Nasogastric tube
A nasal tube , nasal or transnasal probe is inserted through the nasal tube. Some transnasal tubes are used for artificial feeding of a person , but they can also be used for relief, as bleeding can be suctioned off or stomach contents can be drained away. Another form is a nasal probe, which is connected to an oxygen device via a line system and enriches the inhaled air with oxygen; it is called an O 2 nasogastric tube.
Transnasal probe
Depending on the type and manufacturer, the probes are made of PVC , polyurethane , latex or silicone rubber . There are various details about the length of time a nasogastric tube remains in place. Depending on the shelf life of the material used for the nasogastric tube, a tube can be stored for up to four weeks or longer. PVC and latex probes, in particular, are only chosen for a very short dwell time, for example for discharging blood or toxins, because of their poor tolerance.
A transnasal tube is only advisable for short-term nutrition or other therapy of the patient , since the swallowing reflex can be reduced by the lying tube in the pharynx . In addition, pressure points can arise. For long-term feeding via a feeding tube, the installation of a percutaneous endoscopic gastrostomy (PEG) is usually recommended.
Nasogastric tube
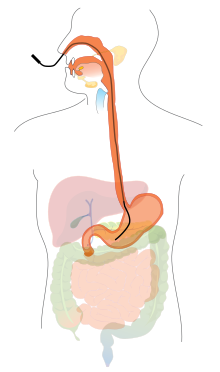
The nasogastric tube is placed through the nostril via the pharynx within the esophagus and into the stomach . The patient does not need any anesthetic or anesthesia for this procedure . The outer part of the probe is then attached to the bridge of the nose with an adhesive plaster . To check the correct position of the probe, gastric juice is drawn off using a syringe and its pH value is tested. If this is alkaline, the probe is probably in the small intestine and the probe must be reinserted. Another control method is to draw up about 20 ml of air into a bladder syringe and administer it through the tube while listening to the stomach area with a stethoscope . If a gurgling sound can be heard in the stomach, the probe is correctly positioned.
The position check must be carried out after each probing and before each feeding and liquid administration. Nutrition with special tube feeding can begin immediately.
Nasoduodenal probe
The nasoduodenal tube is inserted like a nasogastric tube, but the target is not the stomach, but the duodenum , the duodenum. The probe is usually placed under x-ray control; the probes themselves are longer than the nasogastric probes and differ, for example, by an inserted guide wire, a rollable tip or a holding balloon. The advantage of positioning in the duodenum is the reduced risk of aspiration , but a low-osmolar diet should be selected because it is better tolerated. It should only be given through a feeding pump so that it runs slowly into the small intestine.
Oxygen nasogastric tube
Single nasal probes for air enrichment (insufflation) with oxygen are usually fixed in a nostril with the help of a foam ring. The probe is inserted about one centimeter into the nose. The patient is not hindered by the probe when eating and drinking, but the probe tends to slip out due to the type of attachment without further fixation with plasters. Therefore, it has been the so-called oxygen glasses developed that, especially in the long-term continuous oxygen therapy is used. The tube divides into a loop roughly in the middle. The loop is placed over both ears or fixed at the back of the head so that the approx. 1 to 1.5 cm long inflow sockets reach into the nostrils. The seat of the probe can be adjusted under the chin.
Irritation of the nasal mucosa is common with both types of probe; In addition, pressure points can develop in the nose, and behind the ears with the oxygen cannula. In addition, there is a risk of strangulation due to the loop of the glasses if used improperly or in disoriented patients (as well as with the use of oxygen masks).
Individual evidence
- ↑ a b c Walied Abdulla: Interdisciplinary Intensive Care Medicine . 3. Edition. Elsevier, Urban & FischerVerlag, 2006, ISBN 3-437-22711-4 , pp. 407-408 .
- ^ Ina Pfitzer, Maren Asmussen-Clausen : Care techniques today: Understanding care activities step by step . Elsevier, Urban & FischerVerlag, 2006, ISBN 3-437-27090-7 , pp. 357 .
- ↑ S. Jochum et al .: ATL breathing, pulse and blood pressure. In: Thiemes care . Georg Thieme, Stuttgart, 2009, ISBN 978-3-13-500011-4 , p. 494-495 .