CPAP ventilation

The CPAP , including CPAP (Abbreviation for continuous positive airway pressure ) is a ventilation mode , the spontaneous breathing of the patient with a permanent, while inhalation and exhalation maintained, positive pressure ( PEEP combined). The patient can determine his breathing depth , breathing frequency and also the flow (air flow ) himself. The prerequisite for the use of CPAP ventilation is therefore the patient's ability to breathe on his own. CPAP ventilation is used in intensive care and emergency medicine (then combined with assisted spontaneous breathing ) as an application in intubated or non-invasively ventilated patients, but also in outpatient settings as a therapy for sleep apnea .
technical structure
A patient is connected to a ventilator via a hose system. A pressure above atmospheric pressure ( PEEP ) is generated in the tube system and subsequently in the airways and alveoli . This overpressure makes it easier to breathe in . In addition, however, it makes exhalation more difficult, since the higher ambient pressure represents a resistance due to the deviation from the normal pressure level. This higher pressure is present in the ventilation system continuously (continuous flow CPAP and PEEP valve) or with a variable inspiration flow (demand flow CPAP with proportional valve).
CPAP ventilation can be used both as an invasive ventilation method, i.e. via a tube or a tracheal cannula , and as non-invasive ventilation , non-invasive ventilation (NIV) , i.e. via a mask (for example a mouth-and-nose mask, nasal mask , Face mask, oral mask or helmet) possible.
effect
The positive pressure generated in the airways and lungs causes an increase in functional residual capacity (i.e. the amount of air that remains in the lungs after exhalation). The end-expiratory collapse of the alveoli and small airways is prevented. The formation of atelectasis is partially prevented or atelectasis is reopened ( recruitment , alveolar recruitment , mostly recruitment ), thereby increasing the diffusion area of the alveoli and reducing right-left shunts in the pulmonary vascular pathway. As a result, CPAP improves the ventilation / perfusion ratio, oxygenation and reduces the work of breathing.
NIV CPAP
In the case of non-invasive ventilation (NIV), the patient is provided with a mask which, depending on the design, covers the nose / mouth area, covers the entire face or is built as a full helmet. This mask has a relative tightness and inhaled air is made available through it. In addition, purely nasal CPAP (nCPAP) is also used in neonatology, either using nasal masks or nasal prongs ( nasal cannula ).
Similar to invasive ventilation, which takes place via an endotracheal tube or a tracheal cannula , different ventilation methods can also be used with NIV (describing various interactions between patient and ventilator in ventilation technology).
Patients tolerate CPAP ventilation very differently. With mask ventilation and the use of PEEP , a slight sedation is usually administered in order to increase the tolerance for this measure and thus make the situation more bearable for the patient. However, the sedation must not be too strong, otherwise the respiratory drive could be lost and the patient could give up breathing independently.
The NIV is always indicated when a patient with reduced breathing is to be given as gentle support as possible, e.g. B. in the beginning of cardiac pulmonary edema , in moderate pneumonia (pneumonia) or in COPD (chronic obstructive pulmonary disease). For the latter, pure CPAP ventilation is often unfavorable. Instead, further breathing support is indicated in order to relieve the respiratory muscles and give them time to regenerate.
NIV often saves intubation , which entails longer ventilation times and, consequently, a longer hospital stay with correspondingly increasing costs, and removes the patient from his normal living environment for longer.
The use of devices creates the possibility on the one hand and the need to control breathing on the other. If the mask is not completely sealed, there is a constant loss of positive pressure and breathing air from the ventilation system, which can only be partially compensated for by the ventilation device. As always, the error tolerance of the measurements must also be taken into account here.
Despite the obligatory humidification of the breathing air, the mouth and nose become dry. The mask must therefore be taken off regularly, which depends on the one hand on the necessity and urgency of ventilation and on the other hand on the dehydration of the oral and nasal mucosa and varies greatly from person to person. Since the masks are fixed as close as possible to the head, there is also the risk of pressure ulcers ( pressure sores) as accompanying diseases .
CPAP via tube
If the patient's endotracheal intubation cannot be avoided, various ventilation patterns are available (see the nomenclature of mechanical ventilation in the ventilation article ). CPAP ventilation with an endotracheal tube or with a tracheostoma corresponds to that with a mask, but sometimes has different functions. For most clinical pictures, rapid augmentation (assisted) ventilation of the patient is sought. If a patient is so physically exhausted that they have to be intubated, they can only be ventilated immediately with CPAP in rare cases; Mandatory procedures, i.e. the complete takeover of the breathing work by the ventilator, are then indicated.
CPAP is used when the patient is weaning, i.e. when he is being trained by the machine. Patients who have been subject to mandatory ventilation for a longer period of time have to regenerate the auxiliary respiratory muscles in order to take over the work of breathing again themselves, which regress strongly in a short time. In the course of weaning, the ventilation mode CPAP is selected for ever longer periods of time in order to ultimately be able to carry out the extubation (removal of the tube).
As a rule, CPAP ventilation performed in the clinic takes place using ASB pressure and PEEP . The patient is given a certain auxiliary pressure that accompanies each breath and also makes it easier to inhale. In contrast to the PPS ventilation pattern , the auxiliary pressure is constant. That means, it is completely irrelevant how strongly the ventilated person draws in air; every breath is accompanied with the same preset pressure level.
Advantages and disadvantages
The advantages of CPAP in an awake patient with adequate respiratory drive and neuromuscular abilities lie in an increase in the oxygen content in the lungs, an increase in the gas exchange area and an improvement in the volume conductivity of the airways with easier mucociliary clearance ; secretion can therefore be transported away more easily through the larger lumen . In summary, positive effects include the short-term improved breathing situation due to easier inhalation and better diffusion as well as improved secretion transport. This form of ventilation plays a major role in training off the ventilator and can definitely be seen as an improvement.
In the long term, ventilation with CPAP can lead to a reduction in lung volume, as prolonged overinflation can also damage the lungs. Furthermore, patients occasionally become accustomed to a certain degree of habit, i.e. it has become comfortable for these people to find such an easier inhalation and they are only able to find it difficult to regain normal breathing behavior out of habit (see especially COPD - Patients).
In addition, premature babies run the risk of bloating symptoms with a severe deterioration in their general condition. The influence of a changing oxygen supply on the immature retina of premature infants can damage the retina and, in rare cases, lead to its detachment. In order to control the development of the retina, all very immature babies should be examined by an ophthalmologist after the first few weeks of life and then usually on a weekly basis. There is practical evidence that critical damage to the retina in the form of macular edema, e.g. B. epiretinal glioses with unusual visual acuity loss, even in adults, can be traced back to the damaging influence of ongoing CPAP therapy.
criticism
The use of CPAP in patients with a tracheal tube is controversial in the clinic because CPAP does not offer breathing assistance. However, the mode is experiencing a renaissance in non-intubated patients as a strategic element of non-invasive ventilation ( weaning ).
Use to treat sleep apnea
execution
CPAP therapy is also used to treat temporary respiratory arrests during sleep for sleep apnea . With CPAP therapy, the patient is continuously supplied with breathing air (ambient air) with a slight excess pressure while sleeping . As a rule, the air is sucked in by a CPAP device next to the bed and fed to the sleeper via a hose using a full or nasal mask ( nCPAP mask n = nasal). Depending on the anamnesis and any impairment of the lung function, the air supplied is also heated and humidified.
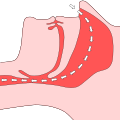
The tissue in the nasal and throat areas of the sleeper, which is relaxed during sleep, is stabilized and kept open by the slight overpressure. The therapy is less about ventilation and more about what is known as “pneumatic splinting”. This reliably prevents respiratory arrests ( apneas ) and air obstructions ( hypopneas ). As a side effect, this also largely suppresses snoring .
The diagnosis and therapy for this is generally initiated for the first time with a mobile breathing monitor that can be used at home and then determined over several nights in a sleep laboratory , in which several cabled sensors attached to the body measure respiratory arrests and blood oxygen levels in particular overnight. To observe the REM sleep phases and other sleep phases, eye movements are measured and brain waves are derived. If the diagnosis is confirmed, an individual, therapeutic pressure is gradually approached. Excessive pressure may cause the compressed air to flow out again immediately through the mouth or, in the worst case, disrupt spontaneous breathing.
- Working principle
Duration of therapy
In the vast majority of cases, CPAP therapy is a long-term therapy that significantly reduces respiratory arrest, but does not cure it. The device and mask are therefore - like glasses, for example - so-called aids. The CPAP machine and mask must be used and worn every night, at home and when traveling. An arbitrary, unauthorized termination of therapy, e.g. B. for convenience, the treated symptoms and impairments usually bring back immediately or within a short time. The therapy is checked at individual intervals, from months to years. The nightly breathing work is recorded at home with a mobile device and discussed later with a specialist. A renewed stay in the sleep laboratory can take place if the therapy is intended to be changed, where it is measured and evaluated again under observation.
Special forms
APAP
A further development of the CPAP therapy is the APAP therapy (auto CPAP therapy). The therapeutic pressure required in each case is determined from breath to breath and supplied to the patient. The employees in the therapy (compliance) and the well-being of the patients are improved, and the print-related side effects are reduced. The APAP is indicated in the therapy of sleep apnea in the case of position dependence or REM sleep association and is also covered by the health insurance companies if these conditions are present. In the case of central sleep apnea, at least one attempt at therapy with CPAP or APAP is indicated, because better oxygenation (oxygen saturation) and thus suppression of central apneas can possibly be achieved by mobilizing the functional lung reserve.
BIPAP
The BIPAP (Bi = two, PAP = positive airway pressure) or BI-level therapy is an independent further development. In this form of therapy, different pressures are generated for inspiration and expiration, which also increases comfort, but also for certain patients, e.g. B. with disturbance of the cardiac output ( heart failure ), is of vital importance. A special form of BIPAP therapy is VPAP therapy (V = variable), in which the inspiratory pressure, analogous to APAP therapy, is variable within defined limits and adapts to the therapeutic needs with every breath.
additional
In addition, CPAP and APAP devices from various companies have a comfort function that lowers the end-expiratory pressure at high expiratory pressures and thus suppresses a feeling of pressure or shortness of breath during exhalation due to the lower counter pressure.
Masks
Compared to earlier models, modern masks have become much smaller and lighter and are made from highly elastic, transparent plastics. Mask systems that are used in the area of CPAP or APAP therapy generally have an exhalation system (vented) or must be operated with an external exhalation system (non-vented) so that the exhaled CO 2 is washed out .
So-called nose pads, which are worn under the nose and hardly resemble a mask, are sufficient for forms of therapy with low pressure. Most often, a mask that only encloses the nose is used. Other mask designs - for example "full face masks" that enclose the mouth and nose - offer individual solutions.
Full face masks are mainly used in the therapy of patients with mouth leaks. Some of them lead to the drying out of the oral mucosa and often cause the user to feel uncomfortable in the throat. However, a full face mask is not absolutely necessary. The patient can often be helped by using a chin strap.
literature
- Medicine in Dialogue , September 2002 edition, ISSN 1434-2804
- L. Juchli: Care . 7th edition. Thieme Verlag, 1994, ISBN 3-13-500007-9
Web links
Individual evidence
- ↑ D. Weismann: Forms of ventilation. In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid 1994, ISBN 3-540-57904-4 , pp. 201-211; here: pp. 203–205.
- ↑ RA. Mahmoud et al .: Current methods of noninvasive ventilatory support for neonates . 2011.
- ↑ Ernst Bahns: It all started with the Pulmotor. The history of mechanical ventilation. Drägerwerk, Lübeck 2014, p. 58 f. ( The ventilator in clinical use - an overview ) and 60 f. ( Breathing and ventilation method - a fundamental difference ).
- ↑ D. Weismann: Forms of ventilation. 1991, pp. 203-205.