Hemolytic anemia
As hemolytic anemia refers to all forms of anemia (anemia), in which the red blood cells do not reach their normal life.
causes
A distinction is made between changes in the blood cells themselves (corpuscular cause) and causes independent of the blood cells (extracorpuscular cause) as causes .
Corpuscular hemolytic anemia
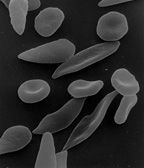
Corpuscular haemolytic anemia is usually based on a genetic defect in one of the components of the erythrocytes. If the cell membrane is defective , depending on which protein is affected by the mutation , spheroid cell anemia (spherocytosis, in the case of a defect in the cytoskeleton , more precisely spectrin or ankyrin ), elliptocytosis (defective spectrin or protein 4.1 ), a stomatocytosis (more precisely unknown defect) or a acanthocytosis (absence of apolipoprotein B ) on. The paroxysmal nocturnal hemoglobinuria (PNH) also results from a defect in the cell membrane, due to an acquired mutation of the pig-A gene, the binding of several proteins with the outer cell membrane is poor. As a result, the drop in blood pH at night (hence the name) promotes hemolysis. PNH has an annual incidence of less than 1 / 100,000. Another cause can be a deficiency in one of the enzymes within the erythrocytes ( glucose-6-phosphate dehydrogenase deficiency ( favism ) or pyruvate kinase deficiency ). Ultimately, defects in the synthesis of hemoglobin, so-called hemoglobinopathies , can lead to the lysis of erythrocytes and the resulting anemia. The thalassemia and sickle cell anemia are particularly emphasized here .
Extracorpuscular hemolytic anemia
Extracorpuscular hemolytic anemias are caused by causes outside of the red blood cells. On the one hand, this concerns the mechanical destruction of cells, for example on artificial heart valves or as a result of microangiopathic processes, in particular in disseminated intravascular coagulopathy , in thrombotic-thrombocytopenic purpura and in haemolytic-uremic syndrome . Plasmodia , the causative agent of malaria , multiply in red blood cells and ultimately destroy them. In addition, chemicals such as copper and lead, but also toxins such as snake and spider venom or bee stings can lead to hemolysis. In addition, hemolytic anemia can rarely occur as complications of Clostridial infections. In immune hemolysis, the erythrocytes are destroyed by internal or external defense reactions ( graft-versus-host reaction ). This occurs either as a reaction to a foreign antigen in transfusion reactions or in the case of incompatible rhesus factors between mother and fetus ( Morbus haemolyticus neonatorum ) or as an autoimmune disease against antigens located on the cells. These autoimmune hemolytic anemias are divided into a warm and a cold type. In the warm type (70% of all patients), IgG antibodies bind to the surface of the red blood cells and thus ensure that these are removed from the circulation in the spleen. The causes are either idiopathic or autoimmune diseases such as systemic lupus erythematosus , rheumatoid arthritis or chronic lymphocytic leukemia . In the cold type, IgM antibodies bind to the erythrocytes in the peripheral circulation as a result of exposure to cold and thereby cause agglutination (clumping) of the cells, which leads to painful acrocyanosis (blue discoloration of the body appendages). This can also occur idiopathically, as a result of infections with Mycoplasma pneumoniae , in Pfeiffer glandular fever or in lymphoproliferative diseases. After viral infections in childhood, so-called bithermal hemolysis can also occur acutely, mediated by IgG antibodies. However, this usually goes back after the infection has subsided without complications. In paroxysmal nocturnal hemoglobinuria , the erythrocytes are destroyed by the complement system .
Clinical phenomena and diagnostics
The usual symptoms of anemia such as decreased performance, weakness, rapid fatigue, dizziness, ringing in the ears, paleness of the skin and mucous membranes and, if necessary, an increase in indirect bilirubin in the blood, yellowing of the skin and sclera (= icterus ). The bile pigment is increasingly excreted in the stool and urine, which is why both can have a dark color. Diagnostically, an increase in the number of reticulocytes , a polychromatism and an increase in erythroblasts in the bone marrow are particularly important.
course
A decrease in the number of red blood cells in the blood occurs when their breakdown is so accelerated that it can no longer be compensated for by increased production in the red bone marrow . The number of reticulocytes is therefore typically increased, as is the iron content of the blood and the spleen is often enlarged for the same reason ( splenomegaly ).
therapy
The therapy basically depends on the cause. In corpuscular forms in many cases, symptomatic a splenectomy be displayed. In the case of extracorpuscular forms that are triggered by autoantibodies, a corticoid (e.g. prednisolone ) is used, for example , and in the case of infection-related forms (e.g. in the context of tropic malaria ), specific treatment of the offending disease is necessary.
In cases of severe anemia, the administration of foreign blood ( blood transfusion ) may be necessary symptomatically ; the use of erythropoietin must be handled restrictively due to the high risk of side effects.
See also
Individual evidence
- ↑ S. Silbernagl among others: Pocket Atlas of Pathophysiology. Georg Thieme Verlag, 2005, ISBN 3-13-102192-6 , p. 40, (online)
- ↑ a b G. Herold et al .: Internal medicine. 2007.
- ↑ a b c d W. Gerok: The internal medicine: reference work for the specialist. Schattauer Verlag, 2006, ISBN 3-7945-2222-2 , p. 63, (online)