Charcot-Marie-Tooth disease
| Classification according to ICD-10 | |
|---|---|
| G60.0 | Hereditary sensorimotor neuropathy including Charcot-Marie-Tooth-Hoffmann syndrome |
| ICD-10 online (WHO version 2019) | |
The Charcot-Marie-Tooth disease (CMT) was after its discoverers Jean-Martin Charcot (1825-1893), Pierre Marie (from 1853 to 1940) and Howard Tooth named (1856-1926). Today, the term hereditary motor-sensitive neuropathy type I (HMSN I) is more common. It is also called neural muscular atrophy and is a neuromuscular disease . Another name is Charcot-Marie-Tooth-Hoffmann syndrome , with the involvement of the German neurologist Johann Hoffmann . The Roussy-Lévy syndrome is considered a variant of this disease.
Epidemiology
Charcot-Marie-Tooth disease is the most common neurogenic disease. 20-30 people per 100,000 inhabitants are affected. There are mostly one autosomal - dominant inherited disease. Therefore there are accumulations in individual families. Usually the cause is a mutation on chromosome 17 .
etiology
CMT is an inherited disease of the peripheral nerves . The nerve cell extension, called the axon , or the insulating myelin layer is damaged by a gene mutation . The myelin acts like a plastic insulation around an electrical cable. In the case of the disease, the saltatory conduction of excitation , i.e. the transmission of nerve impulses in peripheral nerves, is hindered. As a result, commands from the brain do not reach the muscles or reach them correctly. The denervation results in weakness and degradation of the affected muscles.
Unlike muscular dystrophies , CMT patients are born with normal muscles. The muscles shrink (atrophy) because nerves impaired by CMT do not accurately transmit commands from the brain for certain movements.
The primary defect is the duplication of the PMP (Peripheral Myelin Protein) gene on chromosome 17. As a result, myelin sheaths thicken. Soon the myelin sheath and / or the axon will be damaged, presumably due to a lack of nutrients. The more the myelin layer is damaged, the lower the nerve conduction speed and the more severe the severity of the clinical picture. A nerve conduction speed of 50 m / s is normal. The demyelinating form has a conduction speed of <38 m / s, the axonal form of> 38 m / s.
Symptoms
The disease often begins in childhood. Sometimes manifestations are not noticed until between the ages of 20 and 30. The main symptoms are increasing weakness of the hands and feet, which soon spreads to the arms and legs. Sometimes those affected are left with only the help of crutches or even a life in a wheelchair.
As a rule, the tibialis anterior muscle (foot lifter), which runs down the front of the shin, is the first muscle affected. This results in an unsteady gait: the foot hangs limply, you stumble easily and you have to lift your leg from the thigh until your toes also come off the floor. The foot hits the ground again with a slap. This is clearly referred to as a stepper or stork walk.
The reflexes , especially the Achilles tendon reflex , fail early.
diagnosis
The measurement of the (considerably reduced) nerve conduction velocity and the nerve biopsy support the diagnosis. A genetic test to identify the underlying mutation is also possible. There is no causal treatment.
Differential diagnostics
The Rosenberg-Chutorian syndrome and Hagemoser-Weinstein-Bresnick syndrome are to be distinguished .
Course and prognosis
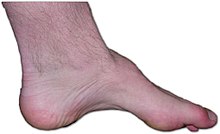
With a longer course, the atrophy of the lower leg muscles is immediately visible, the lower legs appear delicate, while the thigh muscles can still be well developed. Sensitive irritation symptoms (pain, paresthesia, muscle cramps) are part of the clinical picture. Motor failure symptoms are more pronounced and determine the symptoms. The atrophy of the muscles progresses almost symmetrically. Overall, the process is very slow and lasts for decades. A cure for the genetic disease is not yet possible. So far, the disease has only been alleviated in experiments on mice with rapamycin .
literature
- M. Auer-Grumbach: Hereditary sensory neuropathy type I. In: Orphanet J Rare Dis. 2008 Mar 18; 3, p. 7. Review. PMID 18348718 PMC 2311280 (free full text)
Individual evidence
- ↑ Linda Sawade, Federica Grandi, Marianna Mignanelli, Genaro Patiño-López, Kerstin Klinkert: Rab35-regulated lipid turnover by myotubularins represses mTORC1 activity and controls myelin growth . In: Nature Communications . tape 11 , no. 2835 , June 5, 2020, ISSN 2041-1723 , doi : 10.1038 / s41467-020-16696-6 ( nature.com [accessed June 9, 2020]).