Erythropoiesis
| Parent |
| Myelopoiesis |
| Gene Ontology |
|---|
| QuickGO |
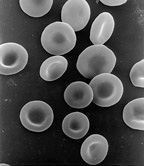
Erythropoiesis (also erythropoiesis , from ancient Greek ἐρυθρός (red) and ποίησις (education)) is the process of the formation and development of erythrocytes (red blood cells). It occurs before birth in the yolk sac , liver , spleen and bone marrow , after birth only in the red bone marrow of the flat and short bones. Erythropoiesis is stimulated by the hormone erythropoietin , which is formed in the kidney when there is a lack of oxygen in the tissue ( hypoxia ) . Disorders of erythropoiesis lead to anemia ( anemia ).
In the 10th week of embryonic development, the liver still accounts for 10% of body weight, at birth it is only half of this - a fact that is also attributed to the liver's function as a blood-forming organ.
Cell differentiation
All preliminary stages of the blood cells arise from mesenchymal cells , which can initially differentiate into all blood cells and are therefore referred to as multipotent stem cells . Once a development path has been taken, the cell loses its ability to enter other development paths; it is now referred to as a unipotent stem cell .
The unipotent stem cell of the erythrocytes is the so-called " erythropoietin responsive cell " (ERC). It develops into erythrocytes (normocytes) via proerythroblast, erythroblast, normoblast and reticulocyte. The development cycle in the bone marrow (up to the reticulocyte) lasts about five to nine days. Every day, around 200 billion (0.8% of the total) red blood cells are formed to replace outdated erythrocytes in humans .
Proerythroblast
Proerythroblasts (also: preerythroblast from Greek blastos "germ") are roundish, 18–22 µm large cells with a large, bright nucleus that contains two nucleoli and increasingly basophilic cytoplasm (which can be stained by basic dyes) . A proerythroblast leads to the formation of 16 erythrocytes through the cell division in the further differentiation. After the division of the pro-erythroblasts, basophilic erythroblasts first develop.
Erythroblast
The first stage of development are the basophilic erythroblasts . Their cell nuclei are relatively small and contain clumped chromatin . With a further reduction in nucleus size and a decrease in basophilia, polychromatic erythroblasts (also macroblasts ) now arise . These synthesize the red blood pigment hemoglobin on the polyribosomes and accumulate it in the cell, whereby the cytoplasm can increasingly be dyed for acidic pigments ( acidophil ) and finally the normoblast is formed.
Normoblast
Two cell forms are grouped as normoblasts , which have a relatively condense, round nucleus and a homogeneous, gray-pink looking cytoplasm in common. The immature cell, which is still capable of dividing, with a gray-bluish cytoplasm is now called polychromatic and the non-dividing, more hemoglobin-containing form with the cytoplasm already beginning to turn pink is called orthochromatic erythroblast . In this last form, the nucleus condenses into a small, black, structureless globule that is eventually expelled. The now nucleated young erythrocyte is rich in ribosomes , which can be precipitated into reticulate structures ( substantia reticulo-filamentosa ) by special staining, the reticulocyte.
Reticulocyte
Reticulocytes are youthful red blood cells and arise from normoblasts in the bone marrow one to two days after they are enucleated. In contrast to erythrocytes, they still contain RNA and cell organelle residues and are somewhat larger than those. These RNA residues are also known as the substantia granulofilamentosa . The reticulocytes owe their name to the staining of the ribonucleoprotein of the ribosomes, which is represented in the supravital staining or the staining with brilliant cresyl blue as a fine reticulate ( reticulum is the diminutive of rete "net") drawing in the cytoplasm.
Reticulocytes migrate from the bone marrow into the blood, where they mature into erythrocytes. Erythrocytes with a normal size, shape and color behavior are also referred to as normocytes .
A change in the number of reticulocytes in the peripheral blood (normally 3–18 ‰) can indicate increased or absent erythropoiesis, which is of practical importance for differentiating the forms of anemia .
regulation
The formation of new cells is regulated by an enzyme ( renal erythropoiesis factor , REF) that is released from the kidneys when the oxygen saturation in the blood is reduced . This enzyme breaks down the hormone-active erythropoietin ("Epo") from a protein in the blood plasma , which stimulates the division of the ERC.
If there is an increased need for erythrocytes, the formation in the bone marrow can be increased by eight to ten times normal production.
Disorders and diseases of the erythropoietic system
A disruption of the formation of erythrocytes (e.g. due to iron deficiency) can lead to anemia , as well as blood loss and hemolysis. An increase in red blood cells leads to polyglobulia or polycythemia . An increased demand for erythrocytes can occur through increased death of red blood cells ( haemolytic anemia , haemolysis ), through bleeding or, for example, when staying at higher altitudes with the associated lower oxygen partial pressure . The administration of erythropoietin also leads to an increase in hematocrit and is considered doping in sport . The number of reticulocytes can also be increased beyond the natural level by the administration of G-CSF .
Web links
- K. Wielckens: Clinical chemistry, pathobiochemistry and hematology. Erythropoiesis and its disorders. (PDF; 2.44 MB) Institute for Clinical Chemistry, University of Cologne Clinic.
Individual evidence
- ↑ Schmidt / Lang - Physiologie des Menschen, Springer-Verlag, 30th edition, p. 531.
- ↑ Ludwig Heilmeyer , Herbert Begemann: Blood and blood diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 376-449, here: pp. 395-419 ( The diseases of the erythropeotic system ).