malaria
| Classification according to ICD-10 | |
|---|---|
| B50 | Malaria tropica caused by Plasmodium falciparum |
| B51 | Malaria tertiana caused by Plasmodium vivax |
| B52 | Quartana malaria due to Plasmodium malariae |
| B53 | Other parasitologically confirmed malaria |
| B54 | Malaria, unspecified |
| ICD-10 online (WHO version 2019) | |
Malaria - also known as common fever , paludism , intermittent fever , marsh fever , intermittent fever , cold fever or outdated acclimatization fever , climate fever , coastal fever , tropical fever - is an infectious disease caused by single-cell parasites of the Plasmodium genus . Nowadays it is mainly transmitted in the tropics and subtropics by the bite of a female mosquito of the genus Anopheles . Outside of these areas, mosquitoes introduced by air traffic occasionally trigger what is known as “airport malaria”. All people in the direct vicinity of airports are at risk, e.g. B. Airport employees or residents. With the exception of transmission through blood transfusion and laboratory accidents, human-to-human infection is only occasionally possible from mother to unborn child when the placenta is injured (especially during childbirth). Humans and the Anopheles mosquitoes represent the only significant reservoir of pathogenic plasmodia.
Malaria is the most common infectious disease in the world, with around 200 million people infected each year. Using scientific computer models, around 1.2 million deaths due to malaria infection were calculated for 2010, based on data collected from 1980 to 2010. According to the models, the number of malaria deaths peaked in 2004 at 1.8 million.
Essentially, a distinction is made between three clinical pictures, depending on the various malaria parasites: Malaria tropica , Malaria tertiana and Malaria quartana .
In the past only four pathogens were considered to be pathogenic to humans: Plasmodium falciparum , Plasmodium vivax , Plasmodium ovale and Plasmodium malariae . It is now known that another strain from Southeast Asia, which was previously considered to be mainly dangerous for macaques , can infect humans in larger numbers than previously assumed: Plasmodium knowlesi .
With regard to the course of the disease and their geographical distribution, the pathogens differ considerably. Plasmodium falciparum is the clinically most important and most threatening pathogen of malaria, which was formerly also known as malignant intermittent fever .
The symptoms of malaria are high, recurring to periodic (alternating) fever , chills , gastrointestinal complaints and cramps . The disease can quickly lead to coma and death , especially in children . The frequency of the fever attacks results from the length of the multiplication cycles of the pathogen.
In Austria and Switzerland the disease is notifiable , in Germany only the proof of the pathogen.
Word origin
The name of the disease malaria is derived from the Italian mal'aria ("bad air", which rises as bad evaporation, also called miasma , especially from the swamps and has been thought to cause disease since ancient times, especially in fever (Febris intermittens)) from Latin mala "bad", and aer "air". The Italian expression mal (a) aria can be found in 1709 in a work by the physician Francesco Torti (1658–1741), a personal physician of Francesco II. D'Este and Rinaldo d'Este, which treated this disease extensively .

Epidemiology
Geographical distribution
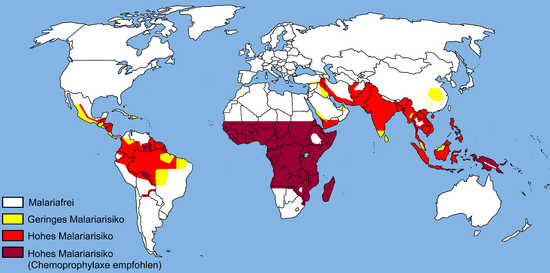
The geographical distribution of malaria (see map 2005 - current map at DTG, web links ) is similar to the temperature distribution of the earth in the 21st century. The Anopheles species suitable as carriers occur on all continents (except Antarctica ), whereby the distribution area of the Anopheles mosquito is limited to low sea levels (below 2500 m on the equator and below 1500 m in the other regions). Malaria was particularly widespread in northern Europe and North America towards the end of World War II. The risk in the individual endemic areas is very different, which is also due to seasonal and geographical reasons. In sub-Saharan Africa , Plasmodium falciparum clearly predominates over all other Plasmodia species. A return of malaria to Central Europe due to global warming is controversial.
Genetic mutations and role of malaria in human history

The modern man ( Homo sapiens ) was for the greater part of human history exposed to the threat of malaria infections. It is estimated that the first representatives of Homo sapiens appeared in East Africa around 200,000 years ago. From there they gradually spread over the whole earth. The climatically cold and malaria-free regions of the world were only settled by modern humans in the last 20,000–30,000 years.
Over time, mutations have emerged in the human population that offer some resistance to the severe forms of malaria. These mutations affect the erythrocytes (red blood cells) in which the malaria parasite develops. These are primarily mutations in the genes of hemoglobin ( hemoglobinopathies ), but also mutations in the metabolism of the erythrocytes:
- Formation of hemoglobin mutants:
- Sickle cell anemia (formation of hemoglobin S, in tropical Africa)
- Hemoglobin C (in West Africa)
- Hemoglobin E (in Southeast Asia)
- Hemoglobin D (in India)
- Decreased synthesis of hemoglobin:
- α- / β- thalassemia (in the Mediterranean region, all of South Asia, North Africa)
- Enzyme defects in erythrocyte metabolism:
Heterozygous carriers (with only one mutated allele ) can develop malaria, but are protected from the more severe forms, as the malaria parasites cannot multiply as well in the erythrocytes. If left untreated, homozygous carriers (both alleles mutated) often have a significantly reduced life expectancy (e.g. in sickle cell anemia) because the function of the erythrocytes is disturbed. Globally, around 8% of today's world population are affected by one of the above mutations. The hemoglobinopathies are thus by far the most common human hereditary diseases. In some regions of the world (area around the East African lakes, parts of Southeast Asia) up to 50% of the local population are carriers. The fact that such mutations, which for the most part have considerable disadvantages, especially in homozygous form for the respective carrier, have persisted in the human population is impressive evidence of the great genetic pressure that malaria has exerted on human development . In areas with less frequent or only episodic occurrence of malaria (Northern Europe, Northern Asia), the above-mentioned mutations are not found in the native population; they have been eliminated by selection pressure within a few thousand years.
In addition, it has been known since 2012 that there are gene variations ( polymorphisms ) in two genes, the carriers of which show a life-threatening course of malaria less often. One of these genes controls the cell membrane pump for calcium, which is also found on erythrocytes, among other things, while the other plays a role in the sealing of blood vessel walls. Carriers of blood group 0 also have a reduced likelihood of a severe course of the disease.
Annual casualties and incidence
According to the World Health Organization (WHO) , almost half a million people die of malaria every year. 90% of the sick live on the African continent. According to the Robert Koch Institute, the number of malaria sufferers worldwide is estimated at 300–500 million cases. The WHO estimated the number of malaria cases in 2016 at 216 million.
In Germany, up to 2013, around 700 sick people were reported annually, of which 3–8 died (0.3–0.9%). The majority of the patients were in African endemic areas (approx. 87%).
| year | 1980 | 1981 | 1982 | 1983 | 1984 | 1985 |
|---|---|---|---|---|---|---|
| Reported cases in the Federal Republic of Germany with West Berlin | 573 | 393 | 514 | 447 | 482 | 530 |
| year | 1996 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reported cases in Germany |
> 1000 | 1008 | 931 | 800 | 1049 | 860 | 820 | 709 | 632 | 569 | 542 | 554 | 526 | 633 | 563 | 551 | 638 | 1007 | 1062 |
Pathogen
List of human pathogens
|
||||||||||||||||||||||||
| (* with insufficient malaria prophylaxis) |
The pathogen belongs to the apicomplexes . The pathogens Plasmodium falciparum , Plasmodium vivax , Plasmodium ovale , Plasmodium malariae and Plasmodium knowlesi , which can cause various forms of malaria, are dangerous for humans .
In addition, Plasmodium semi-oval can also cause malaria. In the case of multiple infections with the same or different plasmodia, the fever attacks can also be irregular. The otherwise regular, typical intermittent fever does not occur; there is an irregular and possibly permanent fever. Since the schizogonic cycle of P. knowlesi is 24 hours, this infection manifests itself in M. quotidiana with daily fever attacks.
Life cycle
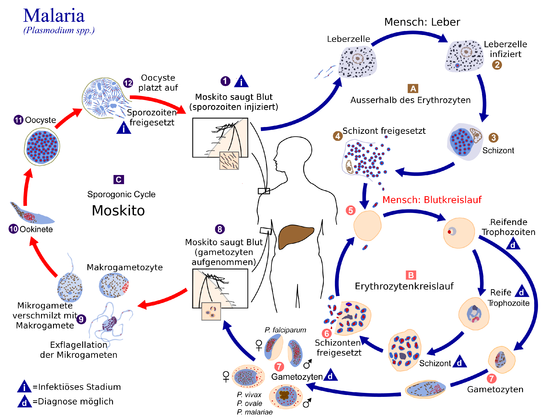
In the course of their life cycle, the pathogens causing malaria, the plasmodia, change hosts . The human being serves as an intermediate host . Mosquitoes, especially of the genus Anopheles, serve as final hosts . The plasmodia multiply in them.
In humans (asexual phase / schizogony )
After being bitten by an infected Anopheles mosquito, it secretes several hundred sporozoites with its saliva , which contains anticoagulants . These are carried with the bloodstream to the liver , where they penetrate the spleen and, above all, the cells of the liver tissue, where they mature into liver schizont. There they multiply (divide), called exoerythrocytic schizogony . This creates up to 30,000 merozoites . The schizont dissolves and gradually releases the merozoites into the bloodstream, enclosed in vesicles . In the case of Plasmodium vivax and Plasmodium ovale , not all merozoites go this way, a small part can survive as hypnozoite undivided in the liver cell. In this dormant state, they can remain undetected by the immune system for months to years. Due to an unknown stimulus, the hypnozoites mature into schizonts, which leads to characteristic relapses of tertian malaria.
The merozoites pass into the bloodstream and attach themselves to receptor molecules of red blood cells , whereupon they can penetrate these and are there enclosed within a membrane-bound, parasitophoric vacuole. Erythrocytic schizogony begins when the red blood cells become infected . The merozoites then mature into a trophozoite . At this stage, the pathogen appears as a ring around its own food vacuole with a dark-colored core at the edge. The throphozoite continues to mature into a schizont that feeds primarily on glucose and hemoglobin. This creates heme , which is immediately crystallized into hemozoin , since free heme is toxic to the trophozoite. After multiple division, the schizont gives rise to 6 to 36 merozoites, depending on the Plasmodium species. Due to their large amount, these cause the erythrocytes to burst and thus their distribution in the blood plasma. There, the merozoites can attack further erythrocytes and the asexual cycle begins again. After a short initial phase, the schizogony cycles are synchronized at regular intervals of 48 ( Plasmodium vivax, ovale, falciparum , but the latter unsynchronized) and 72 hours (Plasmodium malariae) . The fever following the destruction of the erythrocytes occurs every 3 or 4 days due to the synchronization of this cycle ( malaria tertiana and malaria quartana ). A small number of the merozoites develop into their sex forms, the gametocytes . These are then found in the blood, where they die off again after some time ( Plasmodium vivax : 1 day, Plasmodium falciparum : up to 22 days), provided they are not ingested by an Anopheles mosquito. The male gametocytes are called microgametocytes , the female macrogametocytes .
In the mosquito (sexual phase / sporogony )
When a mosquito bites again, the gametocytes are absorbed into the mosquito. They develop into gametes in their intestines . The microgamet penetrates the macrogamete and a zygote is created . This changes, takes on an elongated shape and becomes motile (= mobile), this cell is now called Ookinet . It accumulates between the layers of tissue in the mosquito intestine and turns into an oocyst there . Up to 1,000 new sporozoites are formed in it . After their release, they migrate into the mosquito's salivary glands and are now ready to be re-infected. The cycle in the Anopheles lasts between 8 and 16 days, depending on the outside temperature. A minimum temperature of 15 ° C is required. There is no cycle below this temperature .
Pathways of infection from person to person
Without going through a mosquito, malaria can be transmitted from person to person through the blood.
There are two known ways to do this:
- About the injured placenta of a pregnant woman during childbirth on her child.
- During a blood transfusion .
After the death of an 84-year-old on March 18, 2019 after an operation with blood transfusions the previous February in Carinthia, it was reported that, according to the prosecutor, malaria caused her death. The blood bags are traceable to the donors. Donors must indicate trips abroad and are not allowed to donate within 6 months of returning from an area affected by malaria. Donated blood has not yet been tested for malaria pathogens in Austria.
Pathogenesis
The red blood cells infected with plasmodia , maturing and bursting, release toxins (e.g. phospholipids ) with the merozoites , which in turn lead to the release of cytokines . The cytokines are mainly responsible for the rise in fever and an observed decrease in blood sugar level ( hypoglycaemia ). The hypoglycemia associated with lactic acidosis is not only caused by the action of the cytokines, but is also a consequence of the metabolism of the parasites . Likewise, if there is a high number of parasites in the blood (hyperparasitemia), anemia occurs due to the dissolution ( lysis ) of the red blood cells, the breakdown of affected red blood cells in the spleen and the dampening of erythropoiesis in the bone marrow due to the release of cytokines (especially due to the tumor necrosis factor alpha) .
In addition, there are important pathogenetic differences between Plasmodium falciparum and the other malaria pathogens .
Plasmodium falciparum
In the red blood cells, the trophozoite produces proteins such as Pf EMP1 (Plasmodium falciparum infected erythrocyte membrane protein 1) , which binds the infected blood cells to the endothelium of the blood vessels . The associated microcirculation disorders explain, at least in part, the significantly more severe course of Malaria tropica caused by Plasmodium falciparum .
The adhesion of the red blood cells to the endothelium and the lack of deformability of the affected cells lead to a narrowing of the capillaries and thus to a disruption of the oxygen and nutrient supply to the environment. This has particularly dramatic effects in the central nervous system and the frequent central complications of tropical malaria. Young children in particular can fall into a life-threatening coma (cerebral malaria).
Remaining plasmodia
The other types of plasmodia are unable to adhere to the endothelium, which explains the lower number of circulatory disorders and thus the low level of danger. Plasmodium malariae differs from the other human-pathogenic Plasmodia in that it occasionally affects other higher primates.
Clinical picture, symptoms
The signs and symptoms of malaria typically begin 8-25 days after infection, but can appear later in those who have not taken adequate antimalarial drugs as prevention. Common to all types of malaria, early forms of the disease resemble flu-like symptoms and may resemble other conditions such as sepsis , gastroenteritis, and viral diseases . Symptoms can include headache, fever, tremors, joint pain, vomiting, hemolytic anemia , jaundice , hemoglobin in the urine, retinal disorders, and convulsions.
The classic symptom of malaria is paroxysm - a cyclical occurrence of sudden perceived cold, followed by tremors, and then fever and sweating that occurs every two days for P. vivax and P. ovale infections and every three days for P. malariae . The P. falciparum infection can cause all 36-48 hours a recurring fever or a less pronounced and almost continuous fever.
Severe malaria is usually caused by P. falciparum (often referred to as falciparum malaria). Symptoms of Falciparum malaria appear 9-30 days after infection. People with cerebral malaria often have neurological symptoms, including abnormal posture, nystagmus , paralysis (failure of the eyes to turn in the same direction), opisthotonus , seizures, or coma.
Complications
Malaria has several serious complications. This includes the development of respiratory distress, which occurs in up to 25% of adults and 40% of children with severe P. falciparum malaria. Possible causes are respiratory compensation in metabolic acidosis, non-cardiogenic pulmonary edema, accompanying pneumonia, and severe anemia . Although rare in young children with severe malaria, acute respiratory distress syndrome occurs in 5-25% of adults and up to 29% of pregnant women. HIV co-infection with malaria increases mortality. Kidney failure is a feature of blackwater fever in which hemoglobin from lysed red blood cells passes into the urine.
Infection with P. falciparum can lead to cerebral malaria, a form of severe malaria that includes encephalopathy . It is associated with retinal brightening, which can be a useful clinical sign in differentiating malaria from other causes of fever. An enlarged spleen, an enlarged liver, or both, severe headache, low blood sugar and hemoglobin in the urine with kidney failure may occur. Complications can include spontaneous bleeding, coagulopathy, and shock. Malaria in pregnant women is an important cause of stillbirths, infant mortality, abortion and low birth weight, especially in P. falciparum infections, but also in P. vivax .
Due to the different course of the disease can range from the P. falciparum malaria , the malaria vivax and quartan malaria are distinguished. The malaria tropica is the most severe form of malaria.
Malaria tropica
The malaria or short Tropica (because of its often fatal outcome and Malaria pernicious and tertian malignant is called) by the pathogen Plasmodium falciparum (formerly immaculatum Plasmodium called) causes and is in Europe the most common form of malaria entrained. Characteristic of the complicated, life-threatening malaria tropica are the chills and the high level of parasitemia (with a proportion of at least 5% parasites in the blood), the sometimes pronounced anemia and the frequently occurring neurological complications . There may be a rhythmic fever. However, a lack of fever rhythm is not a criterion for excluding tropical malaria .
incubation period
There is an average of twelve (7 to 14) days between the bite of the Anopheles mosquito and the outbreak of the disease. Significantly shorter time intervals occur in the case of an infection with blood containing pathogens. Longer incubation times are possible with insufficient chemoprophylaxis .
fever
The typical alternating hemorrhagic fever with chills when the fever rises and sweats when the temperature rises, as occurs with other forms of malaria, is usually not observed in tropical malaria . Therefore, malaria, particularly tropic malaria , cannot be ruled out simply because there is no typical fever rhythm. A high fever above 39.5 ° C often occurs in children and is to be assessed as having a poor prognosis. Central complications and coma are common .
Neurological Complications
Disturbances in consciousness , which can even lead to a coma , represent a typical and also life-threatening complication of tropical malaria . Sudden changes in the state of consciousness without a sign are quite possible. The patient may also slowly become cloudy. Neurological focus symptoms such as paralysis and seizures can also occur in the context of cerebral malaria . Normal neurological diagnostics hardly lead to an adequate diagnosis here. A high number of parasites in the blood is a crucial indicator.
In pregnant women and children, hypoglycaemia can occur, which alone or with the central problem can lead to coma.
anemia
Anemia is common in severe infections and is one of the signs of complicated malaria when the hemoglobin is below 8 g / dL. Babies and toddlers represent a special risk group for severe anemia. Mostly it is a hemolytic anemia caused by the destruction of red blood cells. As mentioned above, the inhibition of erythropoiesis is also of some importance. The severity of the anemia correlates strongly with the extent of the parasite infestation.
Hemoglobinuria
The increased hemoglobin level in the blood as a result of the massive hemolysis leads to hemoglobinuria (hence the former name blackwater fever , which was mainly observed in malaria tropica after the use of chinin), the excretion of hemoglobin via the kidneys . The resulting increase in the hemoglobin content in the urine colors it significantly darker. Hemoglobinuria, visible to the naked eye, is one of the criteria for complicated malaria and can lead to acute kidney failure . The treatment of blackwater fever includes the discontinuation of quinine preparations and the administration of chloroquine .
Changes in other organ systems

In the course of the disease, malaria can lead to an enlargement of the spleen ( splenomegaly , " spleen tumor") due to the large number of debris of red blood cells that needs to be broken down there. In rare cases, the tissue growth leads to tension in the capsule so that it can easily tear ( rupture of the spleen ). Symptoms affecting the gastrointestinal tract, such as diarrhea, are frequent and important from a differential diagnosis , as they can lead to the wrong diagnosis of bacterial enteritis if the fever is absent or has a weak degree .
In up to ten percent of cases, lung involvement can occur, which can range from mild symptoms to pulmonary edema as a criterion for complicated malaria.
It is not uncommon for a circulatory disorder in the kidneys to lead to acute kidney failure . Kidney failure (with a creatinine level of over 250 µmol / L) is one of the criteria for complicated malaria. After the infection has healed, the kidney usually recovers.
Usually thrombocytopenia can be detected.
Malaria tertiana
Tertiana malaria, which is less common than tropicana malaria (also known as Tertiana for short , previously also called third day fever , called "alternating fever in malaria with a fever-free interval of one day") is caused by the pathogens Plasmodium vivax and Plasmodium ovale . It is one of the benign forms of malaria disease. Compared to tropical malaria there are hardly any complications. The main problem is to differentiate the unspecific preliminary symptoms from the life-threatening malaria tropica . This is usually only possible with microscopic diagnostics.
incubation period
The incubation period is between 12 and 18 (between 9 and 21) days, but can also last several months if the course of the infection is slowed down by chemoprophylaxis .
fever
After an unspecific prodromal phase of a few days, the typical three-day fever rhythm, which gave tertian malaria its name, usually sets in , ie on the first and third day there is a fever attack. There is usually a fever attack within each 48-hour period.
The fever attacks usually obey the following scheme:
- Frost stage (1 hour): The patient suffers from chills and a subjective feeling of extreme cold. In this phase the temperature rises steeply.
- Heat stage (4 hours): The skin often burns excruciatingly. There is severe nausea , vomiting, and fatigue. The temperature can be over 40 ° C. In contrast to the next stage, the skin is mostly dry.
- Sweat stage (3 hours): With profuse sweating, the temperature sinks to the normal value of 37 ° C, the fatigue subsides before the defervescence.
As with all other forms of malaria, the lack of a fever rhythm is by no means sufficient to rule out the disease.
Quartana malaria
Quartana malaria (also Quartana , from febris quartana , and four-day fever , formerly also called fourth -day fever ; outdated German term: "Quartan fever") is caused by the pathogen Plasmodium malariae , which is rare today, particularly in Africa and Southeast Asia . Again, it is a severe, febrile, but rarely fatal form of malaria. A characteristic complication is the nephrotic syndrome . What is special about this form is that even after more than 50 years, relapses can still occur. The incubation time is also considerably longer than for the other two forms.
incubation period
The incubation period is between 16 and 50 (usually between 19 and 41) days. It is therefore considerably longer than with the other forms of the disease.
fever
The prodromal phase is just as unspecific as that of malaria tertiana . After just a few days, the fever develops a four-day rhythm. After a day with a fever, two fever-free days can be observed before fever again follows on the fourth day. The sequence of stages (frost-heat-sweat) on the fever day corresponds to malaria tertiana . The same applies here: a lack of fever rhythm does not rule out the diagnosis of malaria. There is usually a fever attack within every 72 hour period.
Kidney involvement
In the course of quartana malaria , severe kidney involvement can occur. This is known as malaria nephrosis , among other things . It is a nephrotic syndrome with the following symptoms:
- low serum protein albumin (partly responsible for regulating the water balance in the bloodstream)
- Water accumulation in the connective tissue ( edema ) and the abdominal cavity ( ascites ) due to the lack of albumin
- increased serum cholesterol
Epidemiological studies have shown that this complication occurs more frequently in children between the ages of two and ten in tropical Africa .
Recurrences
As mentioned above, during the life cycle of Plasmodium vivax and Plasmodium oval resting forms, the so-called hypnozoites , develop . They can be the reason for the disease to break out again after a period of rest of months or years. This does not necessarily have to be preceded by a known history of malaria. The recurrences are particularly treacherous because often neither the patient nor the doctor establishes a connection with malaria. The special thing about Plasmodium malariae are the relapses after a particularly long disease-free interval (several years). Relapses after disease-free disease of more than 50 years have been described. The relapses are not caused by hypnozoites in the liver (there are no hypnozoite forms of Plasmodium malariae ), but by persistent parasite infestation in the blood. This is so small that it usually cannot be detected microscopically. This is of great clinical importance, especially in transfusion medicine in endemic areas , since malaria transmission can occur even with negative donors if fresh blood is used. Conserved blood, on the other hand, is stored refrigerated, which kills malaria pathogens. However, recurrences can usually be prevented in the long term by drug measures (primarily with the use of primaquine ).
Diagnosis
The information that is helpful prior to therapy includes details of the travel destination, existing prophylaxis and previous illnesses.
The diagnosis of malaria should be confirmed with the help of laboratory diagnostic methods for parasitological species differentiation and determination of the number of parasites. In practice, the most important and cheapest method for suspected malaria is the microscopic examination of normal blood smears ( thin drops ) and the up to 10-fold enriched thick drops using Giemsa staining for plasmodia. A differentiation of the four plasmodia is possible on the basis of morphological criteria (see Maurerian stain or Schüffner's stippling ). The number of parasites and leukocytes determined is a measure of the severity of the disease. However, a negative result of the microscopic examination cannot rule out malaria due to the low sensitivity of this method.
Alternatively, the malaria pathogens can be detected immunologically and molecularly biologically . The malaria rapid tests available (e.g. ICT Malaria PF-Test, OptiMal-Test) are based on the detection of parasite- specific antigens . However, a negative result cannot rule out malaria even with these tests. By far the most sensitive method for malaria diagnosis is the polymerase chain reaction (PCR). However, due to the high expenditure of material and time, it is not very suitable for acute cases.
General examinations may also be part of the diagnostics (laboratory to determine blood counts, liver and kidney functions, blood gas analysis, assessment of the lungs with an X-ray and the spleen with ultrasound and an EKG).
Prevention and treatment
Since there is no one hundred percent protection against malaria (no possibility of vaccinating against malaria), the risk of malaria should be reduced. The most effective protection is not to travel to areas where malaria is transmitted ( endemic areas ). Since this is not always possible, avoiding insect bites ( exposure prophylaxis ) is the most important element of malaria prevention. In addition, preventive intake ( chemoprophylaxis ) or carry along (stand-by therapy) of malaria medication should reduce the risk of developing severe malaria.
Regardless of whether chemoprophylaxis or stand-by therapy was chosen, a doctor must be consulted immediately for any unclear fever in the tropics and for a long time after return. This should confirm or rule out the suspicion of malaria as quickly as possible by means of a suitable blood test, as tropica malaria that is not treated in time can be fatal.
Spontaneous healing occurs in malaria tropica after a maximum of eight months, in malaria tertiana after a maximum of three years. Quartana malaria does not have a definite spontaneous cure.
vaccination
No vaccine is currently available. Research has been going on in this area for years and several vaccine candidates have been developed. The RTS, S vaccine has been piloted since April and September 2019 in Malawi, Ghana and Kenya. A number of other vaccine candidates are in clinical trials. These also include vaccinations with attenuated live parasites or those based on mRNA (see research ).
Insect repellent
The insect repellent (as exposure prophylaxis ) is the most important part of malaria prevention. This includes wearing light-colored, skin-covering, long clothing, staying in mosquito-proof rooms (especially at night; air conditioning, fly screens, mosquito nets ) and treating skin and clothing with mosquito- repellent agents, so-called repellants (e.g. Icaridin or DEET ). The additional use of insecticides in sprays (above all pyrethroids ), vaporizers, incense coils (“mosquito coils”) and the like can offer additional protection. However, many travelers still do not protect themselves consistently against mosquitoes. A study published in France in April 2006 showed that less than 10% of patients suffering from malaria had used measures to repel insects.
Chemoprophylaxis and therapy
In particular, the treatment of life-threatening tropical malaria should be carried out as quickly as possible and in the hospital. Tertiana malaria and the rare quartana malaria are also serious febrile illnesses, but they are rarely fatal.
For many travel destinations, it is sufficient to carry a medication for emergency self-treatment (stand-by therapy) in the event of an actual illness. Nevertheless, chemoprophylaxis (long-term use of anti-malarial drugs) taking into account possible drug side effects and taking into account the personal health situation (previous illnesses, immune status, ...) is often recommended when traveling to malaria areas with a high risk of infection.
The cinchona bark and the quinine obtained from it have been used for the treatment of malaria since the 17th century - legend has it that British colonialists therefore regularly drank tonic water with a high content of quinine and, in order to improve the then very bitter taste, often mixed it with gin and so invented the gin and tonic . Since the middle of the 20th century, the therapy options have multiplied and drug prevention is possible (chemoprophylaxis). The greatest problem with drug prevention and treatment is the increasing resistance of the pathogen, especially Plasmodium falciparum. In addition, the risk of malaria must always be weighed against the risk of serious drug side effects. The German Society for Tropical Medicine and International Health e. V. recommends as a rule (as of 2018):
- In areas with a medium or low risk of malaria (e.g. Central America, Southeast Asia and South America without high-risk areas): no prophylaxis, emergency therapy with artemether - lumefantrine or atovaquone-proguanil in the event of illness .
- In areas with a high risk of malaria and known resistance (e.g. high-risk areas in Africa , New Guinea , the Solomon Islands , in the interior of French Guiana , Suriname and Guyana ): Prophylaxis with atovaquone proguanil , doxycycline or (if there is a justified medical indication and under Observance of the special warnings) Mefloquine .
- In areas with very low risk (e.g. Egypt , Paraguay ): no prophylaxis, no emergency therapy, if you have a fever, consult a doctor and advise you to travel.
There are also quinine (for therapy, especially in the case of complicated tropic malaria; only under medical supervision), dihydroartemisinin-piperaquine (for treatment; only under medical supervision), primaquine (therapy for tertian malaria or quartana malaria; prevents recurrences ; use for Prophylaxis only in exceptional cases ) and Proguanil (prophylaxis; mostly in combination with chloroquine ; use only in exceptional cases).
In the early 1970s, the Chinese scientist Tu Youyou chemically isolated the artemisinin , a secondary plant substance , a sesquiterpene , which occurs in the leaves and flowers of the annual mugwort ( Artemisia annua ). In the following decades she demonstrated the effectiveness of this substance against malaria. For this she was awarded the Albert Lasker Award for Clinical Medical Research in 2011 and the Nobel Prize for Physiology or Medicine in 2015. Artemisinin-containing preparations (including their derivatives Artemether , Artesunate , Arteflene and Artemotil ) are therefore used primarily in China, Southeast Asia and Africa . These preparations, used as part of a combination therapy ( artemisinin-based combination therapy ), are recommended by the WHO as the first choice for the acute treatment of malaria. In Germany, the fixed combination of artemether-lumefantrine and dihydroartemisinin-piperaquine is used. Artesunate, which is not on the market in Germany but can be imported if necessary, is also recommended as the treatment of choice for the complex malaria tropica. If artesunate is unavailable, quinine can be used if necessary.
The stand-by therapeutics halofantrine and amodiaquine have meanwhile been withdrawn from the market in Europe due to severe side effects, but are still occasionally available as emergency medication in malaria areas. Halofantrine has been associated with cardiac arrhythmias , while amodiaquine therapy increased liver damage and damage to the blood picture ( agranulocytosis , aplastic anemia ).
The combination of sulfadoxine and pyrimethamine is still partly available, particularly in endemic areas . However, this drug combination was withdrawn from the market in Germany due to severe skin reactions ( Stevens-Johnson syndrome ). In addition, there are many malaria pathogens that are resistant to this combination of active ingredients.
The first step in treating malaria is to remove the asexual parasites in the blood. The WHO recommends chloroquine or artemisinin-based combination therapy for infection with Plasmodium vivax. After that, however, there are dormant hypnozoites in the liver that can trigger recurrences. Tafenoquine can be used to eliminate the hypnozoites . Since tafenoquine has a half-life of around 15 days, a single dose is sufficient. With a single administration of 300 mg tafenoquine in combination with 1500 mg chloroquine for 3 days, if infection with Plasmodium vivax has been proven, a relapse-free rate of 62.4% was achieved after 6 months. After chloroquine alone, only 27.7% were free of recurrences after 6 months.
It is important to find out about the current risk and resistance situation in good time before each trip and to plan personal preventive care with a doctor experienced in tropical medicine.
Drug resistance in malaria tropica is widespread worldwide; especially in Southeast Asia and Oceania also with malaria tertiana, in which a follow-up treatment of the persistent liver forms (hypnozoites) is necessary.
| therapy | M. quartana | M. tertiana | M. tropica, Knowlesi-M. | complicated course |
|---|---|---|---|---|
| Chemoprophylaxis | Atovaquone proguanil , doxycycline , mefloquine | |||
| Stand-by medication | Atovaquone-Proguanil, Artemether - Lumefantrine | |||
| 1st Choice | Chloroquine | Atovaquone-Proguanil, Artemether-Lumefantrine, Dihydroartemisinin-Piperaquine (the latter not in M. tertiana) | Artesunate iv | |
| after initial therapy | Primaquine to kill permanent forms (hypnozoites) | oral therapy according to the pathogen | ||
Vector control
The attempt to prevent new infections through targeted control of the Anopheles mosquito is called vector control (combating the vector). For this purpose, insecticides are sprayed into people's homes or the use of insecticide-impregnated bed nets (IIB) is propagated.
In the 1950s and 1960s, under the leadership of the WHO, attempts were made to eradicate malaria as part of the Global Eradication of Malaria Program . An important part of the campaign was spraying the interior walls of all apartments and houses with DDT . The test area Sardinia was cleared of malaria in 1950 without eradicating the vector. Despite the initial success, the project was discontinued in the early 1970s as a failure.
The use of DDT in residential buildings (interior spraying) is controversial. The increase in resistance to DDT can limit its effectiveness. Spreading DDT indoors can pose health risks: there is evidence that DDT may increase the risk of miscarriages or malformations, decrease semen quality in men, or be involved in various forms of cancer . Long-term studies on rats, mice and hamsters have demonstrated the carcinogenic effects of technical DDT with the formation of tumors in the liver, lungs and the lymphatic system , and the WHO International Agency for Research on Cancer (IARC) classified DDT in 2015 as “probably carcinogenic in humans “(Group 2A). Today the manufacture and use of DDT is only permitted in a few countries around the world for the purpose of combating disease vectors. But even these approvals are gradually being withdrawn. For example, India plans to end its use by 2020 as the last major user of DDT to fight malaria.
Reporting requirement
In Germany, the pathogen Plasmodium sp. not to be reported by name in accordance with Section 7 (3) of the Infection Protection Act (IfSG) . Laboratories etc. are required to report ( Section 8 IfSG).
In Austria, malaria is a notifiable disease in accordance with Section 1 (1) No. 2 of the 1950 Epidemic Act . Cases of illness and death must be reported. Doctors and laboratories, among others, are obliged to report this ( Section 3 Epidemics Act).
In Switzerland there is mandatory reporting of malaria in terms of a positive laboratory analytical finding by the attending physician. In addition, if the laboratory results are positive for the Plasmodium spp. by the testing laboratory. This results from the Epidemics Act (EpG) in conjunction with the Epidemics Ordinance and Annex 1 or Annex 3 of the Ordinance of the FDHA on the reporting of observations of communicable diseases in humans .
research
Therapeutic approaches
The base sequences in the genomes of Plasmodium falciparum and Anopheles gambiae were completely deciphered in autumn 2002. At about the same time, new anti-malarial drugs, such as B. atovaquone, lumefantrine and the active ingredients artesunate and artemether, derived from the natural substance artemisinin , were brought onto the market. The first promising results of the treatment of malaria sufferers with tafenoquine and the antibiotic fosmidomycin were also presented. Fosmidomycin blocks the MEP pathway ( methylerythritol phosphate pathway ), a metabolic pathway to dimethylallyl pyrophosphate (DMAPP). Plasmodia use the MEP pathway, but not humans. As a result of its blockage, important cellular building blocks emanating from the DMAPP can no longer be synthesized in cell membranes and cell anchors of the pathogen.
Attempts to develop a globally effective vaccine against malaria have so far failed, despite some initial successes. The biggest problem in developing an effective vaccine is the high variability of the malaria antigens . Defused living pathogens in which the UIS3 gene has been eliminated promise new hope . These sporozoites were injected into mice, which produced no forms of plasmodia that could have changed from the liver (whose infestation does not cause symptoms) to the red blood cells . The result of the immune reaction was impressive: not a single vaccinated mouse became infected with normal plasmodia after infection, while everyone in the control group became ill.
RTS, S ("Mosquirix") has been in development since 1987. This is another vaccine that consists of the hepatitis B vaccine, hepatitis B virus (RTS, S ), which also contains components ( RT S, S) of the circumsporozoite protein on the surface of the Plasmodium falciparum sporozoite and another surface -Antigen (RT S , S) of the hepatitis B virus carries. This triggers an immune response that fights the plasmodia at an early stage, before they infect the liver. In addition, vaccination against the hepatitis B virus is induced. For complete immune protection, it is planned to combine the vaccine with other antigens of the malaria pathogen. GlaxoSmithKline conducted a key study with RTS, S in 2010 . The evaluation of a randomized double-blind study that included more than 15,400 children showed, after one year, a preliminary result in a group of patients vaccinated with RTS, S, a reduction in malaria cases by about half compared to the control group; for the subgroup of severe gradients the difference is about 5% smaller. The client GlaxoSmithKline has assessed the results of a clinical phase III study as positive and, on this basis, applied for a so-called “regulatory application” to the European Medicines Agency ( EMA) in July 2014 . A recommendation by the WHO at the end of 2015 [out of date] is thus possible. After the publication of further study results in April 2015, the immunologists Vasee Moorthy and Jean-Marie Okwo-Bele (both WHO) consider the efficacy and tolerability as definitely confirmed.
As a study carried out on mice in 2012 showed, vaccines of this type (stimulation of the immune system to prevent the plasmodia from penetrating the red blood cells) can lead to the development of particularly aggressive strains of pathogen with significantly more severe disease.
In 2013, US researchers succeeded in cultivating Plasmodium falciparum in such a way that a vaccine can be made from it.
An alternative therapeutic approach could use an antibody against plasmodia in the form of passive immunization .
Another approach of current research is to prevent plasmodia from multiplying. Studies on mice have shown that it is in principle possible to use a vaccine to block the fusion of female and male germ cells of the Plasmodium and thus to curb the spread of the pathogen.
Another way to fight malaria is to break the chain of infection by fighting the Anopheles mosquito. A corresponding attempt to eradicate malaria in the 1960s with the help of DDT ( dichlorodiphenyltrichloroethane ) was only locally and temporarily successful; In the period that followed, environmentally harmful effects became apparent. A new approach is the use of the bacterium Bacillus thuringiensis israelensis (bti), which can easily be propagated in the laboratory (see Bacillus thuringiensis ). Bti has been tried and tested against mosquitoes and is highly effective, but when used correctly it is largely gentle on "non-target organisms". For use, Bti spores are spread in waters inhabited by Anopheles larvae. The larvae ingest the bacteria with their food. In your gut, digestive enzymes release a delta-endotoxin from the spore wall; this protein kills cells in the intestinal wall by creating cation-permeable pores in their membrane. The insects then stop eating and die while still in the larval stage. Bti is available commercially in liquid, tablet, powder and granular form. The use of granules has proven its worth for large-scale outdoor use; if water is heavily contaminated, it is brought out by helicopter.
In addition, the joint department of the IAEA and FAO is researching a novel method to control the Anopheles mosquito by exposing sterile male mosquitoes on a massive scale ( sterile insect technique ).
In view of the increasing resistance to the active ingredients developed in recent decades, the synergistic effect of the long-known active ingredients methylene blue and chloroquine has been in the focus of research since 2002 .
In collaboration with the WHO, the Kenya Medical Research Institute and the British University of Oxford are currently developing world maps available on the Internet on which all knowledge about the spread of malaria is collated (e.g. infection rate Plasmodium falciparum , Plasmodium vivax ). This venture, known as the Malaria Atlas Project , is funded by the English Wellcome Trust and is constantly expanding.
A new therapeutic approach is the fight against Plasmodium in the mosquito intestine using genetically modified mosquito intestinal flora. The bacterium Pantoea agglomerans , which lives in symbiosis with Anopheles , is modified in such a way that it secretes peptides effective against the parasite. This approach can greatly reduce the prevalence of infected mosquitoes.
In a study, antibodies against a previously unknown antigen PfSEA-1 were discovered in the blood of young children from Tanzania , which apparently protects them from a severe form of malaria. The newly discovered antigen PfSEA-1 helps the malaria parasite reproduce in the blood by allowing it to leave the red blood cells and attack other blood cells. The newly discovered antibodies against the PfSEA-1 antigen can prevent precisely this effect. Studies have shown this natural protective factor in around six percent of more than 450 children, and none of these sufferers developed severe malaria. These findings were then tested on around 140 young adults from neighboring Kenya. It turned out that in people with the antibody against PfSEA-1, the parasite density in the blood was reduced by about half. On average, 56 out of 100 adults in this age group had such antibodies. The researchers suspect that contact with the pathogen stimulates the production of the protective protein, which could also explain why malaria in these countries tends to be less severe in adults than in children.
At the beginning of 2014, the University of Edinburgh and the biotech company CILIAN AG announced that they had discovered a vaccine that covered a large number of gene variants of the malaria pathogen and had caused a strong immune reaction in animals. The production of this active ingredient takes place through biotechnical processing of single cells.
The synthetic spirotetrahydro-β-carboline derivative with the provisional name KAE609 (previously NITD609) was developed by Novartis and showed good dose-dependent antimalarial activity against asexual and sexual stages of Plasmodium falciparum and Plasmodium vivax in a phase II study at three centers in Thailand . A median parasite clearance was found after twelve hours. This spiroindolone analog inhibits the Na + -ATPase located in the parasite plasma membrane , which is important for sodium and osmotic cell homeostasis.
Distributed computing
There are currently (as of August 2013) several non-commercial projects of distributed computing for the search for new drugs or effective countermeasures. Private individuals can make the excess computing time of their computer available.
The world community grid project GO Fight Against Malaria was successfully completed in mid-2013; the data evaluation is still ongoing as of July 2014, the project initiators assess the first results as “very promising” and have also led to a scientific publication. The projects FightMalaria @ Home and Malaria Control are currently active .
Body odor in sick people
Several studies have shown that an infection with Plasmodium changes the body odor of the infected in such a way that the Plasmodium- transmitting insects are more attracted to the infected. This can contribute to the rapid and effective spread of the pathogen.
Poverty-Related Illness
Malaria is also known as a poverty-related disease . This term is based on the one hand on the fact that the disease mainly affects poor people who have little purchasing power and consequently do not form an attractive market. It makes more economic sense for pharmaceutical companies to research drugs against diseases that are less “urgent” in medical terms, and those affected by those who have more purchasing power.
Norbert Blüm wrote in 2003:
“Worldwide, the pharmaceutical industry spends twice as much research on the fight against hair loss and erectile dysfunction as it does against malaria, yellow fever and schistosomiasis . This is consistent with the market economy, because customers with erectile dysfunction and hair loss generally have more purchasing power than those suffering from malaria and yellow fever. "
In response to this mechanism, the European Union wants to support the development of funds against poverty-related diseases with 600 million euros.
On the other hand, it is questionable whether, especially for regions in which malaria and poverty are widespread, the fight against malaria by developing a vaccine should be a priority. Parasitologist Paul Prociv points out that constant reinfection makes adults in malarial areas virtually immune to the disease. Priority would be given to improving general health care and living conditions. A malaria vaccine would mainly benefit western visitors to the tropics who shy away from the side effects of conventional malaria prevention.
Malaria can also be considered a poverty-related disease, as in many countries of the so-called Third World the living conditions of most people do not meet the standards for preventing infection (closed living rooms, mosquito nets, air conditioning, insect sprays, etc.), chemoprophylaxis is not available and drugs are expensive and difficult must be obtained (see also section Prevention and Treatment ).
Due to the lack of financial support, Bill Gates announced in late October 2005 that he would be providing a sum of 258.3 million dollars to promote malaria research. In his opinion, "it is a shame for the world that the number of malaria-related deaths has doubled in the last 20 years, especially since action against that disease could be very strong."
Economic impact
According to Jeffrey Sachs , tropical diseases , but especially malaria, are a main cause of the economic misery of the poorest countries on earth: where this disease occurs, especially in the tropics and subtropics , there is also poverty . In the mid-1990s, countries affected by malaria had an average national income of around US $ 1,500 per capita, while unaffected countries had an average of more than five times that with an average of US $ 8,200. Malaria economies grew by an average of only 0.4 percent a year between 1965 and 1990, while the others grew by 2.3 percent. The economic damage caused by the disease for Africa alone is estimated at around 9.54 billion euros per year.
According to studies, the paralysis of the economies of the affected countries caused by malaria is not only due to the direct costs of drugs and medical treatment. Malaria has a negative impact on labor productivity and thus on the country's gross domestic product , which means that necessary investments, such as in education , are not made. In addition, foreign investors avoid such countries as do tourists and trading companies.
Meanwhile, AIDS has dramatically worsened the unfavorable situation for these countries.
history
The earliest reports of malaria epidemics come from the ancient Egyptians (including from the Ebers papyrus ). The oldest DNA finds were recently found by Munich pathologists around Andreas Nerlich in two Egyptian mummies from Thebes, which are around 3500 years old. But interchangeable fever also appears as the “queen of diseases” in Indian scriptures that are around 3000 years old. The Chinese even had an antidote over 2000 years ago. They used the annual mugwort (青蒿, qīnghāo). In modern times, researchers have actually been able to isolate an active substance from this plant: artemisinin ( Qinghaosu in Chinese ).
In ancient times , malaria spread around the Mediterranean . Hippocrates recognized that people from swamp areas were particularly often affected by malignant marsh fever, but he suspected or suspected the Hippocratic doctors that drinking stale swamp water brought the body fluids into an imbalance (see humoral pathology ). At that time, nothing was known about invisible pathogens. The founder of the humoral pathology Polybos assumed an excess of yellow bile as the cause of all types of fever . In Rome, Galenus expanded the ancient fever theory further and assigned the “Quartana” to the excess of black bile and the “Tertiana” to yellow bile . A form of fever with daily flare-ups ( febris quotidiana , daily fever ) has been considered to be caused by excessive or corrupted phlegm since Galenus . In Hippocrates and later, a febris quintana ( five-day fever , Quintana ) was reported, which can be interpreted as a misinterpreted form of malaria such as Volhyn fever . The Roman Empire was also regularly hit by severe malaria epidemics. Some historians even assume that they are one of the decisive factors for the fall of the Roman Empire. A mass children's grave with over 50 bodies was discovered near Rome, which was dated to the year 50. The DNA of Plasmodium falciparum was isolated from the bones of these children's skeletons .
Around 1560, the Italian anatomist Giovanni Filippo Ingrassias (around 1510-1580) , who worked in Palermo as Protomedicus, tried to fight malaria by draining swamps.
From the Middle Ages to the middle of the 20th century, malaria was not only widespread in southern but also in central Europe. Large areas of Italy in particular were plagued by malaria until the 20th century. In the German-speaking area, malaria was primarily to be found in the Upper Rhine and the Lake Constance area. In northern Germany the intermittent fever was also known as marsh fever . Famous European malaria patients were Albrecht Dürer (although the course of the disease raises doubts as to whether it was really a malaria disease), Oliver Cromwell , Friedrich Schiller and Johann Gottfried Tulla . While malaria was still widespread in Germany in the middle of the 19th century , the number of people suffering from it fell sharply towards the end of the century , as evidenced by information provided by Robert Koch . It was only through the systematic drainage of wetlands and the systematic use of insecticides that malaria could be eradicated in Europe in the 1960s.
The first cases of malaria from North and South America were not documented until the 16th century. Today it is assumed that it was brought there by the Europeans or by the slave trade they organized . The pathogen spread there very quickly: At the beginning of the 20th century, for example, one percent of the population in the southern United States died of malaria every year, and in the marshlands of the Mississippi the mortality rate was as high as three percent. The remedy that is still used today, however, also originated in South America. Peruvian workers successfully combated fever with the bark of a tree belonging to the red family , which also includes the coffee plant . Members of the Jesuit order observed this effect and first brought the powder to Europe in 1640, where it was also called "Jesuit powder". The tree was later known as " cinchona bark known" (Cinchonia), the drug as " quinine ". Quinine has an extremely bitter taste. It is used as a flavoring for tonic water and bitter lemon . The legend that drinking gin and tonic regularly protects against malaria continues to this day. However, the quinine concentration in a gin and tonic drink is far too low these days.
Like Russian military doctors in Moldova in 1853 , German military doctors treated intermittent fever with quinine from 1914 to 1918 (e.g. in Albania). Since there were also unsuccessful treatments, they combined with neosalvar therapy .
The malaria pathogen in the form of plasmodia was discovered on November 6, 1880 by the French Alphonse Laveran , who worked at the military hospital in Constantine ( Algeria ). For this he received the Nobel Prize in Medicine in 1907 .
Ronald Ross , surgeon and general from England, discovered the connection between the malaria pathogen and the bite of the anopheles mosquito in 1897 and was awarded the Nobel Prize for Medicine in 1902 . Incidentally, the ancient Egyptians had the connection between mosquitoes and malaria as early as 3000 BC. Recognized. It was seen as the curse of the gods or the Nile .
Julius Wagner-Jauregg infected some of his patients with malaria in 1917 in order to treat the progressive paralysis with the fever attacks that occurred . This so-called malaria therapy proved to be successful and was practiced until the advent of antibiotics , in 1927 Wagner-Jauregg received the Nobel Prize for Medicine for it. Due to the associated risks, the use of malaria as a therapeutic agent is no longer justifiable.
In 1934, Hans Andersag succeeded in discovering chloroquine (called Resochin), a very effective active ingredient against malaria, in the Bayer laboratory in Wuppertal-Elberfeld (at the time part of IG Farbenindustrie AG).
One of the last malaria epidemics occurred in Berlin in 1946; it was based on infected soldiers from Africa and south-east Europe.
In the 1950s, the WHO started the Global Eradication of Malaria Program . New infections from mosquito bites should be prevented by spraying the inside walls of the houses with DDT solution. At the same time, those who are already sick should be treated with chloroquine in order to combat the actual pathogen, the plasmodia .
The campaign was only partially successful. In the Netherlands, Italy, Poland, Hungary, Portugal, Spain, Bulgaria, Romania and Yugoslavia, malaria was permanently eradicated by the late 1960s. The number of new infections with malaria has also been drastically reduced in many countries in Asia and South and Central America. Here, after initial successes, money and medical staff were often withdrawn from the anti-malaria campaigns and used elsewhere. As a result, new cases of malaria remained undetected or could not be adequately treated. Over the years, DDT resistance has emerged in various species of the anopheles mosquito. In addition, some of the plasmodia had become resistant to chloroquine. The WHO officially closed its program to eradicate malaria in 1972 as a failure.
In 1971, the Chinese Tu Youyou isolated the phytochemicals artemisinin used to treat malaria from the annual mugwort (Artemisia annua, Chinese: Qinghao) and was awarded the Nobel Prize for Medicine in 2015.
In 2007, the WHO decided to World Malaria Day (World Malaria Day), a day of action, which takes place annually on the 25th of April.
See also
- Pathogen / carrier: Human parasites , sporozoa , protozoal infection
-
Control: mosquito net , cinnamon oil , DDT , heptachlor
- Herbal remedies: sorrel family , Artemisia (genus) or annual mugwort ( artemisinin ), also: blue monkshood , yellow gentian , cannabis , blackthorn acacia , common boxwood , African baobab
- Medicines: primaquine , sulfonamide , tetracyclines
- Immunity: sickle cell anemia ( erythrocyte ), favism ( G6PD deficiency ), immunity (medicine)
- European Mosquito Control Association
literature
Guidelines
- Guideline Malaria, Diagnostics and Therapy ; DTG ; Ed .: AWMF as of August 16, 2016, PDF 0.32 MB
German-language books
- Jürgen Knobloch : Malaria - Basics and Clinical Practice . Uni-Med, Bremen 2002, ISBN 3-89599-623-8 .
- Waldemar Malinowski: Vaccinations for foreign travelers and malaria prophylaxis. Vademecum for general practitioners . Facultas, Vienna 2001, ISBN 3-85076-538-5 .
University publications
- Margot Kathrin Dalitz: Autochthonous malaria in central Germany Halle (Saale) 2005, (online dissertation Martin Luther University, Halle-Wittenberg 2005, 87 pages, reviewers: G. Ockert, A. Oehme, St. Schubert (Leipzig) full text online PDF, free of charge, 87 pages, 1.87 MB).
- Desirée Bianca Wollgramm: The spread and control of autochthonous malaria in Germany - 1850 to 1900 , Düsseldorf 2016, DNB 1121174647 (online dissertation University of Düsseldorf 2016, 134 pages, academic advisor: Alfons Labisch, reviewer: Carsten Münk full text online PDF, free of charge, 134 pages, 229 pages).
English language books
- Peter Perlmann, Marita Troye-Blomberg: Malaria Immunology . Karger, Basel 2002, ISBN 3-8055-7376-6 .
- David Sullivan, Sanjeev Krishna (Ed.): Malaria. Drugs, Disease and Post-Genomic Biology . Springer, Berlin 2005, ISBN 3-540-25363-7 .
- David A. Warrell, Herbert M. Gilles: Essential Malariology . Arnold, London 2002, ISBN 0-340-74064-7 .
Journal articles and book articles
- Joel G. Breman, Martin S. Alilio, Anne Mills: The intolerable burden of Malaria II . In: The American journal of tropical medicine and hygiene. Volume 71, Issue 2, Supplement. American Society of Tropical Medicine and Hygiene, Northbrook 2004, ISSN 0002-9637 .
- BM Greenwood, K. Bojang, CJ Whitty, GA Targett: Malaria. In: The Lancet . Volume 365, number 9469, 2005, ISSN 1474-547X , doi: 10.1016 / S0140-6736 (05) 66420-3 , PMID 15850634 , pp. 1487-1498 (review).
- Giacomo Maria Paganotti, Claudia Palladino, Mario Coluzzi: The origin of malaria. In: Spectrum of Science . 2004, No. 3, Heidelberg 2004, ISSN 0170-2971 , pp. 82-89.
- August Stich, Katja Fischer, Michael Lanzer: An Epidemic on the Rise - The Malaria Pathogen's Survival Strategy. In: Biology in Our Time . 2000, Volume 30, Issue 4, ISSN 0045-205X , pp. 194-201.
- WA Maier: Environmental changes and their effects on disease-transmitting arthropods in Central Europe using the example of mosquitoes. In: Denisia. Volume 6 ISSN 1608-8700 ; at the same time: catalogs of the Upper Austrian State Museum. New series, No. 184, 2002, pp. 535–547, full text (PDF).
- Jochen Wiesner, Regina Ortmann, Hassan Jomaa, Martin Schlitzer: New antimalarial ingredients. In: Angewandte Chemie . 2003, Volume 115, Issue 43, ISSN 0044-8249 , pp. 5432-5451.
- 1st floor: Malaria therapy. In: Medical monthly for pharmacists . 2004, Volume 27. Issue 8, ISSN 0342-9601 , pp. 260-272.
- H. Idel: Malaria. Prophylaxis and importance of travel medicine. In: Federal Health Gazette . No. 5, Springer, Berlin 1999, ISSN 1436-9990 , pp. 402-407.
- Helge Kampen: vector-borne infectious diseases on the rise? How environmental changes pave the way for disease carriers and pathogens. In: Naturwissenschaftliche Rundschau . 2005, Volume 58, Issue 4, ISSN 0028-1050 , pp. 181-189.
- Malaria Journal. Open Access journal(English)
- Winfried Schröder, Marcel Holy, Roland Pesch, Gunther Schmidt: Climate change and future possible temperature-controlled malaria transmission in Germany. In: Environmental Sciences and Pollutant Research. Volume 22, Issue 3, 2010, ISSN 0934-3504 , pp. 177-187.
- (Louis) Pasteur Vallery-Radot: La lutte contre le paludisme. In: Revue des deux Mondes. Volume 17, No. 8, 1933, pp. 899-921.
- Patrice Bouree: La lutte contre le paludisme en France au cours de siècles. In: Histoire des sciences médicales. 1982, Volume 17, Numéro spécial 1, pp. 136-141 ( ISSN 0440-8888 ).
- Manfred Vasold: intermittent fever. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1468.
- Ulrike Roll: Malaria. In: Werner E. Gerabek u. a. (Ed.): Encyclopedia of medical history. Berlin / New York 2005, p. 886 f.
- Martin Kappas: Climatology: Climate Research in the 21st Century - Challenge for Natural and Social Sciences. Spektrum, Heidelberg 2009, ISBN 978-3-8274-1827-2 ; 7.2.1. Effects of temperature changes on malaria transmission ; 7.2.2. Effects of changes in precipitation on malaria transmission Limited preview in Google Book search.
- Fritz H. Kayser et al. a .: Pocket textbook medical microbiology. 11th edition. Thieme, Stuttgart 2005, ISBN 3-13-444811-4 .
- Charles C. Mann: Columbus' legacy. How people, animals, plants crossed the oceans and created the world of today. 2nd Edition. Rowohlt, Hamburg 2013, ISBN 978-3-498-04524-1 . (Effects of European Malaria Introduction on Early American Colonies)
- Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , pp. 214-217 ( Malaria ).
- Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid 1961, pp. 9–223, here: pp. 160–172 ( Malaria )
Web links
- Malaria - information from the Robert Koch Institute
- Recommendations for malaria prophylaxis from the German Society for Tropical Medicine and International Health e. V. (DTG)
- World map for malaria prophylaxis recommendations for the year 2017 ( Memento from April 20, 2018 in the Internet Archive ; PDF)
- WHO World Malaria Report 2017
- Guidelines for the treatment of malaria (WHO recommendations for the treatment of malaria), WHO (PDF 2.6 MB), 3rd edition April 2015 (English)
- The genetic sequence of Plasmodium falciparum has been deciphered. (Nature)
- Malaria - a known disease? ( OEW )
- Matthias Giger: "Looking back at the history of malaria and historical methods of treatment." . 1999.
- History of malaria in the North Sea Marsh (English)
- D. Sägesser, B. Thoet: Learning program for medical students. Dissertation University of Bern, Department for Teaching Media (AUM). Bern 1999, 2005.
- Interactive query of case numbers and incidences of notifiable infectious diseases in Germany.
- MARA / ARMA Project Malaria Risk Maps for Africa
- Malaria Atlas Project funded by the Wellcome Trust
- Parasite without mercy. Documentation by Heiner Schirmer on dctp.tv.
- TED talk about "Cheese, dogs and a pill to kill mosquitoes and end malaria" at TEDx Maastricht, · Apr 2012
- thinglink.com multimedia collage - 10 years of struggle
- World Malaria Day 2019 Novartis
Individual evidence
- ↑ a b c d Bernhard Nocht, Martin Mayer: The malaria . An introduction to their clinic, parasitology and control. Second expanded edition. Springer-Verlag, Berlin / Heidelberg 1936, ISBN 978-3-642-89400-8 , p. 2 ( limited preview in Google Book Search - Softcover Reprint of the Hardcover 2nd Edition 1936).
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437–519, here: pp. 470–472.
- ↑ Christopher JL Murray, Lisa C. Rosenfeld, Stephen S. Lim, Kathryn G. Andrews, Kyle J. Foreman: Global malaria mortality between 1980 and 2010: a systematic analysis . In: The Lancet . tape 379 , no. 9814 , February 4, 2012, p. 413-431 , doi : 10.1016 / s0140-6736 (12) 60034-8 , PMID 22305225 ( thelancet.com [accessed June 27, 2017]).
- ↑ A. Pain, U. Böhme and a .: The genome of the simian and human malaria parasite Plasmodium knowlesi. In: Nature. Volume 455, Number 7214, October 2008, pp. 799-803, ISSN 1476-4687 . doi: 10.1038 / nature07306 . PMID 18843368 . PMC 2656934 (free full text).
- ↑ German Society for Tropical Medicine and International Health e. V .: Guideline: Diagnosis and Therapy of Malaria. (PDF) July 2016.
- ↑ Georg Sticker: Hippokrates: The common diseases first and third book (around the year 434-430 BC). Translated from the Greek, introduced and explained by Georg Sticker. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 109.
- ↑ D. Crotti: La Malaria, ossia la mal'aria: brevi note di una “storia sociale e popular” In: Le Infezioni in Medicina , No. 4, 2005, pp. 265-270. ( Memento from February 25, 2016 in the Internet Archive )
- ^ Max Höfler: German book of names of diseases. Munich 1899, p. 390.
- ^ Wolf-Dieter Müller-Jahncke : cinchona bark. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 243.
- ↑ Planet Knowledge: History of Malaria .
- ^ A b Paul Reiter: Climate Change and Mosquito-Borne Disease.
- ↑ Karin Rives: Study: Climate Change Contributes to Malaria Spread. But changing farming practices, migration also cause outbreaks in new areas. ( Memento of May 9, 2010 in the Internet Archive ) April 14, 2010.
- ↑ Elke Hertig: Distribution of Anopheles vectors and potential malaria transmission stability in Europe and the Mediterranean area under future climate change. Parasites & Vectors 2019 12:18 https://doi.org/10.1186/s13071-018-3278-6
- ↑ Malaria: Two New Resistance Genes. In: Deutsches Ärzteblatt . August 16, 2012, accessed February 3, 2014 .
- ↑ Key points: World malaria report 2017. Retrieved January 25, 2018 (British English).
- ↑ Robert Koch Institute: Malaria: RKI Advice on Infectious Diseases - Leaflets for Doctors .
- ↑ Key points: World malaria report 2017. Retrieved January 25, 2018 (British English).
- ↑ (for case numbers from 2001): Robert Koch Institute: SurvStat ( Memento from April 27, 2015 in the Internet Archive )
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437-519, here: p. 470.
- ↑ SE Lindner, JL Miller, SH cap: Malaria parasite pre-erythrocytic infection: preparation meets opportunity. In: Cellular microbiology. Volume 14, Number 3, March 2012, pp. 316-324, ISSN 1462-5822 . doi: 10.1111 / j.1462-5822.2011.01734.x . PMID 22151703 . PMC 3907120 (free full text). (Review).
- ↑ Woman died of malaria after surgery orf.at, March 20, 2019, accessed on March 20, 2019.
- ↑ The criteria for complicated malaria include acidosis with a pH value below 7.25 and hypoglycaemia with a blood sugar level below 40 mg / dl. See Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ^ Fairhurst RM, Wellems TE: Chapter 275. Plasmodium species (malaria) . In: Mandell GL, Bennett JE, Dolin R (Eds.): Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases , 7th. Edition, Volume 2, Churchill Livingstone / Elsevier, Philadelphia 2010, ISBN 978-0-443-06839-3 , pp. 3437-62.
- ↑ B. Nadjm, RH Behrens: Malaria: an update for physicians. In: Infectious disease clinics of North America. Volume 26, Number 2, June 2012, pp. 243-259, doi: 10.1016 / j.idc.2012.03.010 , PMID 22632637 .
- ↑ a b c d e Bartoloni A, Zammarchi L: Clinical aspects of uncomplicated and severe malaria . In: Mediterranean Journal of Hematology and Infectious Diseases . 4, No. 1, 2012. doi : 10.4084 / MJHID.2012.026 . PMID 22708041 . PMC 3375727 (free full text).
- ↑ Beare NA, Taylor TE, Harding SP, Lewallen S, Molyneux ME: Malarial retinopathy: A newly established diagnostic sign in severe malaria . In: American Journal of Tropical Medicine and Hygiene . 75, No. 5, 2006, pp. 790-97. doi : 10.4269 / ajtmh.2006.75.790 . PMID 17123967 . PMC 2367432 (free full text).
- ↑ Ferri FF: Chapter 332. Protozoal infections . In: Ferri's Color Atlas and Text of Clinical Medicine . Elsevier Health Sciences, 2009, ISBN 978-1-4160-4919-7 , p. 1159. Archived from the original on June 3, 2016.
- ↑ Taylor WR, Hanson J, Turner GD, White NJ, Dondorp AM: Respiratory manifestations of malaria . In: Chest . 142, No. 2, 2012, pp. 492-505. doi : 10.1378 / chest.11-2655 . PMID 22871759 .
- ↑ Korenromp E, Williams B, de Vlas S, Gouws E, Gilks C, Ghys P, Nahlen B: Malaria attributable to the HIV-1 epidemic, sub-Saharan Africa . In: Emerging Infectious Diseases . 11, No. 9, 2005, pp. 1410-19. doi : 10.3201 / eid1109.050337 . PMID 16229771 . PMC 3310631 (free full text).
- ↑ Beare NA, Lewallen S, Taylor TE, Molyneux ME: Redefining cerebral malaria by including malaria retinopathy . In: Future Microbiology . 6, No. 3, 2011, pp. 349-55. doi : 10.2217 / fmb.11.3 . PMID 21449844 . PMC 3139111 (free full text).
- ^ Davidson's Principles and Practice of Medicine / 21st / 351
- ↑ Hartman TK, Rogerson SJ, Fischer PR: The impact of maternal malaria on newborns . In: Annals of Tropical Paediatrics . 30, No. 4, 2010, pp. 271-82. doi : 10.1179 / 146532810X12858955921032 . PMID 21118620 .
- Jump up ↑ Rijken MJ, McGready R, Boel ME, Poespoprodjo R, Singh N, Syafruddin D, Rogerson S, Nosten F: Malaria in pregnancy in the Asia-Pacific region . In: Lancet Infectious Diseases . 12, No. 1, 2012, pp. 75-88. doi : 10.1016 / S1473-3099 (11) 70315-2 . PMID 22192132 .
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 165.
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437–519, here: pp. 470–472: Malaria (intermittent fever) .
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ See also Karl Wurm, AM Walter: Infectious diseases. 1961, pp. 165-167.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 172.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 172.
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ "Guideline Development" Committee of the DTG: Guideline: Diagnostics and Therapy of Malaria. (PDF) German Society for Tropical Medicine and International Health (DTG), October 2015, accessed on June 6, 2019 .
- ↑ Georg Sticker : Hippokrates: The common diseases first and third book (around the year 434-430 BC). Translated from the Greek, introduced and explained by Georg Sticker. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 109 f.
- ↑ Jürgen Martin: The 'Ulmer Wundarznei'. Introduction - Text - Glossary on a monument to German specialist prose from the 15th century. Königshausen & Neumann, Würzburg 1991 (= Würzburg medical-historical research. Volume 52), ISBN 3-88479-801-4 (also medical dissertation Würzburg 1990), p. 178 ( Tertiana febris ).
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437-519, here: p. 470.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, pp. 163-165.
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437-519, here: p. 470.
- ↑ Georg Sticker: Hippokrates: The common diseases first and third book (around the year 434-430 BC). 1923, p. 109 f. and 112 f.
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ See also Karl Wurm, AM Walter: Infectious diseases. 1961, p. 165 f.
- ^ Institute for Infectious Diseases / Medical Faculty of the University of Bern: Malaria. A learning program for medical students; Section: Transfusion Malaria. On: e-learning.studmed.unibe.ch Revision in summer 2005; last accessed on February 10, 2016.
- ↑ Malaria rapid tests ( Memento from February 28, 2013 in the Internet Archive ) (PDF) University of Freiburg
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 215.
- ↑ Recommendations for the prophylaxis and therapy of malaria of the DTG 2013. German Society for Tropical Medicine and International Health e. V., 2013, accessed February 3, 2014 .
- ↑ Jörg Braun: Infectious Diseases. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 437-519, here: p. 470.
- ↑ Malaria vaccine launched in Kenya: Kenya joins Ghana and Malawi to roll out landmark vaccine in pilot introduction , World Health Organization. September 13, 2019. Retrieved October 22, 2019.
- ^ Rémy Vatan, Thierry Pistone, Pascal Millet, Gabriel Etienne, Patrick Mercié, Maïté Longy-Boursier, Denis Malvy: Analyze rétrospective de 107 cas de paludisme d'importation chez l'adulte . In: La Presse Médicale . tape 35 , 4-C1. Elsevier Masson, April 2006, ISSN 0755-4982 , p. 571-577 , PMID 16614596 .
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ Recommendations for the prevention of malaria. (PDF) German Society for Tropical Medicine and International Health e. V., May 2018, accessed November 17, 2018 .
- ↑ See Roche Germany: Rote-Hand-Brief zu Lariam. ( Memento of October 22, 2013 in the Internet Archive ) Published on the website of the Federal Institute for Drugs and Medical Devices (BfArM), September 2013.
- ^ W. Burns: East meets West: How China almost cured malaria. In: Endeavor. 32, 2008, pp. 101-106, doi: 10.1016 / j.endeavor.2008.07.001 .
- ↑ protein folding and malaria meds take Lasker . Nature News Blog
- ^ Lasker Clinical Medical Research Award - Tu Youyou . Lasker Foundation
- ^ The Nobel Prize in Physiology or Medicine 2015 . nobelprize.org
- ^ WHO Model List. (PDF; 422 kB) 14th Edition. Essential Medicines, 2005.
- ↑ Guideline Diagnostics and Therapy of Malaria. ( Memento from January 13, 2014 in the Internet Archive ) (PDF) German Society for Tropical Medicine and International Health e. V., November 2013. AWMF guidelines register 042/001.
- ^ PM Arguin, R. Kathrine, KR Tan: Malaria. In: CDC Yellow Book. Centers for Disease Control, Atlanta 2014.
- ^ World Health Organization: Guidelines for the treatment of malaria. 3rd ed. Geneva 2015, ISBN 978-92-4154912-7 ( who.int [PDF]).
- ↑ Marcus VG Lacerda, Alejandro Llanos-Cuentas, Srivicha Krudsood, Chanthap Lon, David L. Saunders: Single-Dose Tafenoquine to Prevent Relapse of Plasmodium vivax Malaria . In: New England Journal of Medicine . tape 380 , no. 3 , January 17, 2019, ISSN 0028-4793 , p. 215-228 , doi : 10.1056 / NEJMoa1710775 ( nejm.org [accessed February 28, 2019]).
- ↑ Justin A Green, Khadeeja Mohamed, Navin Goyal, Samia Bouhired, Azra Hussaini: Pharmacokinetic Interactions between Tafenoquine and Dihydroartemisinin-Piperaquine or Artemether-Lumefantrine in Healthy Adult Subjects . In: Antimicrobial Agents and Chemotherapy . tape 60 , no. 12 , 2016, ISSN 1098-6596 , p. 7321-7332 , doi : 10.1128 / AAC.01588-16 , PMID 27697758 , PMC 5119013 (free full text).
- ^ Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ German Society for Tropical Medicine and International Health e. V .: Guideline: Diagnosis and Therapy of Malaria. (PDF) July 2016. For pregnant women, appropriate contraindications must be taken into account and alternative preparations must be used.
- ↑ Criteria for complicated malaria: impaired consciousness, coma, convulsions, anemia, kidney failure, low blood pressure, jaundice , pulmonary edema or lung failure (ARDS) , acidosis, hypoglycaemia, macroscopically visible hemoglobinuria, hyperparasitaemia. See: Marianne Abele-Horn: Antimicrobial Therapy. ... Marburg 2009, p. 214.
- ↑ E. Tognotti: Program to eradicate malaria in Sardinia, 1946-1950. In: Emerging infectious diseases. Volume 15, Number 9, September 2009, pp. 1460-1466, ISSN 1080-6059 . doi: 10.3201 / eid1509.081317 . PMID 19788815 . PMC 2819864 (free full text).
- ↑ B. Eskenazi, J. Chevrier et al. a .: The Pine River statement: human health consequences of DDT use. In: Environmental health perspectives. Volume 117, Number 9, September 2009, pp. 1359-1367, ISSN 1552-9924 . doi: 10.1289 / ehp.11748 . PMID 19750098 . PMC 2737010 (free full text). (Review).
- ^ US Department of Health and Human Services, Agency for Toxic Substances and Disease Registry: Toxicological profile for DDT, DDE and DDD. (PDF; 4.2 MB) , 2002.
- ↑ IARC Monographs evaluate DDT, lindane, and 2,4-D (PDF) June 23, 2015.
- ↑ India-United Nations pact to end DDT use by 2020 , Deccan Herald , August 26, 2015 Accessed January 30, 2018
- ↑ Malaria: RKI-Ratgeber . Robert Koch Institute
- ↑ New hope for malaria vaccine. In: Spectrum of Science . No. 5, 2005, pp. 20ff.
- ^ VA Stewart, SM McGrath et al. a .: Priming with an adenovirus 35-circumsporozoite protein (CS) vaccine followed by RTS, S / AS01B boosting significantly improves immunogenicity to Plasmodium falciparum CS compared to that with either malaria vaccine alone. In: Infection and Immunity. Volume 75, Number 5, May 2007, pp. 2283-2290, ISSN 0019-9567 . doi: 10.1128 / IAI.01879-06 . PMID 17307942 . PMC 1865796 (free full text).
- ^ K. Matuschewski, AK Mueller: Vaccines against malaria - an update. In: The FEBS journal. Volume 274, Number 18, September 2007, pp. 4680-4687, ISSN 1742-464X . doi: 10.1111 / j.1742-4658.2007.05998.x . PMID 17824954 . (Review).
- ↑ Finally a malaria vaccine? In: Spectrum of Science . No. 1, 2006, p. 10.
- ↑ FAZ: Hope in the fight against malaria. In: FAZ.net . January 16, 2010, accessed December 27, 2014 .
- ↑ ST Agnandji, B. Lell u. a .: First results of phase 3 trial of RTS, S / AS01 malaria vaccine in African children. In: The New England Journal of Medicine . Volume 365, Number 20, November 2011, pp. 1863-1875, ISSN 1533-4406 . doi: 10.1056 / NEJMoa1102287 . PMID 22007715 .
- ↑ Positive study results on possible malaria vaccine for children. (No longer available online.) GlaxoSmithKline, October 8, 2013, archived from the original on April 9, 2014 ; Retrieved July 24, 2014 (press release).
- ↑ GSK announces EU regulatory submission for malaria vaccine candidate RTS, p. (No longer available online.) GlaxoSmithKline, July 24, 2014, archived from the original on February 20, 2015 ; accessed on February 20, 2015 (English, press release).
- ↑ Efficacy and safety of RTS, S / AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomized, controlled trial . In: RTS, S Clinical Trials Partnership (Ed.): Lancet . April 23, 2015 (English, thelancet.com ).
- ↑ Vasee S Moorthyemail, Jean-Marie Okwo-Bele: Final results from a pivotal phase 3 trial malaria vaccine . In: Lancet . April 23, 2015, doi : 10.1016 / S0140-6736 (15) 60767-X (English). , quoted from Alina Schadwinkel: The first vaccine against malaria is coming . Zeit Online , April 24, 2015; Retrieved April 25, 2015
- ↑ Experiment with mice: vaccination makes malaria pathogens more aggressive. In: Spiegel Online . August 1, 2012, accessed December 27, 2014 .
- ↑ Finally a vaccine? Anti-malaria serum lowers the disease rate. n-tv, August 8, 2013, accessed December 7, 2013 .
- ↑ Protection Against Malaria by Intravenous Immunization with a Nonreplicating Sporozoite Vaccine. In: Science. Retrieved December 7, 2013 .
- ↑ Wissenschaft.de: Inoculated reproductive stop ( memento of March 30, 2008 in the Internet Archive ) of March 26, 2008.
- ↑ Y. Liu, R. Tewari et al. a .: The conserved plant sterility gene HAP2 functions after attachment of fusogenic membranes in Chlamydomonas and Plasmodium gametes. In: Genes & development. Volume 22, Number 8, April 2008, pp. 1051-1068, ISSN 0890-9369 . doi: 10.1101 / gad.1656508 . PMID 18367645 . PMC 2335326 (free full text).
- ↑ A New Perspective for the Fight Against Malaria. Heidelberg University Hospital, October 30, 2002.
- ↑ RH Schirmer, B. Coulibaly et al. a .: Methylene blue as an antimalarial agent. In: Redox report: communications in free radical research. Volume 8, Number 5, 2003, pp. 272-275, ISSN 1351-0002 . doi: 10.1179 / 135100003225002899 . PMID 14962363 . (Review).
- ^ Malaria Atlas Project
- ^ S. Wang, AK Ghosh et al. a .: Fighting malaria with engineered symbiotic bacteria from vector mosquitoes. In: Proceedings of the National Academy of Sciences . Volume 109, Number 31, July 2012, pp. 12734-12739. doi: 10.1073 / pnas.1204158109 . PMID 22802646 .
- ↑ Hope for a vaccine: Newly discovered antibody protects against malaria. In: Spiegel Online - Wissenschaft. May 23, 2014, accessed June 24, 2014 .
- ↑ DK Raj, CP Nixon et al. a .: Antibodies to PfSEA-1 block parasite egress from RBCs and protect against malaria infection. In: Science. Volume 344, Number 6186, May 2014, pp. 871-877, ISSN 1095-9203 . doi: 10.1126 / science.1254417 . PMID 24855263 . PMC 4184151 (free full text).
- ↑ Malaria: vaccine developed from Tetrahymena. In: aerztezeitung.de . March 10, 2014, accessed June 10, 2014 .
- ^ Vaccine Development: New Weapon Against Malaria. In: Focus.de . March 1, 2014, accessed June 10, 2014 .
- ↑ NJ White, S. Pukrittayakamee et al. a .: Spiroindolone KAE609 for falciparum and vivax malaria. In: The New England Journal of Medicine . Volume 371, Number 5, July 2014, pp. 403-410, ISSN 1533-4406 . doi: 10.1056 / NEJMoa1315860 . PMID 25075833 . PMC 4143746 (free full text).
- ↑ Alexander L. Perryman: GO Fight Against Malaria update: promising early findings for malaria & drug-resistant tuberculosis. July 14, 2014, accessed February 20, 2015 .
- ↑ Alexander L. Perryman et al. a .: A Virtual Screen Discovers Novel, Fragment-Sized Inhibitors of Mycobacterium tuberculosis InhA . In: J. Chem. Inf. Model. January 30, 2015, doi : 10.1021 / ci500672v .
-
↑ Ailie Robinson et al .: Plasmodium-associated changes in human odor attract mosquitoes. In: PNAS . Online pre-publication of April 16, 2018, doi: 10.1073 / pnas.1721610115
Malaria infection creates a 'human perfume' that makes us more attractive to mosquitoes. On: sciencemag.org of April 26, 2018, doi: 10.1126 / science.aat8993 - ↑ Consuelo M. De Moraes et al .: Malaria-induced changes in host odors enhance mosquito attraction. In: PNAS. Volume 111, No. 30, 2015, pp. 11079–11084, doi: 10.1073 / pnas.1405617111
- ↑ Renaud Lacroix et al .: Malaria Infection Increases Attractiveness of Humans to Mosquitoes. In: PLoS Biology. Online publication from August 9, 2005, doi: 10.1371 / journal.pbio.0030298
- ↑ Norbert Blüm: I imagine the CDU to be different. In: Süddeutsche Zeitung . October 7, 2003, accessed February 3, 2014 .
- ↑ Combating poverty-related diseases: Commissioner Philippe Busquin visits Africa and presents the clinical trials program. EU Commission, July 31, 2003, accessed on February 3, 2014 (press release).
- ↑ Paul PROCIV: Malaria Vaccine: Salvation for the World? (PDF) (No longer available online.) In: The Skeptic . 2005, p. 58 , archived from the original on February 14, 2014 ; Retrieved February 3, 2014 .
- ↑ Bill Gates wants to fight malaria with $ 258 million. (No longer available online.) October 31, 2005, archived from the original on January 12, 2006 ; Retrieved February 3, 2014 .
- ↑ J. Sachs, P. Malaney: The economic and social burden of malaria. In: Nature. Volume 415, Number 6872, February 2002, pp. 680-685, ISSN 0028-0836 . doi: 10.1038 / 415680a . PMID 11832956 . (Review).
- ↑ BM Greenwood, K. Bojang et al. a .: Malaria. In: Lancet. Volume 365, Number 9469, 2005 Apr 23-29, pp. 1487-1498, ISSN 1474-547X . doi: 10.1016 / S0140-6736 (05) 66420-3 . PMID 15850634 . (Review).
- ↑ Malaria among the ancient Egyptians. In: Epoc . The magazine for archeology and history. Volume 1, number 10, spectrum, Heidelberg 2009, ISSN 1865-5718 , based on: Discovery chanal 8.2008 .
- ↑ Cf. Georg Sticker : Hippokrates: Der Volkskrankheiten first and third book (around the year 434-430 BC). Translated from the Greek, introduced and explained by Georg Sticker. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 108 f.
- ^ Gundolf Keil : Fever theory. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil, Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte . De Gruyter, Berlin 2005, ISBN 3-11-015714-4 , pp. 398-400, here: p. 398 ( Hippocratic ).
- ↑ Gundolf Keil (2005), p. 399 f. ( Galen ).
- ↑ Georg Sticker : Hippokrates: The common diseases first and third book (around the year 434-430 BC). Translated, introduced and explained from the Greek. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 115.
- ^ Johann Hermann Baas: The historical development of the medical status and the medical sciences. Leipzig 1896, p. 99.
- ↑ Renate Wittern : The intermittent fever at Galen . In: Hist. Phil. Life Sci. tape 11 , no. 1 , 1989, pp. 3-22 , JSTOR : 23330279 .
- ↑ Georg Sticker: Hippokrates: Der Volkskrankheiten first and third book (around the year 434–430 BC) 1923, pp. 118–121 (on five days, seven-day fever, nine-day fever, etc.)
- ↑ Barbara I. Tshisuaka: Ingrassias, Giovanni Filippo. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 673.
- ↑ Manfred Vasold: The mortality in Nuremberg in the 19th century. Living conditions, illness and death (around 1800 to 1913). In: Würzburg medical history reports. Volume 25, 2006, pp. 241-338, here: pp. 279 f.
- ↑ David George Haskell: The forest unseen: a year's watch in nature. Viking, New York 2012, ISBN 978-0-670-02337-0 , p. 111.
- ↑ Georg Sticker : Hippokrates: The common diseases first and third book (around the year 434-430 BC). Translated from the Greek, introduced and explained by Georg Sticker. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, pp. 110–112.
- ↑ See also Paul de Kruif : Ross versus Grassi . The fight against malaria. In: Paul de Kruif: Microbe hunters. (Original edition: Microbe Hunters. Harcourt, Brace & Co., New York 1926) Orell Füssli Verlag, Zurich / Leipzig 1927; 8th edition ibid. 1940, pp. 268-300.
- ↑ Markus Brauer: Nobel Prize in Medicine 2015 for three parasite researchers. Fight against the scourges of humanity . On: stuttgarter-nachrichten.de , October 5, 2015; accessed on October 7, 2015.