Robert Koch
Heinrich Hermann Robert Koch (born December 11, 1843 in Clausthal , † May 27, 1910 in Baden-Baden ) was a German physician , microbiologist and hygienist . In 1876, Koch succeeded in cultivating the anthrax pathogen ( Bacillus anthracis ) outside the organism and describing its life cycle . This was the first time that the role of a pathogen in the development of a disease was fully described. In 1882 he discovered the causative agent of tuberculosis ( Mycobacterium tuberculosis) and later developed the supposed remedy tuberculin . In 1905 he received the Nobel Prize in Physiology or Medicine . Robert Koch has become the founder of modern bacteriology and microbiology - alongside his colleague Louis Pasteur in Paris . He has made fundamental contributions to infection theory and the development of tropical medicine in Germany.
Life
childhood and education

Robert Koch was born in Clausthal in 1843 as the third of a total of 13 children of Steigers and later secret mountain councilor Hermann Koch (1814–1877) and his wife Mathilde (née Biewend, 1818–1871). Of the children, nine boys and two girls survived infancy. Robert's father was promoted quickly and from 1853 supervised the entire mining of the Upper Harz . Robert Koch taught himself to read and write at the age of four. He copied it from his older brothers. From 1848 he was taught by a private teacher. At the age of seven he switched to the humanistic grammar school in Clausthaler Graupenstrasse , which he attended until his Abitur in 1862.
Grandfather Heinrich Andreas Biewend, the father of Koch's mother, and his son Eduard introduced Robert Koch to the microscope and introduced him to photography, which was still new at the time .
From 1862 Robert Koch studied philology in Göttingen , but decided to study medicine in the first semester . Among other things, he heard physics from Wilhelm Weber and chemistry from Friedrich Wöhler . In medicine, the anatomist Jakob Henle , the physiologist Georg Meissner and the clinician Karl Ewald Hasse became his formative teachers.
In 1866 he completed his studies with a doctorate. Before taking the state examination, he studied with Rudolf Virchow in Berlin for a short time . To the general surprise of friends and acquaintances, he announced in May 1866 that he had become engaged to Emmy Fraatz. The two married the following year.
Career
This was followed by medical activities at the General Hospital in Hamburg, then until 1868 at the "Education and Care Institute for mentally weak children" (today KRH Psychiatrie Langenhagen) in Langenhagen near Hanover, where he also ran a private practice. He then moved to Niemegk ( Mark Brandenburg , near Potsdam ) as a country doctor and to Rakwitz near Posen .
In the Franco-Prussian War of 1870/71, Koch volunteered for the medical service and mainly looked after people suffering from typhus and dysentery . Returning from this, he passed the physics examination in 1872 - a prerequisite for working as a medical officer - and in the same year was appointed district physician of the Bomst district with a practice in Wollstein ( Poznan province ). In this function he had to prepare expert reports, deal with court cases, was responsible for the municipal hospital and worked as a doctor for the poor. He also ran a private practice. He spent the little free time doing bacteriological research. For experimental purposes he kept numerous domestic animals, such as rabbits, guinea pigs and, lastly, two monkeys.
Thanks to his work on the development of anthrax and wound infections, Koch was appointed to the Imperial Health Department in Berlin in 1880 . In 1885 he left the health department and became a full professor of hygiene at the newly created Hygienic Institute of the Berlin University . In 1891 he was appointed director of the Institute for Infectious Diseases in Berlin, and in 1904 he retired.
Two marriages
Robert Koch married Emmy Adolfine born in 1867. Fraatz (1847–1913), the daughter of Wilhelm Christian Friedrich Fraatz . From this marriage came a daughter, Gertrud (1868–1945), called “Trudy”, with whom Koch maintained a good relationship throughout his life. In 1888 she married Eduard Pfuhl , who worked for Koch. Koch divorced his wife in 1893. At that time, this was still an unusual step - the possibility of divorce had only existed in the German Reich for 15 years - which could easily lead to social isolation. Emmy Koch agreed to the divorce and Koch bought back his parents' house in Clausthal for her, where she lived until her death in 1913.
In 1890 Koch met Hedwig Freiberg (1872–1945), then seventeen. The meeting place was the studio of the painter Gustav Graef , when Koch was sitting as a model for a portrait. Freiberg was a student of the painter. She married Koch three years later. Unlike Emmy Koch, his second wife liked to accompany him on his numerous trips abroad.
Trips abroad
Even as a young boy, Koch dreamed of becoming a traveling naturalist. Seven brothers and one sister immigrated to Uruguay, Mexico, and the United States. Probably Koch himself stayed in Germany only through the influence of his first wife Emmy. When he was able to combine bacteriological research with trips abroad, he immediately took the opportunity. In 1883/1884 he led a cholera expedition to Egypt and India.
Due to the tuberculin scandal of 1890, Koch's reputation sank to a low point and he fled to Egypt. After that he stayed in Germany only a little: in 1896 the British government invited him to research rinderpest in South Africa ; as a member of the German plague commission, he traveled to India in 1897, then to German East Africa. In 1898/1899 he researched malaria in Italy, Java and New Guinea. In 1901 he was elected to the American Academy of Arts and Sciences , in 1903 to the National Academy of Sciences .
“At home we have worked so thoroughly and the competition is so huge that it is really no longer worth researching there. But out here, there is still the gold of science on the street. How many new things I saw and learned when I came to Africa for the first time! "
- Robert Koch, 1903, font from Bulawayo
In 1905/1906 he led an expedition to German East Africa to investigate sleeping sickness , but then did research mainly on British colonial territory in Uganda. He interrupted this trip to receive the Nobel Prize for Medicine in Stockholm in 1905 for the discovery of the tuberculosis pathogen. In 1908 he made a world trip to the United States , the Republic of Hawaii and the Japanese Empire .
End of life
At the beginning of the 20th century, Koch looked prematurely aged. During his travels he was infected with tropical diseases, including malaria, on several occasions. In April 1910 he became seriously ill. He complained of pain in his left chest and difficulty breathing. On May 23, 1910, he moved into the Dr. Franz Dengler in the Baden-Baden quarter. On the evening of May 27, 1910, Dr. Dengler appears lifelessly at the open balcony door. In Baden-Baden, Koch's body was cremated in the crematorium that had been built shortly before on May 30th, although no special celebration was held at the request of the deceased. His urn was brought to the Institute for Infectious Diseases - today the Robert Koch Institute - in Berlin and buried on December 10, 1910 in a room in the institute designated as a mausoleum . His grave is an honorary grave of the city of Berlin .
Justification of bacteriology
Bacteriology began in 1872, when Ferdinand Julius Cohn published a multi-part article with "Studies on Bacteria". The prevailing opinion at the time was that the different forms of bacteria can merge depending on the environmental conditions, i.e. basically form a single species . On the other hand, Cohn distinguished between different types of bacteria that could only be changed within certain limits. In 1877 he was also able to prove that hay bacilli ( Bacillus subtilis ) formed spores .
The life cycle of the anthrax pathogen

Koch is not the discoverer of the anthrax pathogen , but Aloys Pollender (1849). In 1863 Casimir Davaine made a connection between the bacteria and the disease at least likely. With anthrax , Koch investigated a cattle disease that played a major role in rural areas but could also affect people. For his microscopic studies, he developed the technique of the hanging drop, in which the microbes are cultivated in a drop on the underside of a slide. He used aqueous humor from bovine eyes as a nutrient fluid . With this arrangement, he was able to detect bacteria in the blood of infected animals and observe how they formed spores and how these spores were converted back into bacteria. He later colored the actually transparent spores, a technique suggested by Carl Weigert . If he artificially infected laboratory animals - such as guinea pigs or rabbits - they died of anthrax. He also managed to document the pathological process in which the bacteria damage blood vessels.
With his work, Koch was able to explain why cattle were repeatedly infected with anthrax in certain pastures. The farmers had not buried the carcasses of dead animals deep enough in the ground. Koch was also able to extract anthrax spores from such carcasses. He was also able to prove that dried blood from sick sheep was still infectious after four years. He sent the first draft of his anthrax article to Cohn, who responded enthusiastically. Cohn invited Koch to a multi-day presentation in Breslau; On this occasion Paul Ehrlich also met Koch for the first time. The publication appeared in print in 1876.
An animal model for wound infections
The next problem Koch turned to wound infections. Researchers had already found many different bacteria here without being able to say which species was responsible for the disease. Koch established an animal model for sepsis . He understood the animal body as a cultural apparatus, an original idea at the time. He had also noticed that different animal species were differently susceptible to different types of bacteria. If he inoculated a sample one after the other with different animal species such as mice, rabbits and guinea pigs, he finally received pure cultures of one type of bacteria. He was then able to demonstrate six different forms of sepsis in mice, which were triggered by six different types of bacteria. Koch published his "Studies on the Aetiology of Wound Infection Diseases" in 1878.
Appointment to the Imperial Health Department
The University of Breslau asked the Prussian minister of education to appoint Koch as an extraordinary professor for hygiene. Instead, however, Koch was appointed to the position of city physician in Breslau in 1879 . Koch quickly realized that he was not earning enough in the office and asked for a transfer back.
In 1880 Heinrich Struck, director of the Imperial Health Office , hired him to expand the four-year-old office in Berlin into a medical research facility. Koch was joined by the two military doctors Friedrich Loeffler and Georg Gaffky , and a little later the doctor Ferdinand Hueppe and the chemist Bernhard Proskauer .
Development of bacteriological techniques
Robert Koch always strived to stay at the forefront of technological development, and so many of his discoveries were driven by technological progress. He used the first oil immersion lenses before they were available on the market. Most microorganisms are transparent; they only become visible in the microscopic image after they have been colored. He used photography to record his observations.
At the Imperial Health Department he developed the culture plate technique with solid, transparent nutrient media. Until then, bacteria had either been grown in meat broth - which could not be fixed under the microscope - or on potato slices - which could not be viewed in transmitted light under the microscope and on which many pathogenic bacteria did not grow. Cook the broth solidified with gelatin , later, his staff led Walther Hesse for agar-agar according to the invention his wife Fanny Hesse one. The nutrient media were poured into rectangular "plate dishes". The innovation of solid, transparent nutrient media revolutionized bacteriology.
In order to research the tuberculosis pathogen, Koch had an incubator built for the first time in April 1881 by the art locksmith Hermann Scharlach in Berlin according to his own plans for the cultivation of bacterial cultures in a controlled, warm environment. Today the incubator is kept in the Deutsches Museum in Munich.
Discovery of the tuberculosis pathogen

While in the south of Europe it was always known that tuberculosis - the term has been used since 1834 - was a contagious disease, this was increasingly doubted in the northern part of Europe until hardly anyone believed it anymore in the middle of the 19th century. Koch undertook the first experiments in 1881 by transferring tubercular tissue to two guinea pigs. They turned out to be ideal test animals that actually got sick with tuberculosis. In contrast , the tubercle bacteria only grew very slowly on artificial nutrient media , so Koch's greatest achievement is that he did not lose patience prematurely. In addition, the bacteria are surrounded by a waxy layer that repels dyes. As a major innovation, Koch introduced counterstaining, in which he first stained the bacteria blue with methylene blue (this method was introduced to bacteriology by Koch's student Paul Ehrlich ) and, for contrast, colored the surrounding tissue slightly brown with a second dye called Vesuvin . However, the coloration remained so weak that he only managed to draw the bacteria and not, as he asked, to take pictures. In the 271st trial, Koch discovered the pathogen he was looking for.
Koch also described spores in them as he knew them from anthrax and from Cohn's hay bacilli. However, tuberculosis spores do not exist. On March 24, 1882, he presented his discovery to the Berlin Physiological Society in his now famous lecture on the " Aetiology of Tuberculosis" . After the lecture there was silence because everyone present was aware that they had just witnessed a historical event . Paul Ehrlich, now also working in Berlin, improved the dyeing process that same evening. On June 27, 1882, Kaiser Wilhelm I appointed Robert Koch a secret councilor .
A consequence of this discovery was that the character of tuberculosis as a single disease was confirmed. Before that, pulmonary tuberculosis - the most common form of tuberculosis - as well as tuberculosis of the skin, bones, intestines, the urogenital system and tuberculous meningitis were separate diseases with their own names. Most of the cases that were previously referred to as "consumption" or "phthisis" are also likely to have been tuberculosis. It is controversial whether scrofulosis - which is interpreted as a tuberculous disease of the cervical lymph glands - is one of them. The French doctor René Laënnec had already suspected that all these forms were a disease, but only the common pathogen provided the proof. Koch was able to make breathing air probable as a transmission medium; in the sputum of tuberculosis he detected tubercle bacilli. This made it clear that the main danger came from patients with open pulmonary tuberculosis.
Institutional upgrading of bacteriology
In 1885, the medical faculty of the Friedrich-Wilhelms-Universität in Berlin appointed Koch to a full professor in a newly created chair for hygiene. The subject of hygiene was thus greatly upgraded, but Koch was unqualified as a professor. Lectures and exams were a burden to him. He went on several long recreational trips, but his health has been in poor health ever since. The fact that Louis Pasteur's competing research group in Paris achieved spectacular successes during this time - especially in the development of active vaccination - did not improve his mood. Until 1890 there was no news of any importance from the researcher Koch; he also went through a crisis in his private life, which eventually ended with the divorce from his first wife.
Tuberculin scandal

In Koch's time, around one in seven Germans died of tuberculosis. The public reacted euphorically to the discovery of the pathogen because it linked the hope of a cure. Until then, quinine for malaria was the only known effective cure for an infectious disease.
At the “Tenth International Medical Congress” in Berlin in 1890 - the conference took place in the specially converted Circus Renz - Koch suddenly presented a remedy that he called tuberculin . He kept the composition a secret, which is understandable because it was not customary at the time to patent drugs ( antipyrine was the only exception). The public had to trust the big names and responded enthusiastically. Koch was awarded the Grand Cross of the Red Eagle Order.
The social hygienist Alfred Grotjahn described how tuberculin arrived in Greifswald : “The big day finally came for Greifswald too when the first vaccinations with tuberculin were to be carried out in the inner clinic. It was celebrated such as laying the foundation stone or unveiling a monument. Laurel trees formed the background from which doctors, nurses and patients stood out in snowy white and the boss in black dry clothes: the internist's speech, vaccinations on selected patients, thunderous cheers for Robert Koch! "
Koch tried to make commercial profit from his discovery, which he was resented because he had researched with government funds at a government institute. He demanded that the Ministry of Culture set up its own institute exclusively for the production of tuberculin and estimated the annual profit to be 4.5 million marks. He also indicated that he already had offers from the USA.
There were no rules for drug trials at that time. According to Koch, he had tested the drug on animals; however, he was later unable to produce the supposedly cured guinea pigs. He was not worried that people were much more sensitive to tuberculin with fever, joint pain and nausea than his test animals. Among other things, he tested tuberculin on his lover and later second wife, Hedwig Freiberg, who was then seventeen. In her memoirs, she reports that, according to Koch, she could “possibly get very sick”, “I would probably not die”.
After tuberculin was on the market, reports of healing successes began to pile up in the specialist and public press, then the first reports of deaths followed. However, Rudolf Virchow was able to prove in the autopsy of cadavers that tuberculin did not kill the bacteria and even activated latent bacteria. Robert Koch was forced to uncover the composition of his secret drug, which it turned out that he himself did not know exactly what it contained. It was an extract of tubercle bacilli in glycerine, and dead tubercle bacilli could also be detected.
Koch took leave of absence from the Prussian minister of education and went to Egypt, which was interpreted as an escape from the German public. In the Prussian House of Representatives , a heated debate took place in May 1891st Koch remained convinced of the value of his remedy and in 1897 presented a modified tuberculin, which was also worthless as a therapeutic agent. This and numerous other pieces of evidence indicate that Koch did not want to commit a “tuberculin fraud”, as he was often accused at the time, but that he had deceived himself.
The medical historian Christoph Gradmann has reconstructed how tuberculin should work according to Koch. Accordingly, the agent did not kill the bacteria, but triggered necrosis of the tubercular tissue, which resulted in the tubercle bacilli being “starved”, so to speak. Then, as now, this idea lay outside conventional medical theories.
The tuberculin scandal has been widely understood as a warning not to proceed when testing drugs. When Emil von Behring presented his diphtheria antitoxin in 1893 , it had been preceded by lengthy clinical tests and the serum was only slowly introduced into practice - accompanied by a critical discussion in the professional community. Even Paul Ehrlich was in 1909 with the introduction of the first synthetic chemotherapeutic agent against an infectious disease Salvarsan , striking caution.
In 1907, Clemens von Pirquet further developed tuberculin into a diagnostic agent for tuberculosis in the tuberculin test , which, however, represents an independent achievement independent of Robert Koch's ideas. The color works in Frankfurt / Höchst, formerly “Meister Lucius & Brüning AG” (later Hoechst AG ), bought up the still abundant tuberculin stocks. Later, the company went into production under the direction of Arnold Libbertz, a student at the cook.
Nobel Prize
The Nobel Prize, first awarded in 1901, at the time it was awarded to Robert Koch in 1905, did not yet have the dominant role it plays today, even if the high amount of the prize money caused a sensation. Koch was annoyed that his student Emil von Behring had received it before him.
Bovine Tuberculosis Controversy
In 1882, when the tuberculosis pathogen was announced, Koch had suggested that cattle addiction to cattle was identical to human tuberculosis. In 1891, at the first British Congress of Tuberculosis, he announced the opposite and met with great opposition. Emil von Behring also insisted that the milk of tuberculous cows was dangerous. In 1902, Koch gave his own lecture on “Transferability of Bovine Tuberculosis to Humans”, in which he also described meat from tuberculous animals as harmless. In 1908, as Honorary President of the International Tuberculosis Conference in Washington, he held fast to his views. Through his authority he hindered efforts in Germany to create tuberculosis-free cattle herds.
In fact, according to today's understanding, the bovine tuberculosis pathogen belongs to a separate species. However, Mycobacterium bovis can infect humans, just as the human tuberculosis pathogen can infect cattle. In France , the microbiologist Saturnin Arloing recognized the zoonotic potential of bovine tuberculosis as early as 1872 and introduced state control measures against the disease.
Prussian Institute for Infectious Diseases in Berlin

In 1891 Koch gave up his professorship and took over the management of the Prussian Institute for Infectious Diseases founded especially for him with an experimental and a clinical department. He finally had beds for his clinical research. For that he had to accept harsh conditions. After the tuberculin scandal, the Prussian Ministry of Culture insisted that all further inventions of Koch should belong to the government unconditionally and without compensation. Koch lost the right to apply for patents.
Henle-Koch postulates
The Henle-Koch postulates specify the criteria under which a microbe may be considered a pathogen. They are wrongly attributed to Koch's Göttingen teacher Jakob Henle or Robert Koch himself. The classic formulation of the three postulates was done in 1884 by the Koch student Friedrich Loeffler . Up to this point in time, they can only be derived implicitly from Koch's works, and they also vary with his scientific development.
Koch only formulated his version of the postulates in a lecture at the “Tenth International Medical Congress” in Berlin in 1890, when the question was whether bacteria were not accidental side effects of a disease. To this he replied: “But if it could now be demonstrated: first, that the parasite is to be found in every single case of the disease in question, under conditions which correspond to the pathological changes and the clinical course of the disease; second, that it does not occur in any other disease as an incidental and non-pathogenic parasite; and thirdly, that it is completely isolated from the body and sufficiently often re-bred in pure cultures, is able to recreate the disease; then it could no longer be an accidental accident of the disease, but in any case no other relationship between parasite and disease could be thought than that the parasite is the cause of the disease. "
cholera
The cholera had broken out in Europe for the first time in 1830/31. After that there were several epidemics, most recently in 1866 and 1873. Due to the traffic revolution, the cholera areas - as Koch pointed out - were only a few days away from Europe.
Expedition to Egypt and India
When news of a cholera epidemic in Egypt reached Europe again in 1883 , various European powers sent scientists, including the Prussian government, an expedition led by Robert Koch. When she arrived in Alexandria in August 1883 , the epidemic was already on the decline. There, Koch discovered that the culture methods he used in Berlin failed under Egyptian conditions: the culture mediums made solid with gelatine liquefied in the heat. The Egyptian part of the expedition was therefore more like a tourist excursion.
The expedition moved to India in November. On the one hand there was around Calcutta the only known area in which cholera was endemic, on the other hand the temperatures there were low enough for a short period in winter to work with the usual culture methods. In January 1884, Koch succeeded in obtaining a pure culture of bacteria from cholera oaks, which were shorter and clumsier than tubercle bacilli and had the shape of a comma. He called these bacteria the causative agents of cholera , although he had not been able to prove it by his own standards: he had tried in vain to infect animals with the disease. In February it became too hot in Calcutta to continue the research. The return to Berlin in May was a triumphal procession. Koch received a reward of 100,000 marks and was received by the emperor.
Since then, Robert Koch has often been referred to as the discoverer of the cholera pathogen. In fact, Filippo Pacini described the bacteria as early as 1854, but was ignored at the time. Probably even Koch himself saw cholera bacteria in 1866, when he was dissecting cholera corpses as a young doctor in Hamburg, but at that time did not attach any importance to his observation. Also in 1854 the Catalan Joaquim Balcells i Pascual described the pathogen and in 1856 probably the two Portuguese António Augusto da Costa Simões and José Ferreira de Macedo Pinto .
Another observation made by Koch in India is more important. The disease appeared to be tied to specific villages that were arranged around small ponds. Koch observed that in these ponds the laundry of cholera sufferers was washed, but at the same time they were bathed in them and drinking water was taken from them. There were latrines at the edge of the ponds . Koch correctly concluded from this that cholera pathogens are transmitted with the water. In the English-speaking world, this transmission route was already known thanks to the work of the London doctor for the poor, John Snow, from 1854 (published in German in 1856), but was not taken seriously in Germany due to the influence of Max von Pettenkofer (see below).
Cholera in Hamburg

The cholera epidemic in Hamburg in 1892 was the last major cholera outbreak in Germany. It was probably brought in with the stream of Russian emigrants who passed through the port city after a famine and anti-Semitic pogroms . The first case was diagnosed on August 15, but it wasn't until eight days later that authorities admitted that an epidemic had broken out in the city. Before the epidemic was officially announced, the Prussian Minister of Health sent Robert Koch to Hamburg. After an inspection of the Gängeviertel, Koch uttered the now famous sentence: “I forget that I am in Europe!” It was only through the epidemic that many members of the bourgeoisie became aware of the filth and misery in which a large part of the population lived.
The Hamburg doctors were not yet familiar with the bacteriological methods used to detect the cholera pathogen. Koch implemented disease control measures that assumed a bacterium as the cause. The population was asked to boil drinking water; Sick people's homes were cleaned by special disinfection columns. The only organization capable of acting during the crisis turned out to be the Social Democrats , who distributed leaflets with advice on behavior to all households.
Robert Koch left Hamburg again on August 25, 1892. Further immediate measures that Koch ordered and which were later implemented by the Senate were locking the port, closing the school, and stopping traffic with Hamburg. The climax of the epidemic in Hamburg was August 30, 1892. The victims were buried in mass graves in the Ohlsdorf cemetery. A memorial stone from 1992 on the Ohlsdorf cemetery by the Patriotic Society from 1765 reminds of this.
When the epidemic ended in October, 16,956 had fallen ill and around 8,600 people had died. One of the factors contributing to cholera was found to be that thousands of toilets were not yet connected to the sewer system; the tide pushed polluted harbor water into the central water extraction point, which was two kilometers upstream. The Senate and the city council could not agree on the construction of a sand filtration plant.
After the epidemic, a new waste incineration plant and filter works were put into operation on the Elbe island Kaltehofe . Under Koch's direction, advanced training courses were arranged for medical officers, and in 1893 the Koch student Bernhard Nocht was appointed to the position of port doctor. Another immediate consequence of the epidemic was the professional civil service in Hamburg.
In 1892 there was great concern in the rest of Germany that the epidemic would spread beyond Hamburg. A "Reich Epidemic Law" was drawn up, which came into force on June 30, 1900. For the diseases listed in the law, a compulsory notification requirement was provided, as well as the determination of epidemic cases through bacteriological examinations, the separation of sick people, monitoring of suspected contagious persons, observation of suspected diseases and various disinfection measures.
Max von Pettenkofer , Professor of Medicinal Chemistry in Munich, was still a prominent proponent of the miasm theory. With regard to cholera, this meant that cities on damp ground were at risk, while cities on hard ground - such as Würzburg - had nothing to fear. Pettenkofer did not allow himself to be changed by the discovery of the pathogen and its path of infection. On the occasion of the epidemic of 1892, he asked Koch for a culture of the pathogens that he swallowed. Pettenkofer got away with diarrhea while one of his assistants nearly died.
Further trips to Africa and India
In 1896 the British government asked Koch to help fight a cattle disease in South Africa. It was rinderpest , which was brought in with imported cattle. Koch was able to prove in Kimberley that the blood of sick animals was highly contagious; since it is a viral disease , he was unable to find the pathogen. Following the example of the Pasteur school, he developed a vaccine from the serum of surviving animals and the bile of dead animals. This vaccine is said to have been effective.
During a stay in Bulawayo in March 1897, Koch received an invitation from the German government to go to India, where the plague had broken out. The journey turned out to be cumbersome because the direct ship connections were interrupted due to the plague. However, the pathogen was already known ( Yersin , 1894). Koch's most important observation in this context was that a plague outbreak could be preceded by large rat deaths. The transmission of the plague from rats to humans by the rat flea was only discovered by Charles Rothschild and Karl Jordan .
Koch returned to Africa in July 1897, where he stopped in Dar es Salaam , German East Africa . He stayed for almost a year, researching the plague - which also occurred here -, malaria and a cattle disease.
Robert Koch as an epidemiologist
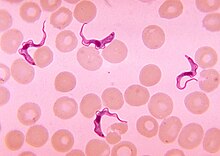
As part of the Hamburg cholera epidemic, Koch first came across the phenomenon that healthy people can harbor infectious agents; in the parlance of the time they were "germ carriers". Above all, however, as a result of a malaria expedition to New Guinea, his attention shifted from pathogens to healthy people as carriers of pathogens - he went from bacteriologist to epidemiologist . He was interested in diseases that, like malaria and sleeping sickness, are not caused by bacteria but by protozoa .
malaria
Robert Koch first dealt with malaria in Dar es Salaam in 1897. The disease - called "intermittent fever" here - still occurred in Germany. The colony with the greatest malaria problem in the German colonial empire, however, was Kaiser-Wilhelms-Land in German New Guinea . In the first years of the protectorate, around 1,500 malaria fever attacks were registered here among 150 Europeans. In Finschhafen even a third of the settlers died of the disease, so that the place had to be abandoned. In 1900, at the request of Paul Kupelwieser , Koch examined malaria on Brioni in the Austrian coastal region (today Brijuni , Croatia), he initiated the rehabilitation of the island and trained doctors. As early as 1901, Brioni was free of malaria and the rise to a popular health resort could begin. In memory of Koch, a monument by Josef Engelhart was erected near the port .
Phenomenon of "acquired immunity"
When the colonial department of the Federal Foreign Office sent Robert Koch to New Guinea in 1898, he was first brought up to date by his colleague Bartolomeo Gosio in Italy. The expedition reached the reserve on December 26, 1900. Koch carried out general examinations of the Papuans , the indigenous people of New Guinea. It struck him that malaria infections were only mild or not recognizable at all, although he could detect the parasites in the blood. The German settlers and Chinese contract workers who had been brought to New Guinea fell ill immediately. The longer they stayed in the country, the more resistance seemed to build up in them too .
This contradicted the prevailing thought in bacteriology until then that an infection was synonymous with a disease. As a result, healthy but infected people became the object of medical measures. Koch recommended screening the blood for the malaria pathogen and the distribution of quinine to all infected people. In the New Guinea town of Stephansort , this strategy also seemed to work for a while. However, Koch's concept was eventually abandoned for cost reasons. The scientific result is that Koch first pointed out the phenomenon of acquired malaria immunity.
Blackwater fever
During a later expedition to German East Africa in 1906, which was mainly about sleeping sickness, Koch also devoted himself to the phenomenon of blackwater fever . In this disease, the red blood cells dissolve, and the urine can turn almost black from hemoglobin. For the colonists in German East Africa, it was the greatest threat. Many doctors thought the disease was a form of malaria and treated it with quinine. Koch was able to prove that this hypothesis and thus also the treatment were wrong. Today, blackwater fever, which is observed almost exclusively in tropical malaria after the use of Chinin, is precisely the result of sensitization to quinine.
Typhoid campaign
Koch's proposals to eradicate malaria in New Guinea through mass screening and quinine therapy had been too expensive for the colonial administration. That is why he looked for a disease in which he could apply his ideas and found it in 1901 in typhus , a salmonella disease that was endemic in Germany .
Koch held the rank of Prussian general à la suite , most of his employees came from the military medical service, and he himself taught at the military medical academy. Thanks to his excellent contacts, he was able to win the Prussian military as an institutional partner for a typhus campaign after he had pointed out the importance of the disease as a war epidemic in several lectures. As a test area, he recommended the area from Trier to Saargemünd , where typhus had occurred in the previous three years. From a military perspective, the area was interesting because it was the staging area of the Schlieffen Plan .

The typhus campaign began with a preliminary test in the high forest near Trier. In order to track down people infected with typhoid, clergy and teachers were interviewed, lists of school attendance and information from local health insurance funds were evaluated. Stool or urine samples were taken from the suspects and examined for bacteriology. Sick and healthy infected people were isolated, and their clothes, linen and homes were disinfected. Some of the doctors involved in the campaign had never seen a person suffering from typhoid, but came to their judgments based solely on bacteriological technology. Allegedly they succeeded in eliminating all typhoid fever cases within three months. Koch ignored the fact that typhoid fever continued to spread in the area.
From 1903 the typhus campaign was extended to an area of 26,000 square kilometers with around 3.5 million inhabitants in south-west Germany. In addition to the examination stations in Trier and Saarbrücken, nine further stations were set up, the medical staff of which last comprised 85 people. They carried out hundreds of thousands of bacteriological examinations and isolated - sometimes under duress - thousands of suspects. Healthy permanent excretors were treated with castor oil , Epsom salt or baking soda for “internal disinfection” , or their gall bladder , which was considered to be the “breeding ground” for typhus bacilli, was surgically removed. They were subject to constant bacteriological monitoring and had to report to the police if they moved. After seven years the incidence of the disease had halved.
"Disease control according to Koch's principles"
In Koch's eyes, the epidemic control method used for typhus was applicable to all infectious diseases, which was later expressed by the term "epidemic control according to Koch's principles". For the first time, the eradication of an infectious disease was seen as a goal. In 1908 the Prussian Ministry of Culture organized a conference solely on the question of the germ carrier, in which numerous Koch students took part. Bacillus carriers were now considered to be a greater danger than visibly ill people. In this style of thinking people were vessels for the multiplication and spread of bacteria.
The Reich Epidemiology Act of 1900 did not contain any regulations on how to deal with healthy bacteria carriers, so that, in the opinion of some doctors, the measures taken had no legal basis. Others argued that the healthy infected should simply be defined as sick within the meaning of the law. In 1906, by an instruction from the Prussian Minister of Medical Affairs, a new category of suspected contagion and disease was created alongside the sick. The actual police force used for isolation and disinfection differed greatly depending on the disease and location.
The Reich Health Council was also set up in 1900 to apply the epidemic laws . It was occupied by numerous former Koch students who brought with them the specific thinking style of the “Koch School”, according to which healthy infected people were considered suspicious. The members of the Reich Health Council are the best way to see how a network of bacteriologists was trained in hygiene and research institutes, the state health administration and the military medical service.
As a result, the German Reich was covered with a network of medical examination offices and hygienic-bacteriological institutes. A special belt of investigation offices in the eastern provinces served to ward off epidemics from the east. Special schools have been set up to train disinfectors . In 1913 there were over 3,500 disinfectors in the Reich.
Failed chemotherapy for sleeping sickness with Atoxyl
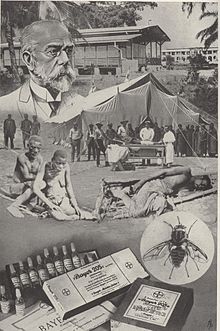
The German public has reacted sensitively to drug trials on humans since the tuberculin scandal, and since 1900 subjects had to give their consent to drug trials due to an "instruction to the heads of clinics, polyclinics and other hospitals from the Minister of Spiritual, Educational and Medical Affairs" give. That's why Koch - like numerous colleagues in German, British and French tropical medicine - switched to the colonies in order to carry out human experiments there without the consent of the local test subjects. In 1902 alarming reports came from German East Africa , which appeared to be threatened by a sleeping sickness epidemic. In fact, there were only isolated cases, at least in German territory, which is why Koch, when he arrived in 1905, finally turned to the Sese Islands in Lake Victoria on British colonial territory. (Koch interrupted his stay to receive the Nobel Prize in December 1905.) The disease was endemic there: within a few years 20,000 people - two thirds of the island's population - had died from it.
Koch experimented with various arsenic preparations, focusing on Atoxyl at the suggestion of Paul Ehrlich . In the short term, the symptoms improved under the therapy, but in the long term he was unable to remove the parasites from the blood. Koch increased the doses up to 1 gram, injected at intervals of seven to ten days. The treatment was very painful and caused dizziness, nausea and colic . When irreversible blindness and death occurred, Koch went back with the dose. Numerous patients - who could not be forcibly interned by the German doctors on British colonial territory - fled from the treatment.
In his recommendations, Koch considered whether the population of entire contaminated districts could be forcibly resettled, but rejected this measure as impractical. He suggested cutting down the forests in these areas in order to combat the vector of the disease, the tsetse fly . He further recommended carrying out serial examinations in contaminated locations, “singling out” the infected and bringing them together in “ concentration camps ”. Although Atoxyl was ineffective and highly toxic, Koch stuck to this agent. The concept behind this was to treat entire populations, as those treated with Atoxyl could not pass the disease on.
After Koch's departure, three sleeping sickness camps were set up with over 1,200 patients. There were no healing successes. What is striking about the published statistics is the extremely high number in the “leaving” category - the patients had escaped by fleeing. Other preparations such as arsenophenylglycine and arsphenamine , which were delivered from Paul Ehrlich's laboratory, were also tested in these camps . This resulted in further deaths. According to a publication in the German Medical Weekly , such attempts were prohibited by the Reich Colonial Office and after 1911 most of the camps and wards in German East Africa were closed. The brutal methods with which sleeping sick were forcibly treated in Togo at the same time cannot be traced back to Robert Koch.
Rivalry with Louis Pasteur
With Louis Pasteur , Koch had a controversy about anthrax vaccination from 1881 on, in which it is difficult to decide what the content was about. With his anthrax research, Pasteur had embarked on an area that Koch saw as his own research area. Pasteur recognized Koch's research, but also made his own priority claims.
The two researchers met on friendly terms at a conference in London in the summer of 1881, and Pasteur praised the much younger chef. A few months later a violent conflict broke out. In the first volume of the communications from the Imperial Health Office , Koch and his students Gaffky and Loeffler attacked Pasteur's research on anthrax vaccination in several articles. They accused him of using unclean cultures and making other mistakes. Pasteur's research has so far yielded nothing. Pasteur answered Koch in detail in a lecture in Geneva in 1882. There was a fatal translation error (Pasteur spoke no German and Koch no French). Ludwig Lichtheim , who sat next to Koch and simultaneously translated for him, interrogated himself at recueil allemand (Pasteur's term for a collection of Koch publications) and translated orgeuil allemand ("German arrogance"), which caused Koch to protest angrily while Pasteur was in progress who had not noticed the misunderstanding, remained incomprehensibly calm to him. Koch's answer to Pasteur's lecture in Geneva was published again. In it, Koch used very insulting tones. He wrote, for example, that Pasteur was not even a doctor and that his anthrax vaccination data were completely worthless; they were only used for aggressive personal polemics. Pasteur replied in 1882 in a long and emotional open letter in which he was surprised at the violent attacks and in turn assessed his research. In 1885 Koch initially criticized Pasteur's rabies vaccination, but a little later took a similar path.
Since France and Germany were again regarded as " hereditary enemies " after the war of 1870/71 , the public press reported on the controversy with strongly nationalistic undertones. Pasteur also met Germany with resentment because of the defeat in 1870/71 (for example, he returned his honorary doctorate from Bonn in 1871).
On the other hand, Koch cooperated excellently with Great Britain. He often conducted research on behalf of the British or carried out German research assignments on British colonial territory.
aftermath
"Cooking School"
Koch separated from many of his former employees in an argument. This does not change the fact that his students occupied key positions at universities and in the state health administration and enforced the specific thinking style of the “Koch School” there. Thanks to the work of Koch and his students, the subject of bacteriology acquired a social prestige within medicine that was otherwise only possible in surgery. Outstanding members of the "Koch School" were:
- Emil von Behring : founder of serum therapy , winner of the first Nobel Prize for Medicine in 1901 (from 1889 to 1895 assigned to the Institute for Hygiene at Berlin University as a medical officer)
- Paul Ehrlich : founder of chemotherapy and immunology , Nobel Prize in Medicine 1908 (from 1890 to 1896 at the Institute for Infectious Diseases in Berlin)
- Paul Frosch : together with Friedrich Loeffler, he demonstrated the pathogen causing foot-and-mouth disease and was one of the founders of virology (from 1887 assistant to Robert Koch at the scientific department of the Institute for Infectious Diseases, from 1899 board member)
- Georg Gaffky : succeeded in breeding the typhoid pathogen Salmonella typhi in 1884 (military doctor, from 1880 to 1888 at the Imperial Health Department, together with Loeffler the first assistant to Koch, followed Koch as director of the Institute for Infectious Diseases)
- Martin Kirchner : 1911–1919 Head of the Prussian Medical Administration (1887–1894 as medical officer at the Hygiene Institute in Berlin)
- Shibasaburo Kitasato : Pure culture of the tetanus pathogen Clostridium tetani , immunological work with Behring (1885–1892 with Koch in Berlin)
- Friedrich Loeffler : together with Paul Frosch, he demonstrated the pathogen causing foot-and-mouth disease and was one of the founders of virology (1879 to 1888 as a military doctor at the Imperial Health Department, from 1880, together with Gaffky, Koch's first assistant)
- Bernhard Nocht : first director of the Institute for Ship and Tropical Diseases in Hamburg (from 1887 to 1890 at the Hygienic Institute)
- Richard Pfeiffer : discovered the bacterium Haemophilus influenzae as the alleged causative agent of influenza (1887 assigned to the Berlin Hygiene Institute as a military doctor, was head of the scientific department there until 1899)
- August Paul von Wassermann : developed a test for the detection of syphilis (1891 to 1906 at the Institute for Infectious Diseases)
- Friedrich Karl Kleine : in the early 1920s he carried out the tests for the first successful drug against sleeping sickness Suramin (Bayer 205, Germanin) from Bayer in East Africa .
- Carl Spengler : From 1892 to 1896 pupil and assistant to Robert Koch at the Robert Koch Institute . Then he was head of the Alexanderhaus sanatorium in Davos, Switzerland, and carried out research on tuberculosis and cancer. The immune body preparations he developed proved to be effective.
Fear of bacteria
Koch founded the idea in German-speaking countries that bacteria are dangerous. It was disseminated, for example, by the “General German Exhibition in the Field of Hygiene and Rescue Services” in Berlin, where Koch certified the danger with photos of bacteria in 1882/1883. The bourgeoisie in particular began to adopt a "hygienically clean" lifestyle. Bacteria remained just as invisible to laypeople as the miasms had previously been. In France, under the influence of Louis Pasteur, microbiology took a different direction, emphasizing the usefulness of microbes - for example in the production of cheese, bread or wine. In Germany, such processes were long considered purely chemical processes under the influence of Justus von Liebig .
The von Koch School had many successes in isolating and identifying pathogens, and emphasized hygiene measures in public health. She also advocated a doctrine of the immutability of microbes, while the Pasteur School emphasized their mutability due to the success of vaccinations with attenuated strains of the pathogen.
Honors
Monuments and plaques
In Wolsztyn , Poland, where Koch had worked as a district physician, a memorial was erected in 2005 on the occasion of the 100th anniversary of the Nobel Prize. Another monument is on the Brijuni Islands ( Croatia ). In addition, at the National Hospital Muhimbili in Dar es Salaam, Tanzania, the bronze commemorative plaque for Robert Koch, which was attached to the Protestant Hospital in 1906, has been located since 1971.
Robert Koch monument on Brijuni
Statue Robert Koch by Louis Tuaillon (1916) in front of the Berlin Charité
Memorial plaque in Dorotheenstrasse 96 in Berlin-Mitte
Berlin memorial plaque on Kurfürstendamm 52 in Berlin-Charlottenburg
Memorial plaque in Luisenstrasse 57 in Berlin-Mitte
Memorial plaque on Nordufer 20 in Berlin-Wedding
Museums
In the Institute for Microbiology and Hygiene of the Charité in the Humboldt University in Berlin there was a Robert Koch Museum from 1960 to 2009 . The Robert Koch Forum is also home to the Robert Koch Library and the Robert Koch Reading Room. In the Robert Koch Institute on Berlin's north bank there is a small museum in the south-western part of the main building that recalls Koch's life and work. The first exhibition at the Robert Koch Institute took place on the occasion of Koch's funeral on December 4, 1910 in the anteroom of the mausoleum. After the annex was completed, a larger museum was set up on the ground floor in 1913. As a result of the renovation in the 1950s, a museum was created in the newly added porch of the main building, which was inaugurated at this location on the 50th anniversary of Robert Koch's death on May 27, 1960. The museum was rebuilt from October 2015 to November 2017 and reopened on December 1, 2017. The redesign and expansion took place in cooperation with the Museum für Naturkunde .
Attached to this is the mausoleum , in which Robert Koch's ashes were buried in a copper urn on December 4, 1910 in the presence of family members, friends and colleagues in the masonry. The official inauguration of the mausoleum, which was built according to Koch's plans, took place on December 10, 1910. On the ground floor of the south-west wing opposite the lecture hall, a large room, in which the photography department was housed during Robert Koch's lifetime, was chosen as a burial place and lined with marble in various shades. The execution was carried out according to plans by the architect Paul Mebes . The western narrow side contains the epitaph executed by the Berlin artist Walter Schmarje with the relief image of Robert Koch. Below is the urn with the ashes in a niche closed by a white marble slab. On the east side of the mausoleum under the heading “Robert Koch - Works and Works”, essential data on the results of his research work are shown. Burial in the mausoleum was possible because at that time there was no law in Prussia on urn burial.
Robert Koch as namesake
The following were named after Robert Koch:
- the Robert Koch Forum (with memorial, formerly together with the Robert Koch Museum )
- the Robert Koch Institute
- the Robert Koch Prize
- the ICE 698 Frankfurt (M) –Berlin Ostbahnhof (June 10, 2001 - December 14, 2002)
- the Robert-Koch-Strasse in many cities
- the Koch Glacier on the Brabant Island in Antarctica
- the Robert Koch Park in Leipzig
- the Robert Koch Park in Böhlen (near Leipzig)
- the Robert Koch Park in Panketal (near Berlin)
Robert Koch Schools
- Robert Koch School (Clausthal-Zellerfeld) , high school with all-day school in Clausthal-Zellerfeld
- Robert Koch School (Frankfurt) , Frankfurt-Höchst
- Robert Koch Secondary School (Dortmund) , Dortmund-Renninghausen
- Robert-Koch-Gymnasium (Berlin) in Berlin-Kreuzberg
- Robert Koch High School (Deggendorf) in Deggendorf
Postage stamps and coins
12 + 38 Pfennig - additional value stamp of the German Post (1944) 100th birthday in 1943
20 Pfennig special stamp of the Deutsche Bundespost Berlin (1960) on the 50th anniversary of death
10 Pfennig special stamp Deutsche Post (1960) for "250 years of Charité"
1 Mark stamp pad from Deutsche Post (1982) on the 100th anniversary of the discovery of the tuberculosis pathogen
144 cents special stamp of the Federal Republic of Germany ( 2005) for "100 years of the Nobel Prize - Robert Koch"
5 mark commemorative coin of the GDR (1968) for the 125th birthday
10 DM commemorative coin of the Federal Republic of Germany ( 1994) for the 150th birthday
There are stamps in honor of Koch with his portrait in numerous other countries, e. B. Bahamas, Belgium, Gabon, Ghana, Congo, Cuba, Upper Volta, Poland, Rwanda, Sweden, South Africa, Tanzania, Thailand, Chad, Vietnam and Zaïre.
Others
Robert Koch's life was filmed in Germany in 1939, based on the novel by Hellmuth Unger , under the title Robert Koch, the fighter of death with Emil Jannings in the title role.
March 24th is celebrated annually by the WHO as " International Day of Tuberculosis ". On March 24, 1882, Robert Koch announced the discovery of the tuberculosis bacterium in a lecture to the Berlin Physiological Society.
Fonts
- Christoph Gradmann (Ed.): Robert Koch. Central texts. Springer Spectrum, 2018.
- Julius Schwalbe, Georg Gaffky, Eduard Pfuhl (eds.): Robert Koch. Collected Works. 3 volumes. Leipzig 1912:
literature
- Wolfgang Genschorek: Robert Koch: Life, Work, Time , with co-worker of Gertraude Genschorek, 2nd through. Edition, Hirzel Verlag, Leipzig 1976.
- Bruno Heymann : Robert Koch. 1. Part 1843–1882 , Leipzig 1932, Part 2: 1882–1908. Fragments (Ed. Georg Henneberg et al.), Berlin 1997
- Bernhard Möllers : Robert Koch. Personality and life's work 1843–1910. Schmorl & von Seefeld Nachf., Hanover 1950.
- Werner Friedrich Kümmel: Koch, Robert. In: New German Biography (NDB). Volume 12, Duncker & Humblot, Berlin 1980, ISBN 3-428-00193-1 , pp. 251-255 ( digitized version ).
- Thomas D. Brock: Robert Koch. A Life in Medicine and Bacteriology. Science Tech, Madison (Wisconsin) 1988.
- Robert Koch Institute History at a Glance , Texts: Ragnhild Münch, Images: Robert Koch Estate and RKI Image Archive, Layout Günter Bredow, Print: RKI's in-house printing facility, Berlin 2000.
- Manfred Vasold: Robert Koch, the discoverer of pathogens. Spectrum of Sciences Publishing Company, Heidelberg 2002, ISBN 3-936278-21-0 .
- Christoph Gradmann : Illness in the laboratory. Robert Koch and medical bacteriology. Wallstein, Göttingen 2005, ISBN 3-89244-922-8 .
- Johannes W. Grüntzig , Heinz Mehlhorn : Expeditions into the realm of epidemics. Medical ascension orders of the German imperial and colonial times. Spectrum Akademischer Verlag, Heidelberg 2005, ISBN 3-8274-1622-1 .
- Johannes W. Grüntzig, Heinz Mehlhorn: Robert Koch. Plague hunters and Nobel Prize winners. Spektrum Akademischer Verlag, Heidelberg 2010, ISBN 978-3-8274-2710-6 .
- Paul de Kruif : Robert Koch. The fighter of death. In: Paul de Kruif: Microbe hunters. (Original edition: Microbe Hunters. Harcourt, Brace & Co., New York 1926) Orell Füssli Verlag, Zurich / Leipzig 1927; 8th edition, ibid. 1940, pp. 102-137.
- Barbara Rusch: Robert Koch. From country doctor to pioneer of modern medicine. Bucher, Munich, 2010, ISBN 978-3-7658-1823-3 .
- Friedrich Hoffmann : Deadly Worlds - The incredible story of three doctors who saved millions of lives. Herder, Freiburg im Breisgau 2010, ISBN 978-3-451-06202-5 .
- Werner Köhler : Koch, Heinrich Hermann Robert. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. de Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 767 f.
- Claude E. Dolman: Koch, Heinrich Hermann Robert . In: Charles Coulston Gillispie (Ed.): Dictionary of Scientific Biography . tape 7 : Iamblichus - Karl Landsteiner . Charles Scribner's Sons, New York 1973, p. 420-435 .
- Ragnhild Münch: Robert Koch and his estate in Berlin. de Gruyter 2003
Web links
- Literature by and about Robert Koch in the catalog of the German National Library
- Newspaper article about Robert Koch in the press kit of the 20th century of the ZBW - Leibniz Information Center for Economics .
- The collected works of Robert Koch , digitized by the Robert Koch Institute
- Susanne Eckelmann: Robert Koch. Tabular curriculum vitae in the LeMO ( DHM and HdG ) (not entirely reliable)
- Information from the Nobel Foundation on the 1905 award ceremony for Robert Koch (English)
- Microscope from Robert Koch's laboratory in Wollstein (1877) and microscope lenses of the type with which Robert Koch achieved the breakthrough in the photographic reproduction of pathogenic microorganisms (1877–1878)
- Golf Dornseif, Professor Robert Koch and colonial malaria research (PDF; 1.6 MB)
Individual evidence
- ↑ Barbara Rusch: Robert Koch. From country doctor to pioneer of modern medicine. Munich 2010, p. 19.
- ↑ Barbara Rusch: Robert Koch. From country doctor to pioneer of modern medicine. Munich 2010, pp. 19 and 20.
- ↑ a b c d e Werner Friedrich Kümmel: Koch, Robert. In: New German Biography [online version]. 1979, pp. 251-255, accessed on May 29, 2020 ( archived version in the Internet Archive ).
- ^ Ragnhild Münch: Robert Koch and his legacy in Berlin . Walter de Gruyter, 2012, p. 98.
- ↑ Jürgen Zimmerer, DER SPIEGEL: Robert Koch: The famous researcher and human experiments in Africa - DER SPIEGEL - history. Retrieved June 3, 2020 .
- ↑ Robert Koch . In: New Free Press . Vienna May 31, 1910, p. 10 ( ANNO - AustriaN Newspapers Online [accessed on May 27, 2020]).
- ^ A Robert Koch mausoleum . In: Neues Wiener Journal . Vienna December 11, 1910, p. 13 ( ANNO - AustriaN Newspapers Online [accessed May 27, 2020]).
- ^ The ashes of Robert Koch . In: Neues Wiener Journal . Vienna June 11, 1910, p. 5 ( ANNO - AustriaN Newspapers Online [accessed on May 27, 2020]).
- ^ Heinrich Hermann Robert Koch at knerger.de
- ↑ Christoph Gradmann: Laboratory Disease, Robert Koch's Medical Bacteriology . The Johns Hopkins University Press, Baltimore 2009, ISBN 978-0-8018-9313-1 , pp. 63-65.
- ↑ Robert Koch: Investigation on the etiology of wound infectious diseases. Vogel, Leipzig 1878. Digitized and full text in the German text archive
- ↑ Sylvelyn Hähner-Rombach: Künstlerlos and arms destiny. About the different perceptions of tuberculosis. In: The great dying. Epidemics make history. Jovis, Berlin 1999, pp. 278-307, here p. 291.
- ↑ Axel C. Hüntelmann: Paul Ehrlich: Life, Research, Economics, Networks. Wallstein, Göttingen 2011, ISBN 978-3-8353-0867-1 , p. 150.
- ^ Gradmann: Laboratory Disease ..., p. 77.
- ^ Gradmann: Laboratory Disease ..., p. 77.
- ↑ Robert Koch: The Aetiology of Tuberculosis. In: Berliner Klinische Wochenschrift. Volume 19, No. 15, 1882, pp. 221-230.
- ↑ Manfred Vasold: Robert Koch, the discoverer of pathogens. Spectrum of Sciences, Publishing Company, Heidelberg 2002, ISBN 3-936278-21-0 , p. 75.
- ^ Alfred Grotjahn: Experienced and strived for, memories of a socialist doctor. Herbig, Berlin 1932, p. 51.
- ↑ Vasold: Robert Koch ..., p. 80.
- ^ Gradmann: Laboratory Disease ..., p. 106.
- ^ Gradmann: Laboratory Disease ..., p. 101.
- ↑ quoted from Vasold: Robert Koch ..., p. 81.
- ^ Gradmann: Laboratory Disease ..., p. 133 f.
- ^ Gradmann: Laboratory Disease ..., p. 136.
- ↑ Eckart Klaus Roloff : Hero in the Twilight. Robert Koch - the famous doctor, honored with the Nobel Prize 100 years ago, has great merits. Its fatal errors and mistakes are less known. In: Rheinischer Merkur. (Bonn), No. 49 of December 8, 2005, p. 35.
- ↑ Gradmann: Laboratory Disease ..., p. 100 f.
- ^ Christoph Gradmann: Locating Therapeutic Vaccines in Nineteenth-Century History. In: Science in Context. Volume 21, No. 2, 2008, pp. 145-160, here p. 155.
- ↑ Ernst Bäumler: colors, formulas, researchers. Hoechst and the history of industrial chemistry in Germany. Piper, Munich / Zurich 1989, p. 67.
- ^ Courmont, quoted in M. Roussel: Éloge du professeur Arloing. In: Bull. Acad. vét. Fr.:. LXXXV, 1932, p. 429-448.
- ^ Gradmann: Laboratory Disease ..., p. 111 f.
- ^ Gradmann: Laboratory Disease ..., p. 184 f.
- ^ Gradmann: Laboratory Disease ..., p. 191.
- ^ Gradmann: Laboratory Disease ..., pp. 37-39.
- ↑ a b Real Academia de la Historia (ed.): Joaquín Balcells y Pasqual , 2018, archive link (Spanish)
- ↑ Col·legi Oficial de Metges de Barcelona (ed.): Joaquim Balcells i Pascual , 2015, archive link ( Catalan )
- ↑ da Costa Simões, António Augusto / de Macedo Pinto, José Ferreira: Relatório da Direcção do Hospital de Cholericos de NS da Conceição em Coimbra , 1856, Coimbra: Imprensa da Universidade (Portuguese)
- ↑ The presentation of the cholera epidemic in Hamburg follows Michael Dorrmann: "The Asian monster", The Cholera in the 19th century. In: The great dying. Epidemics make history. Jovis, Berlin 1999, pp. 204-251, here pp. 237-246.
- ^ FJ Krause: A man cleans up. Robert Koch and cholera in Hamburg. In: Senioren Magazin Hamburg, June 2020, pp. 12-14.
- ↑ Vasold: Robert Koch ..., p. 64.
- ↑ A. Schiff: About the occurrence of typhus bacilli in the bile of typhus patients and "typhus bacilli carriers" . In: Wiener Medical Wochenschrift . No. 36 . Moritz Perles , Vienna September 2, 1905, Sp. 1763 f . ( ANNO - AustriaN Newspapers Online [accessed May 27, 2020]).
- ↑ The presentation on New Guinea follows Wolfgang U. Eckart: Medicine and Colonial Imperialism, Germany 1884–1945. Ferdinand Schöningh, Paderborn, 1997, ISBN 3-506-72181-X , pp. 402-409.
- ^ Hugo Kronecker : Hygienic topography. In: A. Pfeiffer (Ed.): 21st annual report on progress and achievements in the field of hygiene. Born in 1903. Verlag Friedrich Vieweg and Son, Braunschweig 1905, p. 68.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 9–223, here: p. 172.
- ↑ Vasold: Robert Koch ..., p. 98 f.
- ↑ The description of the typhus campaign follows Silvia Berger : Bacteria in War and Peace. A history of medical bacteriology in Germany 1890–1933. Wallstein, Göttingen 2009, ISBN 978-3-8353-0556-4 , pp. 143-170.
- ↑ Medical research with minors → Legal aspects , on drze.de
- ↑ Eckart Klaus Roloff : Hero in the Twilight. Robert Koch - the famous doctor, honored with the Nobel Prize 100 years ago, has great merits. Its fatal errors and mistakes are less known. In: Rheinischer Merkur. (Bonn), No. 49 of December 8, 2005, p. 35.
- ↑ The presentation in this section follows Eckart: Medicine and Colonial Imperialism…, pp. 340–349.
- ↑ Wolfgang U. Eckart: The colony as a laboratory. In: Cultural history of human experimentation in the 20th century. Edited by Birgit Griesecke, Marcus Krause, Nicolas Pethes, Katja Sabisch. Suhrkamp, Frankfurt 2009, pp. 199-227, here p. 220, names arsenic acid, the arsenic-containing nucleogen from H. Rosenberg (Berlin), arsenic ferratin from GF Boehringer and Sons (Mannheim); also Trypan red and Afridol blue from Fr. Bayer's paint factory (Elberfeld). With the last-mentioned dyes, the pain was so severe after the injection that Koch could not repeat the experiment.
- ↑ Axel C. Hüntelmann: Paul Ehrlich: Life, Research, Economics, Networks. Wallstein, Göttingen 2011, ISBN 978-3-8353-0867-1 , p. 167 f.
- ↑ Wolfgang U. Eckart: Illustrated history of medicine . Springer, 2010, ISBN 978-3-642-12609-3 ( page 308 in the Google book search).
- ↑ Jürgen Zimmerer, DER SPIEGEL: Robert Koch: The famous researcher and human experiments in Africa - DER SPIEGEL - history. Retrieved June 3, 2020 .
- ^ Agnes Ullmann : Pasteur-Koch: Distinctive Ways of Thinking about Infectious Diseases. ( Memento of May 10, 2016 in the Internet Archive ) In: asm.org .
- ↑ The information in this section is compiled from Wolfgang U. Eckart , Christoph Gradmann : Ärztelexikon: From antiquity to the 20th century. CH Beck, Munich, 1995, ISBN 3-406-37485-9 .
- ↑ Cf. also Eva Anne Jacobi: The sleeping sickness medication Germanin as a propaganda instrument: Reception in literature and film at the time of National Socialism. In: Würzburg medical history reports. Volume 29, 2010, pp. 43-72.
- ↑ Carl Spengler: Peter Bollier. In: Historical Lexicon of Switzerland . February 14, 2012 , accessed March 29, 2017 .
- ^ History of the mausoleum and museum on the Robert Koch Institute website
- ^ ICE named after Robert Koch , Goslarsche Zeitung of July 19, 2001.
- ↑ Koch, Robert (1843–1910) , p. 1, on catawiki.nl
- ↑ Koch, Robert (1843–1910) , p. 2, on catawiki.nl
- ↑ Hellmuth Unger: Robert Koch. Novel of a great life. Publishing house of the German Medical Association, Berlin 1936.
- ↑ Niels Martens: Robert Koch - Fighter of Death. In: uni-kiel.de
- ^ Heidrun Riehl-Halen: The German-language tuberculosis film in medical education and training and in public education (1913–1973). Dissertation at the Institute for the History of Medicine (today: History and Ethics of Medicine), Ruprecht-Karls-Universität Heidelberg, supervisor Wolfgang U. Eckart . 1998. On the film “Robert Koch, the fighter of death” pp. 87–93. Video cassette
| personal data | |
|---|---|
| SURNAME | Koch, Robert |
| ALTERNATIVE NAMES | Koch, Heinrich Hermann Robert (full name) |
| BRIEF DESCRIPTION | German physician and microbiologist |
| DATE OF BIRTH | December 11, 1843 |
| PLACE OF BIRTH | Clausthal |
| DATE OF DEATH | May 27, 1910 |
| Place of death | Baden-Baden |