anthrax
| Classification according to ICD-10 | |
|---|---|
| A22 | Anthrax (anthrax) - infection caused by Bacillus anthracis |
| ICD-10 online (WHO version 2019) | |

Anthrax or anthrax (from ancient Greek ἄνθραξ anthrax "coal") is an acute infectious disease that is caused by Bacillus anthracis and mostly affects cloven-hoofed animals , but also other herbivorous animals. This zoonosis can also affect humans if they are exposed to anthrax spores, which can also be transmitted from animals to humans. Human-to-human transmission is very unlikely; no such case has yet been documented.
The causative agent of anthrax is an aerobic and spore-forming rod bacterium . The anthrax toxin produced by the pathogen is highly toxic. When humans are infected, the skin and mucous membranes are usually affected, and less often the lungs or digestive tract. The spores can survive for decades or even centuries.
Due to its suitability as a biological weapon and the search for defense options, the mode of action of the anthrax pathogen and the course of the disease have been well researched. Among other things, research is being carried out into using the cell toxin effect selectively against cancer cells.
etymology
The term anthrax is derived from the brown-black spotty discoloration of a severely affected spleen , which was also found filled with black blood in sections of animals.
The Greco-Latin and scientific name Anthrax ( Greek ἄνθραξ anthrax "coal") is based on the blackish color with carbuncles (from Latin carbunculus: small coal ') designated boils with skin anthrax and other formerly karbunkelähnlichen ulcers. For Hippocrates , “anthrax” did not refer to the anthrax bump, but to the smallpox disease.
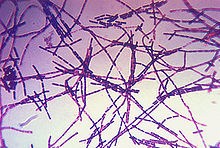
Pathogen
The anthrax pathogen, Bacillus anthracis , belongs to the genus Bacillus (spore-forming, aerobic rod bacteria) within the family Bacillaceae . It is an approximately five to six µm (1 µm = 0.001 mm) long, gram-positive , immobile, spore-forming rod that forms short, in culture longer, chain-like associations in body fluids (" serpentine " or " Medusa head " shape). In the animal body, the bacterial cell is encased in a clear capsule (consisting of D- glutamate ), while in the culture no capsule formation is usually recognizable. Outside the animal's body, in the presence of oxygen and at temperatures of 12 to 43 ° C, spores (permanent forms) are formed, the size of which is around 0.5 to 1.2 µm.
The bacterium itself is not very resistant. In the rotting, unopened carcass, the germs perish after two to three days in warm weather. At low temperatures, they can remain infectious for two weeks. They are killed in the gastric juice after about 20 minutes. The spores of the anthrax pathogen, on the other hand, are exceptionally insensitive. They are not destroyed by drying out. Sun exposure will kill them within four days. In the ground and protected from the sun, they remain viable for many decades. Ten percent formaldehyde is effective after about two hours, 20 percent formaldehyde in about ten minutes. In the flowing steam of 100 ° C they perish after five minutes, in dry heat from 120 ° C to 140 ° C after three minutes.
Anthrax pathogens were detected microscopically in sheep's blood by Aloys Pollender in 1849, but it was Robert Koch who systematically examined the pathogen and described it in more detail in 1876. Koch was able to reproduce Bacillus anthracis in culture and demonstrate its role in the development of the disease. Grigorij Nikolaevič Minch (1836–1896), who worked as a pathologist in Kiev from 1876 to 1895 , recognized the common origin of intestinal anthrax and pulmonary anthrax .
distribution
Today anthrax occurs in all countries and in all parts of the world, but the frequency varies greatly. In Germany the disease occurs only very rarely. Anthrax is most common in warmer regions, especially southern Europe, the Middle East, Asia, North Africa, and South America. The pathogen is found primarily on damp, swampy soils and in floodplains by rivers and streams, where the spores can be carried away and spread by the water.
Even from deeply buried carcasses, the activity of earthworms or rising groundwater can cause spores to come to the surface again and again after decades. If, in the course of construction work, the areas of former stoneworks, waterworks or tanneries are cut, which decades ago were still far outside the urban periphery , spores can be carried back upwards.
The majority of anthrax cases were found in grassland and grazing areas. In terms of the season, a high point is emerging in spring, while the statistical low point is in summer (June). Even in years with extremely high amounts of precipitation, more cases of illness must be expected.
With regard to the occurrence in various domestic and wild animal species as well as in humans, their varying degrees of susceptibility play a role. Sheep, goat, cattle, buffalo, horse, camel, reindeer, elephant and mink are highly susceptible; moderately receptive dog, cat, rat and human. Pigs are less receptive and birds are almost resistant (with the exception of the ostrich).
Forms of manifestation, symptoms and therapy
Skin anthrax
The cutaneous anthrax is the most innocent and most common form of anthrax. It is only transmitted through direct skin contact; if left untreated, 5 to 20% of cases are fatal. If there is an infection, a vesicle-lined ulcer with a black necrosis in the middle forms at the point of transmission (hence the name of the anthrax bacteria: Gr. Anthrax for "coal", "black"). A pus-filled vesicle develops from this. As the disease spreads further, new vesicles appear. When these vesicles combine, an anthrax carbuncle develops , which, if attached to a blood vessel, can lead to blood poisoning . Skin anthrax is treated with systemic ciprofloxacin , and if sensitivity is proven, penicillin G (alternatively also doxycycline or penicillin V ) is treated. Skin and pulmonary anthrax used to be common occupational diseases of butchers and especially tanners.
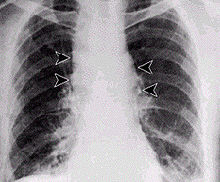
Pulmonary anthrax
Inhalation of spore-containing dust causes pulmonary anthrax , also called rag disease . For an outbreak of disease (apparent infection), about 3000–9000 anthrax spores, which adhere to animal skins or hair and are contagious even after years, have to be inhaled with the air. The incubation period ranges from a few days to several weeks. The illness begins unspecifically and similar to the flu with a cough , followed by a high fever , chills and shortness of breath . The coughed up secretion is highly infectious. Even with immediate antibiotic therapy (ciprofloxacin, doxycycline, penicillin G or V), the mortality (death rate) from pulmonary anthrax is very high, since the occurrence of the symptoms has already resulted in a massive release of the anthrax toxins. Death usually occurs within three to six days with the picture of septic shock .
Intestinal anthrax
Intestinal anthrax is transmitted by eating infected dairy products or infected meat . The incubation period is a few hours to three days. Bloody vomiting and bloody diarrhea occur, which are signs of bloody bowel inflammation. The germs spread all over the body, blood poisoning and heart and kidney failure can occur. Over 50% of the sick die. This is the rarest form of anthrax. Intestinal anthrax, like lung and skin anthrax, is treated with broad spectrum antibiotics such as ciprofloxacin (also doxycycline or penicillin G or V). Oropharyngeal anthrax can also develop after oral ingestion of anthrax spores (edema and necrosis in the neck area).
Diagnosis
When talking to the patient, the course of the disease over the past few days must be investigated very carefully (anamnesis). Information about possible occupational exposure and contact with animals is important for the doctor. For the diagnosis of skin anthrax, an examination of the above-mentioned typical skin changes on the entire body of the patient is necessary.
As a safeguard, the anthrax bacilli are obtained from the skin damage or, if pulmonary anthrax is suspected, from the sputum and examined microbiologically. If necessary, a blood sample will also be examined. Three methods can be used to detect the pathogen. On the one hand, the pathogen is detected directly under the microscope. On the other hand, the detection can be made using a bacterial culture. Thirdly, molecular biological detection is possible using PCR . A rapid test has recently been developed for this purpose.
Prevention and Regulations
If there is suspicion that inhalative anthrax exposure, for example in the context of a bioterrorist attack, has taken place, a 60-day prophylaxis (or 100-day prophylaxis according to the recommendations of the US health authority CDC ) with an antibiotic ciprofloxacin , doxycycline (or Amoxicillin in pregnant women) in combination with clindamycin or rifampicin .
In June 2013, an anthrax vaccine , trade name BioThrax , made by Emergent BioSolutions was approved in Germany. The vaccine consists of filtered antigens. Use of the vaccine is only recommended in adults.
In Russia there is a live vaccine with the strain Bacillus anthracis СТИ-1.
In animals, anthrax is a notifiable animal disease in Germany in accordance with Section 4 of the Animal Health Act in conjunction with Section 1 of the Ordinance on Notifiable Animal Diseases . In Austria it is notifiable for animals in accordance with Section 16 of the Animal Diseases Act. In Switzerland, anthrax is notifiable as an animal disease to be eradicated within the meaning of Article 3 of the Animal Diseases Ordinance (TSV) with extensive obligations under Articles 132-134.
In humans, anthrax is a reportable disease in Germany according to § 6 and § 7 of the Infection Protection Act . There is an obligation to report in the event of suspicion, illness and death, as well as evidence of the pathogen. In Austria, it is a notifiable disease in accordance with Section 1 (1) of the 1950 Epidemic Act . Cases of suspicion, illness and death must be reported. In Switzerland, anthrax is also a reportable disease according to the Epidemics Act (EpG) in conjunction with the Epidemics Ordinance and (Appendices 1 and 3) the Ordinance of the FDHA on the reporting of observations of communicable diseases in humans.Reporting of a clinical suspicion is required, Consultation with a specialist in infectious diseases and initiation of a pathogen-specific laboratory diagnosis or notification of a positive laboratory diagnosis regarding the pathogen.
In the event of occupational exposure, the trade association must also be informed. When working in contaminated areas with suspected anthrax, the trade association leaflet BGI 583 "Biological agents in soil remediation" must be observed.
history
Anthrax has been known as a disease and malignant epidemic since ancient times. It is reported by both the Greeks ( Homer ) and the Romans ( Ovid ). The ancient Arab doctors called anthrax in humans "Persian fire". There is much to suggest that some epidemics that have been passed down as plague or dysentery epidemics were in fact anthrax epidemics. The epidemic, which Jeremias Gotthelf describes in his novella “The Black Spider” , can also be interpreted as anthrax.
Anthrax has long been known as a wild disease . There are reports of real epidemics as early as the ninth century . After the epidemic in the domestic animal population could be suppressed as a result of the advancing knowledge of microbiology, it has only been found sporadically in game in recent decades.
Anthrax in tanneries
In the past, the occurrence of anthrax was mostly linked to the importation of infected animals or animal hides for leather production or to the importation of pelts, hair and bristles. Anthrax spores survived the preservation of leather and the tanning process and found their way into the waterways via the tannery wastewater and into the affected river plains and pastures during floods. There are numerous historical known anthrax epidemics in domestic animals downstream from tanneries. These animal epidemics declined at the beginning of the 20th century after some violent protests by affected farmers after the direct discharge of tannery wastewater was banned in many places and the wastewater was instead roughly clarified and trickled .
Anthrax in humans occurred primarily as an occupational disease in tannery workers (see history of tannery ) and in people who processed hides, bristles and hair (e.g. in mattress production), but also in port and transport workers who had to deal with these materials, also with skimmers . The high points of the occurrence were times of crisis in the leather industry, when more and more cheap animal hides were imported from regions with little or no veterinary control of the slaughter. With the decline in production in these branches of industry and with increasing veterinary checks in the countries of origin of the animal products, the number of cases of illness has decreased to such an extent that cases of anthrax have become extremely rare today.
In the abandoned polluted by contaminated sites of the leather industry they are considered as potentially contaminated with anthrax. In a corresponding research project, virulent anthrax spores could still be detected in Germany over 40 years after the plant was closed. On the other hand, according to these surveys, no cases of anthrax disease in humans or animals due to contact with relevant contaminated materials are known. The risk of anthrax can also be regarded as largely eliminated if historical surveys and testimonies from contemporary witnesses confirm that no anthrax diseases occurred during the former production, and especially if only domestic hides from slaughtered by a veterinarian were used.
Events in the 21st century (selection)
In July 2001, hundreds of bison were threatened in Alberta, Canada . 19 animals died as a result of the pathogen.
On July 12, 2001 in Changyong County, Gyeongsangnam-do Province , South Korea, five human anthrax cases occurred and one person died. All had eaten meat from a beef found dead in a swampy area.
In 2008 there was an accumulation of anthrax cases in cattle in the eastern French department of Doubs , after the disease had practically never occurred there for over 40 years. By August 2008 the disease had been found in 21 cattle farms, 40 animals had to be killed.
In 2010, anthrax-contaminated heroin caused seven deaths in Scotland and one death in Germany.
In early April 2010 a skin anthrax infection became known in the Aachen area.
In August and September 2010, around 300 people were infected with anthrax in Bangladesh . In addition, over 200 cows and goats fell ill and 50 animals died.
In 2012 a drug addict died of anthrax-contaminated heroin in the Regensburg area .
In July 2012, there was an outbreak of anthrax in a herd of cattle in the Stendal district ( Saxony-Anhalt ). The diagnosis was confirmed by the Friedrich Loeffler Institute in Jena . According to the Ministry of Agriculture, nine cattle had died by July 13, the origin of the pathogen was still unclear at that time.
In June 2014, 86 researchers accidentally came into contact with the anthrax pathogen in a laboratory of the US health authority Centers for Disease Control and Prevention (CDC), because the spores were not killed, contrary to safety regulations. The rooms were decontaminated after the breakdown was discovered and the employees concerned treated as a precaution.
In 2016, anthrax broke out in Russia on the Siberian Yamal Peninsula , which was initially attributed to a historic Yamal-Nenets grave . Experts attributed the recurrence of the disease to the climatic changes , which thawed reindeer carcasses buried in the permafrost from an epidemic decades ago and pathogens could become active again.
Use as a biological weapon
Opinions differ as to the extent to which anthrax bacteria are suitable for biological warfare . Based on experiments with primates, scientists estimate the lethal dose LD 50 at 2,500 to 55,000 inhaled spores.
The spores are insensitive to external influences and are therefore significantly more suitable than the plague bacterium Yersinia pestis, for example .
Until 1945
In the Middle Ages, contaminated animal carcasses were thrown over castle walls during armed conflicts in order to infect the opposing population.
During the First World War , German scientists experimented with anthrax. The attempts were discontinued due to poor success.
At the Tokyo Institute for Epidemic Prevention, the military doctor Ishii Shirō and his colleagues experimented with various pathogens from 1930, including the anthrax. They carried out experiments on Chinese and Korean prisoners of war. In 1932 these experiments were relocated to the village of Beyinhe in occupied Manchuria in order to be able to keep them more secret and to exclude potential dangers for their own population. In 1936, biological weapons research was relocated to Pingfang, south of Harbin , to unit 731 .
In addition to Japan, France also developed an anthrax pathogen. This was discovered when the German troops marched in and, although Hitler strictly rejected biological weapons, German scientists experimented with the pathogen.
In the winter of 1942 and spring 1943, Great Britain tested anthrax pathogens in the form of “beef cakes” on sheep on Gruinard Island ( Operation Vegetarian ), after which the island was a restricted area for almost fifty years. The island was decontaminated in 1986 and 1987 with a total of 280 tons of formaldehyde and the land was sold to the descendants of the previous owners in 1990.
The US worked on anthrax bombs during World War II . Winston Churchill asked US President Roosevelt for an accelerated delivery of 500,000 "N-bombs" that had previously been developed and tested at the Dugway Proving Ground .
1970s
The Soviet Union also experimented with anthrax. In April 1979, in the anthrax accident in Sverdlovsk, numerous residents were infected with anthrax in a biological weapons research facility. The infected were in the direction of the wind at the time, when probably only about one gram of the anthrax pathogen was released. It was only when the industrial accident became public under Boris Yeltsin in 1992 that the families of the deceased learned what had caused their family members to die. The journal Science published the results of the American-Russian commission of inquiry in 1994 - it is the most thorough documentation of a biological weapon effect to date.
The entire former island of rebirth , which was formerly located in the Aral Sea , is contaminated with anthrax. It was a secret test area of the Soviet army; it is said that anthrax bacteria were still exposed there in 1988. Due to the withdrawal of water from the tributaries of the Aral Sea, the water level has meanwhile sunk so much that in 2000 the former island connected to the mainland.
In 1972, 143 states signed the Biological Weapons Convention , which prohibits the development, manufacture and storage of biological weapons.
1990s
In the 1990s, the Sverdlovsk accident became public knowledge, as well as the fact that Iraq was storing large quantities of anthrax for filling warheads and bombs . Negotiations on an additional protocol then began, which ended after six years. This protocol still leaves many loopholes, and since factory inspections must be announced well in advance, traces can be removed. The USA withdrew from the additional protocol on the grounds that it was not going far enough. The United States itself conducts research into the defense against biological threats. This includes B. the development of vaccines or diagnostic tests.
The presumed production and storage of, among other things, biological weapons as weapons of mass destruction in the Iraq conflict , after a tug-of-war over weapons inspections in 2003, served the USA as essential legitimation to start the Iraq war . It later turned out that these assumptions or supposed evidence were unfounded.
2000s
In September and October 2001, a total of seven letters containing anthrax pathogens of varying degrees of virulence were sent to government agencies and high-ranking politicians in the case of anthrax attacks in the United States . Five people died. A presumed connection with the terrorist attacks on September 11, 2001 could not be proven. Instead, domestic laboratory personnel are held accountable because the anthrax pathogens sent were the same as strains grown at the U.S. Army Medical Research Facility for Infectious Diseases ( USAMRIID ) at Fort Detrick . The main suspect US scientist Bruce Edwards Ivins committed suicide in July 2008. In connection with the anthrax letters in the USA, spores of the anthrax pathogen were also detected in Kenya in a letter to a private individual on October 18, 2001 .
literature
- RC Spencer: Bacillus anthracis . In: Journal of Clinical Pathology , 56, 2003, 3, pp. 182-187. Review. PMID 12610093 . ISSN 1472-4146
- W. Biederbick, R. Fock, K. Güttler, C. Veit: Infections by Bacillus anthracis. In: Dtsch. med. Weekly , Stuttgart 15.2002,127, pp. 809-814. ISSN 0012-0472
- Paul Richter: The Significance of Anthrax for the History of Epidemics. In: Sudhoffs Archiv , 6, 1913, pp. 281–297.
- Thomas Schlich: Anthrax. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 992 f.
- Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid 1961, pp. 9-223, here: pp. 218 f.
Web links
- Anthrax - information from the Robert Koch Institute
- Anthrax (anthrax) - Information from the Federal Ministry for Social Affairs, Health, Care and Consumer Protection, Austria
- Anthrax in animals and humans - information from the Federal Food Safety and Veterinary Office (FSVO), Switzerland
- Information from the Centers for Disease Control and Prevention, USA (English).
- Text of the ordinance on protection against anthrax and intoxicating fire
Individual evidence
- ^ S. Liu, H. Aaronson, DJ Mitola, SH Leppla, TH Bugge: Potent antitumor activity of a urokinase-activated engineered anthrax toxin. In: Proceedings of the National Academy of Sciences . Volume 100, number 2, January 2003, pp. 657-662, doi: 10.1073 / pnas.0236849100 , PMID 12525700 , PMC 141052 (free full text).
- ↑ See Anthrax at Duden online
- ↑ Georg Sticker : Hippokrates: The common diseases first and third book (around the year 434-430 BC). Translated from the Greek, introduced and explained by Georg Sticker. Johann Ambrosius Barth, Leipzig 1923 (= Classics of Medicine. Volume 29); Unchanged reprint: Central antiquariat of the German Democratic Republic, Leipzig 1968, p. 102.
- ↑ J. Stahnke: Ludwik Teichmann (1823–1895). Anatomist in Krakow. In: Würzburg medical history reports. Volume 2, 1984, pp. 205-267; here: p. 216.
- ^ Louis Pasteur : Sur les virus-vaccins de choléra des poules et du charbon. In: Louis Pasteur Vallery-Radot (ed.): Oeuvres de Pasteur Réunies. Volume VI, Masson et Cie., Paris 1933, p. 367. Reprinted from: Comptes rendus des travaux du Congrès international des directeurs des stations agronomiques, session de Versailles. Berger-Levrault & Cie, June 1881, pp. 151-162.
- ↑ So z. B. in Trier , where the area of a tannery that had been closed for decades was examined: http://www.trier-reporter.de/spitzmuehle-erde-kom-in-faesser-und-wird-verbrannt/
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 184.
- ↑ Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid 1961, pp. 9-223, here: pp. 218 f.
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. 2009, p. 184.
- ↑ BioThrax [R] Adsorbed Anthrax Vaccine; Suspension for injection; Emergent Sales and Marketing Germany GmbH branch in Bruchsal. In: PharmNet.Bund - Arzneimittel-Informationssystem / dimdi.de. Retrieved on March 14, 2020 (German): "Anthrax-Antigen-Filtrat"
- ↑ Anthrax vaccines (anthrax). (HTLM) In: pei.de. Paul Ehrlich Institute, February 3, 2020, accessed on March 14, 2020 : "Use from an age of 18 years"
- ↑ pharmacopoeia.ru
- ↑ Notifiable animal diseases. Federal Ministry of Food and Agriculture (BMEL), August 2, 2019, accessed on March 14, 2020 .
- ^ The Swiss Federal Council: Animal Disease Ordinance (TSV). In: admin.ch. Retrieved on March 14, 2020 (Swiss Standard German, June 27, 1995 (as of January 1, 2020)).
- ↑ Anthrax in animals and humans. Federal Food Safety and Veterinary Office FSVO, accessed on March 14, 2020 (Swiss Standard German): “ Anthrax is an animal disease that must be exterminated and therefore notifiable. Anyone who keeps or looks after animals must report suspected cases to the herd veterinarian. »
- ^ Ordinance of the FDHA on the reporting of observations of communicable diseases in humans. from December 1, 2015 (as of February 1, 2020). Federal Chancellery, accessed on March 13, 2020 .
- ↑ Stefan Winkle: Scourges of humanity . Artemis & Winkler 1997
- ↑ Hans Killian: There is only God behind us. Sub umbra dei. A surgeon remembers. Kindler, Munich 1957; here: Licensed edition as Herder paperback (= Herder library. Volume 279). Herder, Freiburg / Basel / Vienna 1975, ISBN 3-451-01779-2 , pp. 60–81.
- ↑ Umweltbundesamt (Ed.): Guide - Exploring former tannery sites . 1998. Project executing agency: Waste management and remediation of contaminated sites, State Office for Nature and the Environment of Schleswig-Holstein, Geology / Soil Department, Contaminated Sites Department.
- ^ Anthrax in Eastern France. In: Dt. TAB. Issue 11 (2008), p. 1542.
- ↑ Eight deaths from anthrax-contaminated heroin. In: Welt Online . January 19, 2010, accessed January 20, 2010 .
- ↑ rp-online.de ( Memento from April 19, 2010 in the Internet Archive ) Slight case of anthrax
- ↑ Officials work to control anthrax outbreak in Bangladesh. Retrieved September 6, 2010 .
- ↑ Anthrax spores: heroin addict died of anthrax in Bavaria . Mirror online
- ^ Anthrax cattle recovered from the Elbe. In: Spiegel Online . July 13, 2012, accessed July 13, 2012 .
- ^ Anthrax in cattle in Saxony-Anhalt. Greenpeace, July 12, 2012, accessed July 12, 2012 .
- ↑ Anthrax alert: sloppiness in the US health department's laboratory. Spiegel Online, June 20, 2014, accessed June 20, 2014 .
- ↑ orf.at 86 US researchers probably exposed to anthrax pathogens, ORF.at of June 21, 2014.
- ↑ anthrax in Siberia erupted on online 1 August 2016; accessed on August 5, 2016
- ↑ Russia: twelve-year-old died of anthrax . In: The time . August 1, 2016, ISSN 0044-2070 ( online [accessed August 2, 2016]).
- ↑ Deutschlandfunk: Anthrax in Siberia August 4, 2016; accessed on August 8, 2016
- ↑ TV Inglesby et al. a .: Anthrax as a Biological Weapon . In: Journal of the American Medical Association . tape 18 , no. 281 , 1999, p. 1735-1745 , PMID 10328075 .
- ↑ Till Winfried Bärnighausen: Medical human experiments of the Japanese troops for biological warfare in China, 1932-1945. Medical dissertation, Heidelberg 1998
- ↑ Erhard Geissler: Biological weapons - not in Hitler's arsenals: biological and toxin weapons in Germany from 1915 to 1945 . LIT Verlag, Münster, p. 341 ( limited preview in Google Book search).
- ↑ Domagoj Valjak: Operation Vegetarian: in 1942, the British planned on killing millions of Germans by dropping anthrax onto their pastures The Vintage News, January 10, 2018
- ^ Jonathan Glancey: Goodbye to Berlin. In: The Guardian . May 12, 2003, accessed November 27, 2017 .
- ↑ Mike Davies: Attack on "German Village" . In: Der Spiegel . No. 41 , 1999 ( online - 11 October 1999 ).
- ↑ M. Meselon , J. Guillemin, M. Hugh-Jones, A. Langmuir, I. Popova, A. Shelokov, O. Yampolskaya: The Sverdlovsk anthrax outbreak of 1979 . In: Science . tape 266 , no. 5188 , November 18, 1994, pp. 1202–1208 , doi : 10.1126 / science.7973702 , PMID 7973702 ( online (PDF)). The Sverdlovsk anthrax outbreak of 1979 ( Memento from May 2, 2015 on WebCite )
- ^ Former FBI Agent Sues, Claiming Retaliation Over Misgivings in Anthrax Case . New York Times, April 8, 2015.