neurology
The Neurology (from ancient Greek νεῦρον neuron , German , nerve ' and -logie , teaching') is the science and study of the nervous system , its diseases and their medical treatment. It has been an independent branch of medicine since the second half of the 19th century . The boundaries between psychiatry and neurosurgery are sometimes blurred.
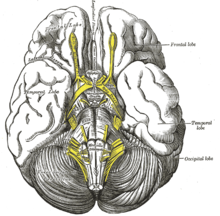
The most important organ systems in neurology are the central nervous system (i.e. the brain and spinal cord ), its surrounding structures and blood vessels . Then there is the peripheral nervous system and the muscles , including the connecting structures between the two. In Germany, neurology emerged as a branch of internal medicine around 1845 with Moritz Heinrich Romberg . In the USA, Great Britain, Russia and other countries, on the other hand, neurology had developed as an independent subject.
The neurological syndromes
A syndrome is a group of symptoms that occur simultaneously. There are about a dozen syndrome groups in neurology, and there are numerous syndromes in each syndrome group. Each syndrome has various neurological diseases, which are also structured completely differently from the syndromes. First of all, the different syndrome groups should be mentioned and briefly characterized.
- The syndromes of the peripheral nervous system subdivide the syndromes that affect disorders of the nerves in their course outside the spinal canal . These are lesions of peripheral nerves, the plexuses , nerve roots and the borderline , which are usually traumatic, as well as polyneuropathies .
- The term cerebral syndromes is used to summarize the four groups of local brain syndromes . These are the hemispheric syndromes , the brain stem syndromes , the extrapyramidal syndromes and the cerebellar syndromes . These syndrome groups can be further subdivided.
- Five different syndrome groups are summarized under the term spinal cord syndrome: the complete cross-sectional syndromes , the hemisphere syndrome of the spinal cord, the central spinal cord syndrome, the syndrome of the posterior cords and the anterior horn syndrome.
- There are five different neuro-ophthalmological syndromes : the olfactory groove syndrome, the sphenoid wing, the tip of the orbit, the Foster Kennedy syndrome and the cavernous sinus syndrome .
- The dizziness ( vertigo ) is divided in two ways: the vestibular and non-vestibular forms.
- There are three different neurootological syndromes : the pyramidal tip syndrome , the jugular foramen, and the cerebellopontine angle syndrome .
- There are two different groups of meningeal syndromes : the acute and the chronic meningeal syndromes.
- There are three different intracranial pressure syndromes: transfalxial, mesencephalic, and bulbar entrapment. It corresponds to the various forms of impaired consciousness in the section Neuropsychological Syndromes .
- There are five different types of headache that can be understood as syndrome groups: the vascular-related seizure-like headaches , the idiopathic seizure-like facial neuralgia (see also Atypical facial pain ), the diffuse permanent headache with an acute onset and the same with a gradual onset as well as the localized permanent headache.
- The four different CSF syndromes are a special group in neurological syndrome theory .
- The vertebral syndromes are differentiated according to their localization: cervical, thoracic and lumbar spine.
- Finally, there are five different groups of neuropsychological syndromes : the severe disturbances of consciousness , the aphasia , the apraxia , the agnosia and the amnesia .
The neurological diseases
The following disease groups are the subject of neurology and are treated and researched by it:
- Vascular diseases: these include in particular ischemic cerebral infarction and the various forms of cerebral hemorrhage .
- Basal ganglia diseases : this includes above all Parkinson's disease .
- Nerve injuries: all forms of nerve injuries are treated in cooperation with neurosurgeons and trauma surgeons.
- Neoplasms: tumors of the brain, spinal cord and peripheral nerves.
- Disc disease: all forms of mechanical nerve root irritation that do not require surgery or do not require surgery are treated by neurologists.
- Seizure disorders: this includes the treatment of epileptic and non-epileptic seizure disorders.
- Inflammatory diseases of the central nervous system: these include mainly bacterial and viral infections of brain and spinal cord tissue and membranes.
- Demyelinating diseases: this primarily includes multiple sclerosis .
- Primarily degenerative diseases: these include dementias , so-called motor neuron diseases ( amyotrophic lateral sclerosis , spinal muscular atrophies ) and degenerative cerebellar diseases (hereditary ataxias ).
- Dysraphic disorders (the so-called occlusive diseases ) and malformation diseases ( phacomatoses ).
- Peripheral nervous system disorders: e.g. B. Polyneuropathies .
- Muscle diseases: muscle dystrophies , myotonia and inflammatory muscle diseases, myositides .
- Neuromuscular transmission disorders: primarily myasthenia .
- Headache and facial pain: here especially the migraine .
Neurological examination techniques
Sophisticated diagnostic technology is still the domain of neurology today. The so-called neurological-topical diagnosis is considered ideal: the exact location of the damage in the nervous system should be indicated solely on the basis of the patient's report on his complaints (anamnesis) and a physical examination without technical aids . This requires precise questioning of the patient and his relatives, extensive experience in the clinical examination of patients and very precise theoretical knowledge of the theory of diseases and the structure and function of the nervous system. In this way, more than 90% of all relevant diagnoses in neurology can be made.
History taking in neurology
The peculiarities of taking anamnesis in neurology result from the nature of the neurological diseases. Some diseases started a long time ago so that patients have no precise memory of them. Then the patients often do not find the right words for the phenomena that interest the neurologist. For example, paralysis is sometimes confused with a sensory disorder, a coordination disorder is described as paralysis, and sometimes headache and facial pain are confused, etc. In such cases the doctor must structure the patient's medical history. This means that you have to have an idea of the symptoms that the patient could have and then ask exactly which disorder is present and the hypothesis formed, the description of the patient and your own opinion and the findings of the physical examination are brought into agreement. Since this is often not possible at the first interview, neurology needs time. It is worth asking patients again and again about their symptoms and calling in relatives in order to complete the picture of the patient's disorder.
Some anamneses can be fully structured. This includes, for example, questioning patients with headaches and seizure disorders. The neurological history of these diseases includes the following aspects in epilepsy : onset of the disease, occurrence of febrile convulsions in childhood, frequency of attacks per unit of time (week, month), daily attachment (occurrence at certain times of the day), triggering factors, the patient feels, if an attack occurs ( aura ), how long does the attack last, are the patients unconscious, if they bite the tongue (at the tip of the tongue or on the side of the tongue), if there is a faecal or wetting, the attack leads to falls in which the patient falls injure, there are special complaints after the attack (persistent confusion, speech disorder or similar), if witnesses have observed the attack, can they describe the motoric expressions, are the eyes open or closed during the attack, how do the patients fall, which medication What dose have been prescribed so far, have they effectively suppressed the seizures, have medication become the norm Taken moderately, were drug levels determined? For headache and facial pain, the survey is structured in a similar way, but special questions about the nature of the pain are added.
In conclusion, it should be said that taking anamnesis is always based on the patient's complaints and the suspected disease. A patient with the first manifestation of an inflammatory disease of the central nervous system is interviewed differently than a patient with Parkinson's disease . Sometimes someone else's medical history is the only information available in an emergency situation. Some patients cannot give any information about their illness (small children, animals in animal neurology). Such situations are always a special challenge.
The physical exam in neurology
A full clinical-neurological examination is time consuming. It requires patience and active cooperation from the patient.
Cranial nerve function : There are twelve pairs of cranial nerves . The function of each cranial nerve can be checked in a neurological examination. Since this is very time-consuming, cranial nerves are usually only examined for “orientation”. That is, you do an incomplete examination under the assumption that everything is probably all right. However, if a cranial nerve disorder is suspected, each individual function must be carefully checked in case of doubt. The first two cranial nerves are the olfactory nerve for the sense of smell and the optic nerve for the sense of sight. The smell is checked with odoriferous substances (e.g. with coffee powder) and the field of vision by means of what is known as finger perimetry . The cranial nerves III , IV and VI control the movements of the eyes (following the movement of a doctor's finger). The fifth cranial nerve is the trigeminal nerve . It takes care of the face in a sensitive manner and the masticatory muscles in terms of motor . The facial nerve is the seventh cranial nerve. It supplies the facial muscles with motor . The eighth cranial nerve is responsible for the organs of hearing and balance . This is where the tuning fork test comes into play. It makes sense to only test the sense of balance when it is disturbed. The patients then feel dizzy . For this purpose, there are special methods that can be used to provoke dizziness. The ninth cranial nerve is the glossopharyngeal nerve . It helps with swallowing and also conveys the taste in the back third of the tongue (there you taste bitter). The tenth cranial nerve is the vagus nerve , it mediates the vegetative parasympathetic innervation of the internal organs. It also supplies the auricle with sensors and the soft palate with motor . The eleventh cranial nerve controls part of the neck muscles and the twelfth cranial nerve ( hypoglossal nerve ) moves the tongue .
Motor skills : The motor skills are examined in various aspects. Various methods can be used to test the strength of each muscle group and, in some cases, that of many individual muscles. An example to explain the principle: The movement of the hand is made possible by three different nerves: the radial nerve , ulnar nerve and median nerve . The failure of one of the three nerves leads to characteristic changes: disorders of sensitivity, impairment of strength, long-term weakening of the muscles (muscle atrophy) and weakening of the respective reflexes . In the case of the median nerve (for example due to an injury to the elbow), the function of the nerve can be impaired. Since the medianus supplies the flexor muscles for the thumb, index and middle fingers, the patient's hand will not be able to develop full force when the fist is closed. It is not possible to open the screw cap of a bottle with the hand concerned. The muscles of the ball of the thumb recede over time.
Reflexes : A neurological examination can examine around ten so-called muscle stretching reflexes. At this point, only a single one of these reflexes will be briefly explained for explanation . The patellar tendon reflex is well known : a reflex hammer is used to lightly strike the tendon that leads below the kneecap to the front of the tibia . Provided the leg to be examined is positioned in such a way that the lower leg can swing freely, the triggering of the reflex will lead to the leg being stretched in the knee : The lower leg swings forward (this is the reflex response). The principle is that when you hit the tendon, the associated muscle ( quadriceps femoris muscle ) is briefly stretched. The nerves supplying the muscles emerge from the spinal canal in the lumbar spine (L3, 4). The reflex response is initiated via a reflex arc. If, due to a tissue change in the area of the nerve exit points of the corresponding lumbar vertebral bodies, parts of the intervertebral discs press on the nerve roots , this results in a functional impairment in addition to pain. The muscle is no longer properly innervated and thus weakens the extension of the leg. In addition, the reflex response is so impaired that it is weakened in comparison with the healthy side. The weakened reflex indicates the so-called “peripheral” paralysis. The location of the lesion is not in the central nervous system (brain or spinal cord), but in the peripheral nervous system, here in the area of the nerve root.
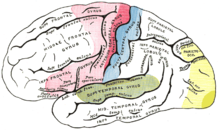
Sensitivity : There are four different sensitive qualities: tactile sensation and touch, pressure sensation, position of the extremities as well as pain and temperature sensation . The surface of the human body can be divided into defined areas based on sensitivity . This division of the surface of the body into sensitive areas ( dermatomes ) looks different, depending on whether a nerve root or a nerve is damaged in the further course. If the median nerve is damaged, you experience numbness in the area of the palm between the thumb and index finger (median supply area). When the intervertebral disc between the third and fourth lumbar vertebrae presses on the respective nerve root, one suffers a feeling of numbness in the corresponding supply area, which extends from the outside of the thigh to the inside of the lower leg.
Coordination : Disorders of the coordination of movements can have various causes. A dysfunction of the cerebellum can lead to what is known as ataxia . Such a movement disorder causes a movement sequence that overshoots the target. This can be checked, for example, by means of a pointing experiment (with your eyes closed, placing your index finger in a large arc on the tip of your nose). Even in the case of sensory disturbances, the movement sequence is impaired. Alcoholism and diabetes are common causes of sensitive neuropathy in which peripheral nerve function is impaired, especially in the lower extremities with a feeling of numbness. Since the patients do not feel the ground properly, they walk unsteadily and broad-based ( seaman's gait ).
Muscle tone : Some diseases ( multiple sclerosis , Parkinson's disease ) cause typical changes in the toning of the muscles. Limbs can usually be moved passively without resistance when patients relax. People with multiple sclerosis often have a spastic gait disorder (the gait looks lanky and awkward) and the increased muscle tone can be felt in the legs by flexing and straightening the patient's relaxed leg at the knee. You can feel a sudden increase in resistance during movement, which decreases when you reduce the force. The same applies to the so-called rigor of the muscles in Parkinson's disease. A sign characteristic of this disease in this context is the so-called gear wheel phenomenon .
Meningism : Neck stiffness is caused by irritation of the meninges and is particularly evident in the patient's posture. This is tested by means of various maneuvers that stretch the meninges slightly (e.g. bending the head forward). However, the examination is very painful for patients with meningitis.
Pyramidal trajectory sign : The pyramidal tract consists of a bundle of nerve cell processes that run continuously from the frontal lobe to the first switching points in the spinal cord. These cells act as a pacemaker for voluntary movements. The name pyramidal track comes from a structure in the brain stem (the pyramis ) through which the pyramidal track runs. If this nerve bundle is interrupted at any point, a typical functional failure occurs: spastic paralysis (reduced strength with increased muscle tone). The causes can be completely different: an injury to the spine and the spinal cord, a circulatory disorder in the brain stem, a cerebral haemorrhage in the area of the so-called capsule or a tumor in the cerebral cortex at the relevant point. In addition to paralysis and increased muscle tone, so-called pyramidal trajectories are often found. This means primarily the lifting ( dorsiflexion ) of the big toe when brushing the outer edge of the sole of the foot ( Babinski reflex ).
Further examination procedures: Special examinations are carried out for various diseases. So you can with certain methods welding - secretion check or adjustment of blood pressure and heart rate during exercise. After a stroke, one examines the motor functions of the language in the case of dysarthria or the grammatical functions of the language in the case of aphasia . Disturbances of complex movement sequences without impairing strength and sensation are called apraxias (an example would be putting on a jacket). Some patients do not notice their newly created deficit after a stroke ( anosognosia ). Sometimes after a stroke there is a visual field loss that patients do not notice. Failure to notice this disorder is called neglect . There are special investigation methods for these phenomena. Another special area is the neurological examination of impaired patients and young children.
In summary, it can be said that the examination methods that were briefly presented here and of which only an incomplete selection could be given, are irreplaceable for the detection of neurological diseases. No technical procedure can take the place of attentive observation and sensitive conversation, as well as the many different maneuvers and tests. The aim of all these measures is a diagnosis and thus the determination of which neurological disease is present.
Technical examination procedures in neurology
The technical examination procedures in neurology are very diverse.
A number of diseases can be diagnosed by examining biological material such as blood (laboratory values), nerve water ( liquor diagnostics ), tissue samples from nerves and muscles, as well as genetic analyzes.
Another group of examination methods is the measurement of electrical phenomena such as brain waves ( electroencephalography (EEG), evoked potentials ), muscle functions ( electromyography , EMG), the electrical functions of the nerves ( nerve conduction speed through electroneurography , ENG) and transcranial magnetic stimulation .
The vessels supplying the brain can be examined using ultrasound (extracranial and transcranial Doppler and duplex examinations) and invasive procedures (e.g. angiography ).
Imaging methods for displaying the brain and spinal cord are computed tomography (CT), magnetic resonance tomography (MRT) and the so-called functional imaging methods: positron emission tomography (PET), single photon emission computed tomography (SPECT), functional magnetic resonance tomography (fMRI) and magnetoencephalography (MEG ).
The clinical method and the clinical reality
The references to errors in the application of the clinical method should express the fact that in everyday clinical practice sometimes the clinical method is not used. Most textbook authors agree that engineering research should not replace clinical method. In addition, the implementation of technical examinations should fulfill the function of testing clinical hypotheses. In short, computed tomography is not intended to replace clinical diagnostics. Whenever these basic rules are violated during a diagnostic procedure, there is a high risk of making mistakes or being unable to make a diagnosis at all. Before the neurological diseases are outlined in a special chapter, the course of the clinical method in neurology must be supplemented by a further step. It is a question of formulating all the knowledge that has been gained so far in terms of syndromes. Specifically, this means: Do the data (anamnesis, findings and neurophysiological considerations) allow a patient's complaints to be assigned to one of the known neurological syndromes? This question is the last necessary step before a neurological diagnosis can be made and will be discussed in the next section.
Therapy principles of neurology
For many years, neurology was considered a discipline in which very complex diagnostic procedures were used, but only a few therapeutic options existed. This has changed fundamentally in the last few years: Many neurological diseases are much easier to treat today than they were a few decades ago. Critical to improving the care of stroke patients is z. B. the now routine diagnostic imaging that allows a distinction between ischemic cerebral infarction and cerebral hemorrhage. Various groups of drugs are now available for the treatment of Parkinson's disease.
When treating the seizure disorders, freedom from seizures can be achieved in many cases. The infectious-inflammatory diseases of the nervous system are almost all completely curable if diagnosed early. Multiple sclerosis is still incurable, but since the introduction of interferons , the course has become easier to influence. Treatment options are still very limited for most degenerative diseases of the nervous system, malformations and congenital muscle diseases .
The clinical method in neurology
The patient as a guide
Neurology textbooks emphasize the importance of the clinical examination of the patient. Exact questioning of the patient and the physical examination based on the symptoms are extremely important in neurology. In the course of this examination, the doctor forms hypotheses about the nature of the patient's illness. Here, he is guided by knowledge of the functioning of the nervous system ( neuroanatomy , neurophysiology ), knowledge of the various neurological diseases and his experience, the so-called clinical view of typical combinations of complaints and signs in certain diseases. On the basis of these hypotheses, he makes an assumption about which region of the nervous system could be damaged (damage location in the sense of a neurological-topical diagnosis). He then initiates a targeted investigation that should, if possible, confirm or refute the hypotheses formed about the location of the damage. The following case studies will illustrate this approach.
Case study I: normal pressure hydrocephalus
A 71 year old male patient is brought to the neurological consultation by the relatives. It was reported that the grandfather had fallen repeatedly recently but was not injured, that he had become forgetful and it was found that he had problems urinating. In response to specific inquiries, the relatives report that the complaints came over time and that the whole thing has dragged on for at least two years. Then the patient is physically examined. The neurologist asks the patient to walk through the room: he shows a clumsy gait pattern and raises his feet only a little while running. The working hypothesis is now: Dementia with bladder emptying disorder and so-called "magnetic" gait, which has existed for about two years and was accompanied by an increase in symptoms, could be caused by slowly developing hydrocephalus . First, a CCT of the skull is performed. Due to the suspected hydrocephalus, one expects so-called ballooned lateral ventricles with marginal and preferably frontal hypodensity . Since the CCT shows these findings, a therapeutic-diagnostic measure is carried out: in the so-called Fisher test , approx. 30 to 40 ml of nerve water is sampled using a lumbar puncture . This measure should improve the symptoms. The test does not show any increased CSF pressure. About 10 minutes after the lumbar puncture, the patient shows an improved gait pattern. His memory impairment will not be affected, and urinary incontinence is most likely to improve later. The patient is referred to the neurosurgeon with the diagnosis of normal pressure hydrocephalus for the implantation of a ventriculo-peritoneal shunt system for the purpose of permanent drainage of excess nerve fluid.
Case study II: brain tumor
A 32-year-old man is taken to a hospital emergency room after colleagues found the patient unconscious and lying on the floor with a head laceration. The occurrence of the presumed fall and whether there was jerks or the like was not observed. The patient himself lacks any memory. In a dazed state, he is first treated by a trauma surgeon in the polyclinic. The patient complains about a weakness of the right arm and explains that this is new. After the head wound has been treated, the patient is presented to the neurologist, who notices a drop in the arm hold attempt on the right. The neurologist now considers, among other things, that the patient could have suffered a fall as part of a generalized epileptic seizure , whereby the paresis could also be interpreted as so-called Todd's palsy . The CCT examination carried out shows a left, highly parietal, round hypodensity . After a neurological-internal investigation of the vascular risk factors had shown negative results and suspicious structures had been seen in the MRI , a brain biopsy was carried out to confirm the suspected diagnosis of a brain tumor , by means of which the diagnosis of an astrocytoma can be made.
Case study III: brain stem infarction

A 62-year-old woman is taken to the emergency room with a sudden unsteady gait. She also complains of a new "hoarseness". The patient is diabetic and has high blood pressure . She reports that she had injected her insulin almost exactly an hour ago, took her blood pressure medication, and after that it was strange to her and she fell when getting up. Her family members immediately took her to the emergency room. A gait test shows that the patient can only stand with help, although her leg strength is unimpaired. The inspection shows that her right upper eyelid is drooping slightly. When the neurologist holds up a mirror to her, she realizes that her right eye is “crooked”. The examination shows that the temperature sensation in the area of the left arm has disappeared. A CCT of the brain skull shows no noticeable changes. With a Doppler sonography of the extracranial vessels supplying the brain, the right vertebral artery cannot be shown. The suspected diagnosis is Wallenberg syndrome as a result of a cerebral infarction of the dorsolateral medulla oblongata in the supply area of the right inferior cerebellar artery due to an occlusion of the right vertebral artery.
Case IV: Meningitis

A 24 year old man is taken to the hospital emergency room. The patient's father reports that his son is a regular soldier and is at home on vacation. At noon on the day of admission, he complained that he was doing badly. He began to complain of increasingly severe headaches and to freeze. Since he no longer reacts properly to being spoken to, he is taken to the nearby hospital. The young man looks seriously ill, he cannot stand and only answers questions with difficulty and is trembling badly. A rectal temperature reading gives 39.4 ° C. The neurologist conducts a physical examination: he grips the patient's head with both hands and slowly moves it to the right and left. This movement alone causes significant pain for the patient, who is lying in bed with his legs drawn up and his head slightly bent backwards. Based on these findings: fever , headache , decreased consciousness , neck stiffness and history (the patient is a soldier) is a tentative diagnosis of meningococcal - Meningitis provided and arranged appropriate hygienic measures for the personnel. If meningitis is suspected, intravenous antibiotics are started immediately . After the exclusion of intracranial pressure, preferably by showing a free cisterna ambiens by means of native CCT, alternatively by looking at the fundus, a lumbar puncture is performed to confirm the diagnosis and optimize the therapy.
The step-by-step approach to diagnosis in neurology
The examples show the different stages in the neurological approach to clinical issues.
First step: medical history, clinical symptoms, clinical signs, technical findings
When taking anamnesis, the time dimension is important (see also the course of the disease ):
- Peracute during a seizure , the patient falls from full health.
- Acute in ischemic (due to reduced blood flow) cerebral infarction, within a few minutes the unsteady gait and hoarseness set in.
- Subacute meningitis, an extremely severe clinical picture develops within hours.
- Chronic with normal pressure hydrocephalus, the symptoms develop gradually over months or years.
If a first hypothesis has been made based on the anamnesis, one makes sure of some details again:
- The patient with the head laceration is too young to have an ischemic cerebral infarction.
- The elderly woman unable to stand has vascular risk factors.
- The feverish young man with severe headache is a soldier (meningococci can be found in nasopharyngeal swabs in 20% of all soldiers).
Then specific physical examinations are carried out:
- The attempt to hold the arm on the young man with the seizure.
- The testing of temperature sensitivity in the old woman with incapacity to stand, hoarseness and crooked eye (you simply hold the metal handle of the reflex hammer under the cold water of the sink and give it to the patient first in the left and then in the right hand, the patients notice this immediately Difference).
- The very careful turning of the head in the meningitis patient.
- The old man's gait test: "Please go through the room."
Further investigations:
- The CCT finding in the young man is ambiguous only on the surface: a round hypodensity always suggests a tumor. In this case, it is irritating that the patient said that the arm paralysis came suddenly.
- The inconspicuous CCT finding is unusual in that, given the risk factors present, asymptomatic older lesions are often found in various parts of the brain. However, the current lesion suspected in the area of the brain stem is usually not visible in the CCT.
- In the case of the young man with meningitis, a CSF culture is absolutely necessary to detect the pathogen. The decision about diagnosis and therapy, however, is made without any technical diagnosis (apart from fever measurements).
- The CCT finding in the old man with the "magnetic" walk is good support for the initial hypothesis, but too unspecific.
This systematic approach facilitates a neurological examination.
Second step: Interpretation of the data obtained in physiological and anatomical terms
The young man with the head laceration has arm paralysis. The reflex test can be used to determine whether the paralysis is central or peripheral: If the muscle stretching reflexes in the right arm are weakened, this indicates damage to the nerves outside the spinal canal (peripheral lesion). If the reflexes are stressed, this indicates damage to the spinal cord or brain (central lesion).
The old lady with the speech disorder has so-called “crossed” symptoms: the drooping upper eyelid on the right (a Horner syndrome ) and the temperature sensitivity disorder on the left . A “crossed” symptomatology is typical of the brain stem due to anatomical conditions. The posterior small cerebellar artery is often affected.
The aim of the feverish young man is his hunched posture when lying down, which is typical for irritation of the meninges and spinal cords . If the patient also has a fever, it is obvious that the irritation of the meninges has an infectious (mostly bacterial) cause. The fact that the young man is a soldier supports the suspicion that meningococcal meningitis is present.
Third step: Syndromal formulation and anatomical diagnosis
An isolated central arm paralysis in the young man with the head laceration is rather unusual. Probably the neurologist did not examine the patient carefully and overlooked the discrete, centrally caused paralysis of the facial muscles (see facial paralysis ) on the right and possibly a slight aphasic disorder. But it is crucial that you get to your destination quickly and safely. The combination of a first-time seizure in a 30-year-old man and the described CCT finding is highly suspicious of an astrocytoma.
The old lady with the brainstem infarction is a prime example of so-called topical diagnostics in neurology. The combination of a Horner's syndrome with a contralateral disturbance of temperature sensitivity always points to the brain stem and there in the area of the medulla oblongata. In order to understand the disorder, it is crucial that in the area of the brain stem, on the one hand, the core areas of the cranial nerves and, on the other hand, pathways for motor skills and sensitivity . The close proximity of these structures at this point in the brain leads to disturbances in distant parts of the body that are supplied by these structures.
The feverish young man has no lesion in a particular point in the nervous system, he has a disorder in an entire organ system, namely the entire meninges. This also determines the severity of the disease and the great risk of numerous complications such as generalized seizures, coma and respiratory paralysis .
Fourth step: pathological or etiological diagnosis
The neurologist does not actually make a definitive diagnosis on the young man with the head laceration. The final (pathological or etiological) diagnosis is made in this case by the pathologist on the basis of a brain biopsy. The neurologist's job is to pave the way for that.
The etiological diagnosis in the case of the elderly woman is presumably an embolic occlusion of a cerebral artery due to arteriosclerotic changes in the upstream circulation leading to an ischemic infarction of the brain area originally supplied by the vessel. A so-called border zone infarction would also be possible due to a lumen reduction ( stenosis ) of the upstream vessels caused by arteriosclerosis .
The released by the infection and the immune reaction of the body bacteria - toxins are lead in the case of meningitis the reason for the dramatic course of the disease, if untreated with very high probability to death.
Summary of all steps: the clinical method in a nutshell
History : A man presents himself to the emergency room and explains that for about an hour he has had the feeling that something is wrong with his face. The man is 65 years old, he is a smoker and has high blood pressure.
Physical examination : the neurologist asks him to close both eyes tightly and "show his teeth". The eyelid closure is complete on both sides, but the grimacing of the mouth is only possible on the right side.
Transformation of the findings into neurophysiological terms : This finding suggests a central left facial paresis.
Syndromal formulation in the sense of a neurological topical diagnosis : The localization of the disturbed brain region can be narrowed down further if the neurologist has the patient hold both arms in front of him with his eyes closed: the left arm shows an inward rotation. Both legs are normal in the neurological examination. The neurologist suspects the location of the lesion in the right cerebral hemisphere in the so-called precentral region .
Etiological diagnosis : As the patient has vascular risk factors (age, smoking, hypertension), a circulatory disorder in the supply area of the right cerebral artery is suspected. This assumption can be confirmed or refuted by means of imaging examinations of the brain and, above all, a vascular representation.
The treatment is then carried out according to the therapy guidelines for cerebral infarction patients.
Summary of the diagnosis
The clinical method in neurology can be described as follows: Data is collected by asking the patient or his relatives about the previous history as well as through a physical examination. These data are interpreted on the basis of physiological and anatomical knowledge and a hypothesis is formulated (anatomical diagnosis). Specific technical investigations are then carried out to confirm or refute the hypothesis. This leads to a final pathological or etiological diagnosis, which usually also has a precisely defined name. Therapy is then agreed with the patient on the basis of verified empirical values from clinical studies .
In older neurology textbooks one can occasionally find simple mnemonics about this main principle of neurology such as "The principle of the six Ws" according to Mumenthaler :
- W he did the disease? (Anamnese)
- W as it is found? (Finding)
- W o sits the lesion, which can cause such symptoms? (topical diagnosis)
- W hy ill patient? (etiological diagnosis)
- W OH in the disease process leads? (Forecast)
- W omit treated you? (Therapy)
The question of where , the so-called topical diagnosis, is specific to neurology . Although this principle also plays a role in the diagnosis of myocardial infarction, for example, it is a defining feature for all of neurology. This fact is explained using further selected (constructed) case studies in which errors in the clinical method are shown.
Error in the application of the clinical method
The main mistake in applying the clinical method is not applying it consistently. Beginners in particular, but also experienced doctors, tend to carry out technical examinations in cases in which they do not know what to do or are unsure, in the hope of being able to bring about a diagnostic clarification. It is not uncommon for this approach to be misleading or costly in terms of time and money, and sometimes it even hinders the establishment of a correct diagnosis. In order to make this clear, some (partly abbreviated and constructed) case studies are given in which the doctors concerned did not consistently apply the clinical method.
Case study V: A child with a seizure status
A ten year old child is taken to a hospital emergency room in a dazed state with a head laceration. The cause of the fall is initially unclear. While in the emergency room, the child had a seizure. Since this does not subside, the patient is emergency intubated and ventilated and the seizure status is interrupted by anesthesia. The neurologist consulted suspects encephalitis . A CCT and a CSF examination do not give any conclusive findings. The child is initially further ventilated in an intensive care unit. If you try to reduce the depth of anesthesia, seizures occur again.
Another neurologist is consulted to clarify the situation. This first takes a detailed anamnesis. The suspected diagnosis is "encephalitis" and the task is to find a possible pathogen. The relatives provide the following information: there was no trip abroad, the child has a cat as a pet and a sibling died as a result of an HIV disease. The general physical examination revealed the following: axillary lymph node swelling on the right and bilateral conjunctivitis . This constellation of findings allows the following suspected diagnosis: Encephalitis caused by the causative agent of the cat's scratch disease ( Bartonella henselae ). This assumption was confirmed by serological examinations of the CSF and the detection of encephalitic foci in the putamen by means of magnetic resonance imaging . Therapy consists of the administration of macrolide antibiotics , co- trimoxazole or rimfampizine . The child recovers and the disease heals without any consequences.
The mistake was that no detailed anamnesis was taken in the acute situation or later. In this case, only the anamnesis and the non-neurological examination findings provide clues that lead to the pathogen and the diagnosis of Bartonella encephalitis (cat as a pet, axillary or cervical lymph node swelling). The noticeable bilateral conjunctivitis is a side effect of this rare encephalitis (only a few dozen cases have been described worldwide).
Case VI: A young man with a cerebral infarction
A man about 35 years old is admitted to the clinic with signs of an acute ischemic cerebral infarction. According to information from work colleagues, he fell, then suddenly complained of malaise and spoke indistinctly. In the admission situation, the patient shows arm and facial paralysis on the right, he is dazed and aphasic. The event is less than 45 minutes old. At this stage, a CCT examination does not show any early signs of a cerebral infarction, but is carried out to rule out cerebral hemorrhage. A Doppler and duplex sonographic examination of the neck vessels shows evidence of an occlusion of the internal carotid artery (ACI) on the left. The diagnosis is: occlusion of the ACI on the left with ischemic cerebral infarction in the medial flow area on the left. There is a thrombolytic therapy initiated. Paralysis and language disorders recede completely. Doppler sonography shows a high degree of flow obstruction of the ACI on the left. However, the patient has no vascular risk factors. For this reason, the anamnesis is checked again. The patient reports that he fell shortly before the event and, very unhappily, fell against the edge of the table with the left side of his neck. The suspected diagnosis of a dissection of the internal carotid artery is confirmed by magnetic resonance imaging of the cervical vessels.
The mistake was not to have asked the patient's companion in detail about the circumstances of the fall.
Special features of animal neurology
Neurology is also a major challenge for veterinarians because, in addition to the great complexity of the nervous system, it is also burdened with additional handicaps. On the one hand, in contrast to the human neurologist, he is only in the rarest of cases a specialist who “only” has to treat neurological cases.
Another problem is the wide range of species. Findings from human medicine can only be transferred for a few diseases, since other mammals , birds or even reptiles have significant neuroanatomical and functional differences and the clinical picture of a certain neurological disease can vary considerably depending on the species . Even a severe stroke with complete failure of the supply area of the arteria cerebri media , which causes complete hemiplegia in humans, only leads to mild disturbances of the postural reflexes in a sheep, but hardly to impairment of the gait pattern. The most noticeable is torticollis , but it can also have many other causes. This is due to the differences in the intersection of the pyramidal trajectory and the very different importance of the pyramidal and extrapyramidal systems for the movement patterns.
The neuroanatomical diversity is also responsible for the fact that many neurological diseases in animals have not been adequately researched. Animal neurology is a relatively young science, with only a few proven specialists and small budgets, which can at best research more intensively the most important diseases and only in the most widespread representatives of domestic animals (especially horses and dogs ). In the case of exotic animal species, the veterinarian must always extrapolate from known species.
Another problem is limited communication. In human neurology, intensive questioning of the patient, the anamnesis, is an important element of diagnosis. Of course, an animal can tell the vet very little, and questioning before and during the diagnosis is not possible. The veterinarian is dependent on the animal owner's ability to observe, and is sometimes exposed to his imagination. The animal can make expressions of pain, but these already vary greatly not only between species, but also individually. An animal with a certain illness can stoically endure possible pain, especially when the treatment room is stressed, while another, actually healthy animal can react over-sensitive or aggressively to certain manipulations. Important diagnostic criteria such as two-point discrimination , i.e. the ability to localize the origin of a pain stimulus, cannot be ascertained in animals. The animal can express pain, but cannot tell the veterinarian whether it is feeling the second pain in the same or a neighboring area.
After all, veterinary medicine is much more cost-oriented than human medicine. In the case of farm animals, complex diagnostics or treatments are usually ruled out from the start. But even with pets, the medical effort must always be tolerated by the owner and also be financially supported. Cost-intensive large devices such as CT or MRT are only available in very few large animal clinics. And even an elaborately secured diagnosis does not necessarily have to lead to (affordable) therapy (if it is possible at all), which is ultimately unsatisfactory for both parties, owner and veterinarian.
Disease groups
The neurological diseases of pets are usually divided into eight disease groups, which can be remembered with the acronym VETAMIN D based on veterinary and vitamin D :
- V askular diseases ( Latin vas ' blood vessel ' ): All vascular diseases such as malformations , bleeding or ischemia are classified in this group . Vascular diseases are relatively rare in animals, only infarcts of the spinal cord are somewhat more common.
- E ntzündungen: In this group include viral (eg. Rabies ), bacteria (eg. Listeriosis ), mycotic , parasitic or immunopathologically induced inflammation of the nervous system.
- T raumatische diseases: Here all diseases are classified by mechanical causes (eg, by traumatic bleeding.) A direct or indirect damage cause.
- A nomalien: anomalies are congenital malformations that are either genetic or due to infections during the prenatal can be caused development.
- M etabolisch-toxic diseases: In this group include all disorders characterized by lack of nutrients, vitamins and trace elements or by endogenous toxins (eg. Urea ) are caused.
- I diopathic diseases: Idiopathic (without recognizable cause) diseases show no recognizable morphological changes in the nervous system, but only functional disorders such as e.g. B. epilepsy .
- N eoplasias: New formations ( neoplasia ), i.e. all tumor diseases, are classified in this complex . These can be tumors of the nerve cells, although glial cell tumors ( gliomas ) occur almost without exception in animals . A second group are tumors that originate from mesenchymal tissues, such as meningiomas .
- D egenerative diseases: Degenerative diseases are characterized by pathological deposition of materials (eg. Amyloidosis , by the death of specific neuronal populations, or by demyelination of nerve pathways () leukodystrophy in) and are mostly due to hereditary.
Historical aspects
Neurology as we know it today is very closely linked to developments in anatomy and histology . Only since regular autopsies have taken place and, above all, through the development of the microscope , has structures and their relationships been clarified.
The first indications of "neurological" treatment attempts are obtained from archaeological finds. The oldest documented trephination as a neurosurgical intervention was around 10,000 BC. Performed. The opening of the skull is one of the few tangible treatment methods, as the changes in the bone can still be detected even after thousands of years. Several hundred skulls opened in this way have been found worldwide. Most of these interventions were survived by the patients, which can be demonstrated by the regeneration processes of the bone. The technology of the time was so sophisticated that the dura mater was not normally opened, an essential requirement for survival. One can only speculate about the reasons for such interventions, assuming neurological symptoms such as severe headaches , epileptic seizures or ritual acts.
The first documents describing neurological symptoms come from the Mesopotamia between the Euphrates and Tigris and from Egypt, where around the 14th century BC. Headaches, epilepsies and dizziness were described. The first anatomical descriptions of the brain and surrounding structures can also be found. Furthermore, accident-related neurological symptoms such as paralysis or bleeding from the nose and ear in skull fractures are mentioned. There are also various pictorial representations of various neurological diseases.
Antiquity
Pythagoras and Anaxagoras first described the brain as the seat of the faculty of thought, sensations and the soul, as well as the connection between the brain and nerves . In contrast to these traditions, no corresponding written statements are known from Hippocrates .
The Greek word for nerve is neuron and denotes (as a (tensioned) string-like structure ) both tendons and nerves. An anatomical distinction was made as early as the 3rd century BC. The Latin word nervus remained a synonym for tendon until the late Middle Ages .
Modern times
Guillaume-Benjamin Duchenne and Jean-Martin Charcot are considered the founders of modern neurology .
See also
Literature and Sources
Human medicine
General textbooks
- Peter Berlit: Clinical Neurology . Springer, Berlin Heidelberg 2011, ISBN 978-3-642-16919-9 .
- Allan H. Ropper, Martin A. Samuels: Adams and Victor's Principles of Neurology. McGraw Hill, New York 2009, ISBN 978-0-07-149992-7 .
- Walter Gehlen, Heinz-Walter Delank: Neurology. Founded by Heinz-Walter Delank. Thieme, Stuttgart (1978; several new editions, e.g.) 2010, ISBN 978-3-13-129772-3 .
- Lewis P. Rowland, Timothy A. Pedley (Eds.): Merritt's Neurology. Lippincott Williams & Wilkins, 2009, ISBN 978-0-7817-9186-1 .
- Marco Mummenthaler , Heinrich Mattle: Neurology. New edition Thieme, Stuttgart 2008, ISBN 978-3-13-380012-9 .
- Heinrich Mattle, Marco Mumenthaler: Short textbook neurology. Thieme, Stuttgart 2010, ISBN 978-3-13-142933-9 .
- Karl F. Masuhr, Marianne Neumann: Neurology. Thieme, Stuttgart 2007, ISBN 978-3-13-135946-9 .
- Werner Hacke: Neurology. Springer, Heidelberg 2010, ISBN 978-3-642-12381-8 .
Child neurology
- Bruce O. Berg (Ed.): Principles of Child Neurology. McGraw Hill, New York 1996, ISBN 0-07-005193-3 .
Neurological differential diagnosis
- Peter Duus: Neurological-topical diagnostics. Thieme, Stuttgart 2003, ISBN 3-13-535808-9 .
- John Patten: Neurological Differential Diagnosis. Springer, Berlin 1996, ISBN 3-540-19937-3 .
Clinical neuroanatomy
- Detlev Drenckhahn, Wolfgang Zenker (Ed.): Kidney, reproductive organs, endocrine glands, nervous system, sensory organs, skin. Urban and Schwarzenberg, Munich 1994, ISBN 3-541-00255-7 (Benninghoff: Anatomie, Vol. 2)
- Lennart Heimer : The Human Brain. Functional Neuroanatomy and Dissection Guide. Springer, New York 1995, ISBN 0-387-94227-0 .
- Werner Kahle: Pocket Atlas of Anatomy. Vol. 3: Nervous system and sense organs. Thieme, Stuttgart 1976, ISBN 3-13-492203-7 .
- Stephen G. Waxman: Correlative Neuroanatomy. Appelton & Lange, New Haven 1995, ISBN 0-8385-1506-1 .
Neurobiology and neurogenetics
- Thomas Herdegen (Ed.): Clinical Neurobiology. Molecular pathogenesis and therapy of neurobiological diseases. Spectrum, Heidelberg 1997, ISBN 3-8274-0069-4 .
- Olaf Rieß (Ed.): Neurogenetics. Molecular biological diagnosis of neurological diseases. Springer, Berlin 1998, ISBN 3-540-63874-1 .
CSF diagnostics
- Robert A. Fishman: Cerebrospinal Fluid in Diseases of the Nervous System. Saunders, Philadelphia 1992, ISBN 0-7216-3557-1 .
- Uwe K. Zettl, Reinhard Lehmitz, Eilhard Mix: Clinical liquor diagnostics. Gruyter, 2005, ISBN 978-3-11-018169-2 .
Electrodiagnostics
- Mitsuru Ebe, Isako Homma: Guide to EEG Practice. An image compendium. Fischer, Stuttgart 1994, ISBN 3-437-00772-6 .
- Hanns C. Hopf u. a .: Electromyography Atlas. Thieme, Stuttgart 1996, ISBN 3-13-102221-3 .
- Borries Kukowski: Electrodiagnostics of peripheral nerve lesions. Thieme, Stuttgart 1995, ISBN 3-13-100271-9 .
- Bernhard Neundörfer: EEG primer. The EEG in the medical practice. Gustav Fischer, Stuttgart 1995, ISBN 3-437-00807-2 .
- Manfred Stöhr, Manfred Bluthardt: Atlas of clinical electromyography and neurography. Kohlhammer, Stuttgart 1987, ISBN 3-17-009563-3 .
- Manfred Stöhr, Johannes Dichgans, Ulrich W. Büttner: Evoked Potentials. Springer, Berlin 2005, ISBN 978-3-540-01773-8 .
- Stephan Zschocke, Hans-Christian Hansen: Clinical encephalography. Springer, Berlin / Heidelberg 2012, ISBN 978-3-642-19942-4 .
Cerebral infarction and vascular diagnostics
- Christian Arning: Color-coded duplex sonography of the arteries supplying the brain. Thieme, Stuttgart 1996, ISBN 3-13-102131-4 .
- Ulrich Bogdahn u. a .: Echo signal amplifiers and transcranial color duplex sonography. Blackwell, Berlin 1998, ISBN 3-89412-324-9 .
- Hans Joachim von Büdingen, Gerhard-Michael von Reutern: Ultrasound diagnosis of the arteries supplying the brain. Thieme, Stuttgart 1993, ISBN 3-13-731402-X .
- Marc Fisher (Ed.): Cerebrovascular Disorders. Wolfe, London 1994, ISBN 1-56375-091-0 .
- Bernhard Widder: Doppler and duplex sonography of the arteries supplying the brain. Springer, Berlin 1985, ISBN 3-540-58731-4 .
Imaging procedures
- Mauricio Castillo: Neuroradiology Companion. Methods, Guidelines and Imaging Fundamentals. Lippincott-Raven, Philadelphia 1999, ISBN 0-7817-1695-0 .
- Torsten B. Möller, Emil Reif: Head, neck, spine, joints. Thieme, Stuttgart 1997, ISBN 3-13-799202-8 . (Pocket Atlas of Sectional Anatomy, Vol. 1)
- Radü, Ernst Wilhelm u. a .: Computed tomography of the head. Thieme, Stuttgart 1994, ISBN 3-13-582603-1 .
- Detlev Uhlenbrock: MRI and MRA of the head. Thieme, Stuttgart 1996, ISBN 3-13-103531-5 .
Neuropsychology
- Stephan Ahrens u. a .: Psychosomatics in neurology. Schattauer, Stuttgart 1995, ISBN 3-7945-1593-5 .
- Siegfried Gauggel, Georg Kerkhoff (ed.): Case book of clinical neuropsychology. Hogrefe, Göttingen 1997, ISBN 3-8017-0793-8 .
- Robert E. Hales, Stuart C. Yudofsky (Ed.): Handbuch der Neuropsychiatrie. Psychologie-Verlags-Union, Weinheim 1993, ISBN 3-621-27123-6 .
- Wolfgang Hartje, Klaus Poeck : Clinical Neuropsychology. Thieme, Stuttgart 1997, ISBN 3-13-624503-2 .
Neurological rehabilitation
- Peter Frommelt, Holger Grötzbach (Ed.): Neuro-Rehabilitation. Blackwell, Berlin 1999, ISBN 3-89412-321-4 .
Individual illnesses
- Marco Mumenthaler, Hans Schliack: Lesions of peripheral nerves. Thieme, Stuttgart 1965, ISBN 3-13-380205-4 .
- G. Bartolome (Ed.): Swallowing disorders. Diagnostics and rehabilitation. Fischer, Munich 1999, ISBN 3-437-21320-2 .
Neurological therapy
- Johannes Jörg (Ed.): Neurological Therapy. Springer, Berlin 1997, ISBN 3-540-60066-3 .
- Thomas Brandt, Johannes Dichgans, Hans-Christoph Diener (eds.): Therapy and course of neurological diseases. 5th edition. Kohlhammer, Stuttgart 2007, ISBN 978-3-17-019074-0 .
- Richard MA Suchewirth: Neurological examination. Neuromedizin Verlag, Bad Hersfeld 2009, ISBN 978-3-930926-11-4 .
Veterinary medicine
- André Jaggy: Atlas and textbook of small animal neurology. Schlütersche, Hannover 2005, ISBN 3-87706-739-5 .
History of neurology
- Klaus-Joachim Zülch : The historical development of German neurology. Berlin / Heidelberg / New York / London / Paris / Tokyo 1987.
- Klaus-Joachim Zülch: Neurology in America. In: German Medical Weekly . Volume 80, 1955, pp. 1311-1314.
- Axel Karenberg : Neurology. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 1037-1044.
- Kurt Kolle (Ed.): Great neurologists. 3 volumes. Stuttgart: Thieme 1956–1963; 2nd edition there 1970.
Web links
- German Society for Neurology - Latest version of the guidelines
- Guideline Clinical Nutrition in Neurology of the AWMF
- European Federation of Neurological Societies
- American Academy of Neurology
- National Institute of Neurological Disorders and Stroke
Individual evidence
- ↑ Johannes Pantel: Neurology, Psychiatry and Internal Medicine. Course and dynamics of a historical dispute . In: Würzburg medical history reports . tape 11 , 1993, p. 77–99 , here: p. 77 .
- ^ Axel Karenberg: Neurology. In: Werner E. Gerabek u. a. (Ed.): Encyclopedia of medical history. 2005, pp. 1037-1044; here: p. 1038.
- ^ Friedrich Kluge , Alfred Götze : Etymological dictionary of the German language . 20th ed., Ed. by Walther Mitzka , De Gruyter, Berlin / New York 1967; Reprint (“21st unchanged edition”) ibid 1975, ISBN 3-11-005709-3 , p. 507.
- ^ Franz Dornseiff : The Greek words in German. Berlin 1950, p. 53.
- ↑ Hieronymus Brunschwig : The book of the Cirurgia. Strasbourg (Johann Grüninger) 1497; Reprints Munich 1911 and Milan 1923, p. 262.
- ↑ See Jean Bogousslavsky (Ed.): Following Charcot. A Forgotten History of Neurology and Psychiatry. Basel 2011.