heavy snoring with breathing interruptions perceived by third parties. See also: sleep apnea syndrome .
In sleep medicine , polysomnography is recommended for diagnosing the following sleep disorders according to ICSD-2 :
- Sleep-related breathing disorders,
- Hypersomnias and
- Sleep-related movement disorders.
Under certain conditions, it can also be used for insomnias, circadian sleep-wake rhythm disorders , parasomnias and sleep disorders from the group of isolated symptoms, standard variants, unresolved problems according to ICSD-2. In addition, polysomnography can be used for differential diagnostics and exclusion diagnostics in individual cases.
Cardiorespiratory polygraphy is also recommended for sleep-related breathing disorders and sleep-related movement disorders . With this method, less information is collected with a simplified system. The diagnosis of obstructive sleep apnea is possible after a comprehensive previous medical history of sleep, provided there are no other diseases or sleep disorders.
Conducting the investigation
recommendations
There are detailed recommendations for carrying out this investigation, which concern the measurements, the equipment and personnel, the premises and the evaluation.
In Germany, the guideline "Non-restful sleep / sleep disorders" of the German Society for Sleep Research and Sleep Medicine (DGSM) gives recommendations on this procedure. According to this, the "cardiorespiratory polysomnography in the sleep laboratory with monitoring by qualified sleep medicine personnel" is recommended as a basic instrument and as a reference method, whereby the measurement and evaluation should be carried out according to the current recommendations of the American Society for Sleep Medicine (AASM). Videometry is considered to be indispensable for the diagnosis of parasomnias and the differential diagnosis.
In the medical guidelines on various sleep disorders such as narcolepsy , restless legs syndrome (RLS) and periodic limb movement disorder (PLMD) and insomnia, reference is made to this procedure for diagnosis in principle or in a limited way to special cases.
Due to the requirements for the accreditation of sleep laboratories by the specialist sleep medicine associations, the national and international recommendations for the sleep laboratories concerned become binding.
Measurements
Polysomnography monitored by sleep medicine in the sleep laboratory is regarded as a basic instrument and reference method for the device-based diagnosis of sleep disorders. This includes the recordings of sleep EEG , EOG , EMG , EKG , respiratory flow, breathing effort, oxygen saturation, body position and video, the latter being recommended as indispensable for diagnosing parasomnias and differentiating forms of epilepsy.
Before taking measurements in the sleep laboratory, the patient is usually observed for a day in order to identify his activities and habits. Usually two nights are then spent in the laboratory.
In the case of inpatient polysomnography, the following monitoring is carried out as required:
- Brain wave image (EEG)
- Heart rhythm (EKG)
- Oxygen content of the blood ( pulse oximetry )
- Body temperature
- Respiratory flow (mouth and nose)
- Breathing movement
- Muscle tension (EMG)
- Leg movement
- Eye movement (EOG)
- Body position
In addition, the following measures or measurements can be taken during sleep:
- Sound recording
- Video
- Blood pressure
- Gastric acid reflux
- Differences in pressure in the chest
- Erections
- Mask pressure (for breathing masks )
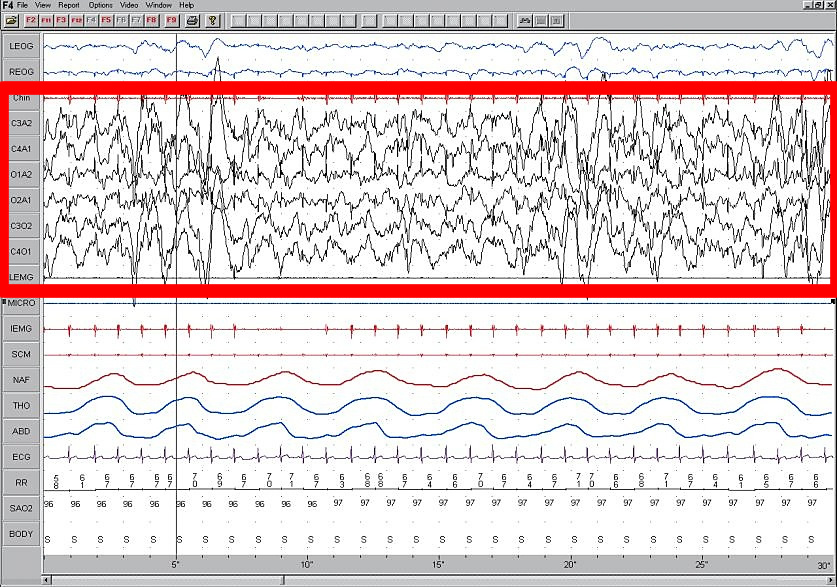
A polysomnogram
The following screenshot shows recordings during 30 seconds of sleep phase 4 deep sleep .
The time runs to the right in the graphic; it is scaled in the lower window frame. The image has a resolution of 26 pixels per second.
The top 2 blue zigzag lines represent - measured electrically - the movements of the eyes.
The band of strongly jagged brain waves is framed in red, measured as voltages between two electrodes.
LEMG and MICRO underneath show no recordings, recognizable by the straight line.
IEMG, a muscle current and another red line with almost regular pulses are synchronized with the heartbeat (below) - about 1 time per second.
3 wavy lines then show the breathing flow through the nose (NAF) and the movement of the chest (THO) and abdomen (ABD).
The peaks of the current from the heart contraction (ECG - electrocardiogram) every second, including the 58 to 71 numerical values of the pulse rate in / min, are concise.
Every second a value of the oxygen saturation of the blood (96-97%) is given and the body position on the "S" side.
Electrode points EEG (brain current)
- C3
- top left central
- C4
- top right central
- A1
- left ear
- A2
- right ear
- O1
- left occipital (left occiput)
- O2
- right occipital (right occiput)
- Chin EMG
- EMG1 chin left, EMG2 chin right
- LEMG
- laryngeal electromyogram (EMG1 left larynx, EMG2 right larynx) (muscle current)
Further measurements
- LEOG
- left electrooculography (left eye)
- REOG
- right electrooculography (right eye)
- NAF
- Breathing the nasal airflow
- THO
- thoracic breathing movement
- IEMG
- integrated electromyogram
- ABD
- abdominal breathing movement
- ECG
- electrocardiogram
- RR
- Heartbeat interval
- SAO2
- arterial oxygen saturation
- BODY
- Position of the body (p
- Lateral position)
- SCM
- scanning capacitance microscope
See also
literature
- American Academy of Sleep Medicine (Ed.): The AASM Manual for Scoring Sleep and Associated Events. Rules, technology and technical specifications . 1st edition. Steinkopff-Verlag, Heidelberg 2008, ISBN 978-3-7985-1851-3 .
Web links
Individual evidence
- ↑ a b c S3 guideline for non-restful sleep / sleep disorders of the German Society for Sleep Research and Sleep Medicine (DGSM). In: AWMF online (as of 2009).
- ↑ Conrad Iber, Sonia Ancoli-Israel, Andrew L. Chesson, Stuart F. Quan: The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications . Ed .: American Academy of Sleep Medicine. AASM, Westchester, Ill. 2007.
- ^ S1 guideline narcolepsy of the German Society for Neurology. In: AWMF online (as of 2008)
- ^ S1 guideline Restless Legs Syndrome (RLS) and Periodic Limb Movement Disorder (PLMD) of the German Society for Neurology (DGN). In: AWMF online (as of 2008)
- ↑ Dirk Pevernagie, Steering Committee of the European Sleep Research Society: European guidelines for the accreditation of sleep medicine centers . In: Journal of Sleep Research . Vol. 15, No. 2 , 2006, p. 231-238 , doi : 10.1111 / j.1365-2869.2006.00524.x , PMID 16704580 (English).