Atherosclerosis
| Classification according to ICD-10 | |
|---|---|
| I70.- | Atherosclerosis |
| ICD-10 online (WHO version 2019) | |
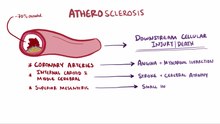
Atherosclerosis (imprecisely also arteriosclerosis ) describes the pathological storage of cholesterol esters and other fats in the inner wall of arterial blood vessels . Atherosclerosis occurs primarily in the coronary arteries , the junction of the carotid artery and the large arteries of the leg. It is a chronic inflammatory process: fatty streaks can already be detected in the vessels of young people, which slowly develop into atherosclerotic plaques in which a fat core is covered by a more or less stable layer of connective tissue .
Atherosclerotic plaques can constrict vessels so much that the oxygen supply to the affected organ is impaired, which can manifest itself in the affected person as tight chest (heart) or intermittent claudication (leg). When atherosclerotic plaques tear, blood clots form that can completely obstruct the vessel , resulting in medical emergencies such as heart attacks and strokes . Atherosclerosis is a disease of civilization and is now the most common cause of death worldwide.
In colloquial terms, hardening of the arteries is often referred to , but there is no deposit on the surface of the inner wall of the vessel, nor is it chemically any form of calcium . Atherosclerotic plaques, however, often contain other calcium salts (e.g. calcium phosphate ) that harden the vessel.
Demarcation
Atherosclerosis is a form of hardening of the arteries ( arteriosclerosis , from ancient Greek ἀρτηρία artería , German 'vein' and σκληρός sklerós , German 'hard' ). Arteriosclerosis is often used synonymously in German with atherosclerosis, but strictly speaking also includes Mönckeberg sclerosis , in which the middle vascular layer hardens due to the storage of calcium salts, as well as arteriolosclerosis , which pathologists use to describe the storage of hyaline substance in the arterioles of certain organs. Within the vascular diseases ( angiopathies ), atherosclerosis is one of the macroangiopathies because it affects arteries, i.e. larger vessels; Disturbances of the microcirculation such as diabetic microangiopathy are to be distinguished from this .
pathology

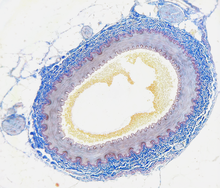
The disease is characterized by a chronically progressive degeneration of the arterial walls . Connective tissue overgrowth, intra- and extracellular deposits of cholesterol , fatty acids and calcium phosphate as well as the accumulation of collagen and proteoglycans lead to hardening and thickening of the vessel walls, which are accompanied by a decrease in the elasticity of the vessel walls and i. d. Usually also lead to narrowing of the vessel volume. The mineral deposits that occur are carbonate-containing hydroxylapatite , which is chemically very similar to the calcium phosphate phase of the bone.
Pathogenesis
The pathogenesis of atherosclerosis is the subject of ongoing research and is not fully understood. With the help of the ever more detailed understanding of the biochemical processes in and between cells and on the basis of (numerous) histological findings , attempts are made to clarify the causes and the biochemical process.
Regarding the elucidation of the mechanisms that lead to the initiation of arteriosclerosis, two central hypotheses have emerged in the last decades of broad arteriosclerosis research: the “Response to injury hypothesis” and the “Lipoprotein-induced atherosclerosis hypothesis”.
initiation
The response-to-injury hypothesis
According to the response to injury hypothesis put forward by the American atherosclerosis researcher Russell Ross in 1976 , an injury to the inner arterial wall layer initiates arteriosclerotic events. The inner layer of the artery wall, the intima , consists of a single-cell layer of endothelial cells and the subendothelial connective tissue. In his work Ross lists several causes for the injuries to the endothelial cell layer. This includes morphological damage due to trauma , for example due to high blood pressure or mechanical injuries, biochemical damage due to bacterial toxins , attack by viruses or antigen-antibody reactions as well as biophysical injuries at the molecular level. As a result of violation of the endothelial cell layer, two observed phenomena typical for the emergence of this disease: on the one hand by growth factors or cytokines induced growth ( proliferation ) and migration (migration) of smooth muscle cells from the multi-layered media into the intima, and on the other Formation of foam cells in the intima and media caused by fat storage . Over a longer period of time, these two phenomena lead to the formation of focal tissue changes (plaques), which are characteristic of the picture of arteriosclerosis. In recent years, an increased rate of apoptosis has increasingly become the focus of research interest.
The "response-to-injury" hypothesis presupposes a specific injury that naturally occurs for a limited time. A modified approach speaks of endothelial dysfunction as the cause of the triggering of arteriosclerosis, which means any malfunction of the endothelium that promotes the development of arteriosclerosis. Whether the malfunction is caused by a singular injury or by a gradually occurring imbalance of endothelial functions is irrelevant.
The lipoprotein-induced atherosclerosis hypothesis
The American researcher and Nobel Prize winner Joseph Leonard Goldstein was the first to report on the rapid uptake of chemically modified LDL by macrophages and the subsequent conversion to foam cells. The chemical modification consisted of acetylation of the protein portion. In view of the important role of LDL and its modified (oxidized) form in the development of arteriosclerosis, a new hypothesis emerged that sees the damage to endothelial cells only as a partial step in a sequence of complex processes. The oxidative modification of LDL or the contents of the LDL particles is seen as the real cause of the initiation of the arteriosclerotic process.
Further course
In the description of the further course, both hypotheses are identical. The formation of foam cells causes an inflammatory reaction which in the further course can spread to deeper areas of the arterial wall - such as the media with its muscle cells. The result is a gradual tissue remodeling, with a connective tissue-like cap forming in the artery , which has a lipid core inside. The lipid core results from the content of the dead foam cells that have absorbed a large amount of oxidized LDL particles. Blood clotting reactions then take place on broken arteriosclerotic plaques , which further reduce the diameter of the arteries. This tissue remodeling makes the damaged artery brittle. The final stage of this process is known colloquially as "hardening of the arteries". The formation of arteriosclerotic plaques can be reversed until the foam cells have increased. This effect was observed in a number of people who started endurance sports, with the cholesterol level falling significantly and the ratio of the various lipoproteins shifting significantly towards HDL . Beyond this stage the process is no longer reversible; the damage is permanent.
Further research
The intestinal flora is also believed to have an influence on the development of arteriosclerosis . For example, intestinal germs can form trimethylamines from the phosphatidylcholines (also known as “ lecithin ”) and L- carnitine ingested with food , which are then metabolized to trimethylamine-N-oxide (TMAO) in the liver . This has pro-arteriosclerotic properties and it is assumed that TMAO suppresses the transport of cholesterol out of the cell. This leads to the deposition of cholesterol on the vessel walls, which promotes the development of arteriosclerosis. Trimethylamine-producing germs are found particularly in a meat-rich diet. The formation of TMA can be inhibited by 3,3-dimethyl-1-butanol , which in animal models prevents arteriosclerosis despite pro-arteriosclerotic nutrition.
It has been proven that Porphyromonas gingivalis , the marker germ for severe and aggressive forms of periodontitis and thus responsible for the loss of teeth , can penetrate intracellularly into macrophages , epithelial , endothelial and smooth muscle cells , survive there and move from one cell to the other next can spread. Porphyromonas gingivalis could therefore possibly use these cells as a means of transport to get to peripheral tissues. Porphyromonas gingivalis has been found in atherosclerotic plaques, which can contribute to the progression of atherosclerosis.
localization
The inner walls of the blood vessels are lined with endothelial cells that are exposed to shear stress due to the flow of blood . The endothelial cells perceive the shear stress and react to it with the production of nitrogen monoxide (NO). NO dilates the blood vessel and inhibits smooth muscle growth. NO also inhibits the accumulation of platelets and immune cells on the vessel wall and the oxidation of LDL in the intima. In this way, the NO protects locally against atherosclerosis.
The blood cannot flow evenly ( laminar ) at the branching vessels, but forms - reinforced by the pulsatile blood flow - eddies in which the flow direction of the blood changes chaotically (turbulent flow). Under these conditions, the endothelial cells switch on proinflammatory signaling pathways and produce less NO. As a result, branching vessels are particularly often affected by atherosclerosis.
As a result of arteriosclerosis, constrictions and occlusions can form in the affected vessel sections. The vessel wall can also be weakened to such an extent that it expands and creates an aneurysm . Both the constrictions and the widenings in turn cause disturbances in the laminarity of the blood flow, as a result of which the endothelial damage, which is stimulated by the flow conditions, continues.
Frequent and significant consequences of arteriosclerosis are stroke when the large cervical arteries ( common carotid artery , internal carotid artery ) are affected, myocardial infarction when coronary arteries clog, dilation of the abdominal artery ( aortic aneurysm ) and arterial occlusive disease of the legs (PAD) . The arterial vessels that supply the internal organs with blood are more rarely affected. Symptomatic PAD of the arm arteries is found in around ten percent of cases.
Risk factors
The PROCAM study cites as risk factors ( Cardiovascular risk factors CVRF) in order of relevance:
- Gender ( androtropia )
- Age
- LDL cholesterol ( hypercholesterolemia , hyperlipidemia )
- Smoking status ( tobacco smoking )
- HDL cholesterol (low)
- systolic blood pressure ( arterial hypertension )
- premature heart attacks in the family ( family history )
- Diabetes ( diabetes mellitus )
- Triglycerides
Other risk factors are:
- Lipoprotein a
- Obesity and an increased waist-to-hip ratio
- unhealthy lifestyle
- High-energy and high-fat diet : There is evidence that suggests that the quality of the diet and the composition play a role, with a Mediterranean diet appearing to be superior to a low-fat diet.
- stress
- constitutional factors (e.g. depression)
- Environmental factors (e.g. particulate matter pollution, nocturnal noise).
Likewise, other diseases such as chronic kidney failure , hyperthyroidism (overactive thyroid), gout and rheumatoid arthritis can increase the risk of atherosclerosis secondarily.
In general, the risk factors can be divided into those that cannot be modified, such as age, gender and genetic predisposition, and those that can be influenced. However, it has not been scientifically shown for all modifiable risk factors that a reduction in the risk factor is also associated with a lower risk of atherosclerosis. Risk factors, the correction of which has been proven and relevant to the prognosis, are smoking, high blood pressure and the consumption of animal fats.
Treatment options and preventive measures
The prevention and treatment options for arteriosclerosis are largely identical and differ mainly in terms of their extent. Only invasive medical (surgical) interventions are added to the treatment options . The most important things for pure prevention in otherwise healthy people are sufficient exercise and a generally healthy diet.
Medical therapy
Medicinal / non-invasive
- High blood pressure reduction: ACE inhibitors , diuretics , AT1 receptor blockers , beta-blockers , calcium antagonists
- Cholesterol lowering: statins , ezetimibe , polyphenols
- Lowering of triglycerides: omega-3 fatty acids ethyl esters, fibrates , nicotinic acid
- Antiplatelet agents: acetylsalicylic acid , clopidogrel , dipyridamole
- drug therapy of risk-increasing additional diseases (see risk factors )
Invasive
- Bypass surgery on the heart or legs
- Thrombendarterectomy of the leg or carotid artery
- Expansion by balloon dilatation or stent
- invasive therapy of additional diseases that increase the risk (see risk factors )
Avoidance of risk factors
- Chronic high blood pressure should be normalized.
- The tobacco smoking should be completely adjusted: Because nicotine acts vasoconstrictor starting at low doses, a mere reduction in supply is not pointless, but by much less effect than the total abandonment.
- Specific diseases that increase the risk of atherosclerosis must be treated and their risk factors avoided. These include u. a. Diabetes mellitus and chronic kidney failure (see also: Risk factors ).
- Strong, persistent, negative stress should be avoided. Among other things, it favors the risk factors high blood pressure and obesity.
- The body weight should be in the normal to maximally slightly overweight range. People who are extremely overweight have more frequent and / or more severe arteriosclerotic changes.
- It is recommended that you use medication to lower high cholesterol. The connection between high cholesterol levels and the development of coronary heart disease is, however, controversial (see also: main article cholesterol, paragraph: Doubt about the causal chain of nutrition - cholesterol - coronary heart disease ).
Move
Adequate exercise even in light form (walks) can have a considerable influence on the development and course of arteriosclerotic diseases. Endurance sports in the scope of recreational sports are recommended as regular sports. Sport on the scale of competitive sport is neither considered necessary nor recommended.
- Walks, from 20 minutes daily (if no other sport is added).
- Jogging, cycling, swimming, skating, ball and team sports etc.
- Sports studio: In the studio, endurance training should be emphasized in courses and on appropriate equipment.
nutrition
The general rules of healthy human nutrition should be observed (including plenty of vegetables, fruits and whole grain products). However, the typical Mediterranean diet is particularly recommended in connection with atherosclerosis.
- Dietary fiber (especially soluble) from whole grain products, legumes and vegetables lower the LDL cholesterol level . Dietary fiber binds bile acid , which is then not available to emulsify the fats. In order to meet the bile acid requirement, the liver increases synthesis. In order to synthesize bile acid, the liver has to remove LDL cholesterol from the bloodstream. Furthermore, dietary fiber is important for a healthy intestinal function with their general positive consequences for the organism.
- Saturated fat (in solid vegetable fats and especially in animal fats) increases daily caloric intake without the health benefits of unsaturated fatty acids. For this reason, you should partially do without these fats and replace them with monounsaturated and polyunsaturated fats.
- The monounsaturated oleic acid , abundant in olive oil and rapeseed oil, lowers LDL cholesterol without changing the beneficial HDL cholesterol. Polyunsaturated fatty acids such as linoleic acid (omega-6 fatty acid) and alpha-linolenic acid ( omega-3 fatty acids ) lower total cholesterol levels. The ratio of omega-6: omega-3 should not exceed 5: 1, since both fatty acids compete for the same enzyme systems. By far the most favorable ratio has linseed oil with approx. 1: 4; Linseed oil also has the highest proportion of omega-3 fatty acids of all edible oils. The fatty acids mentioned are essential components of a vegetarian diet. Nuts and fatty fish (herring, salmon, black halibut) also have favorable fatty acid patterns. Linoleic acid and linolenic acid also have an anti-inflammatory effect (although in some cases they also promote inflammation, especially linoleic acid).
- Arginine is a dietary amino acid that is essential for maintaining vascular health and can be used successfully in the dietary therapy of arteriosclerosis. The metabolic disorders underlying this disease can be favorably influenced by increased nitrogen monoxide (NO) formation from arginine, and thus a causal treatment with a nutrient is possible. All pro-oxidative and inflammatory degenerative processes triggered by the endogenous antagonist of arginine, asymmetric dimethylarginine (ADMA), can thus be successfully compensated. Arginine is often combined with B vitamins to lower levels of homocysteine , which inhibits the breakdown of ADMA.
- Antioxidants such as vitamin E (nuts, vegetable oils), vitamin C and carotenoids from vegetables and fruits as well as other phytochemicals reduce oxidative stress. Artificial intake in the form of food supplements should only be limited or if there is a proven deficiency, as these are not a substitute for a balanced diet and a healthy lifestyle. Isolated phytochemicals have by far not proven the same effect as the whole food.
- In salt-sensitive high blood pressure patients, it makes sense to replace table salt in favor of herbs and spices to enhance the taste.
- Fried, grilled, deep-fried and baked dishes and foods that contain artificially hydrogenated fats according to certain processes (e.g. margarines produced according to older processes) should only be consumed rarely because of the high proportion of harmful trans fatty acids .
Secondary diseases
The consequences of arteriosclerosis are primarily based on circulatory disorders such. B.
- of the legs ( PAOD ),
- of the heart ( coronary artery disease ) with myocardial infarction and angina pectoris or
- of the abdominal vessels ( angina abdominalis , intestinal infarction , nephrosclerosis ).
With regard to the brain, for example, the detachment of arteriosclerotic plaques can lead to a stroke or dementia changes .
Diagnosis
- Physical examination
- Walking test - does it cause pain when walking? Distance <200 m,> 200 m?
- Ratschow's positioning test - legs or arms are raised to the maximum, then the feet or hands are rolled / opened and closed. After a minute or if there is pain, the extremities are left hanging and the time until the veins are filled. More than seven seconds indicate closed vessels. (Not used in severe PAD or heart failure.)
-
Sonography or duplex sonography to determine the flow rate of the blood
- the carotid arteries , the intracranial vessels, the heart valves , the abdominal aorta , the leg arteries
- intravascular ultrasound examination of the coronary arteries
-
Angiography
- the carotid arteries, the coronary arteries , the abdominal aorta, the leg arteries
- Laboratory values
- Asymmetrical dimethylarginine (ADMA), cholesterol (LDL / HDL / VLDL / triglycerides), blood sugar , HbA1c value, homocysteine , uric acid
-
CT
- Almost CTt of the coronary arteries, CT of the abdominal artery
-
MRI
- the carotid arteries, the aorta
literature
- T. Gui, A. Shimokado et al. a .: Diverse roles of macrophages in atherosclerosis: from inflammatory biology to biomarker discovery. In: Mediators of inflammation. 2012, p. 693083, ISSN 1466-1861 . doi: 10.1155 / 2012/693083 . PMID 22577254 . PMC 3337637 (free full text). (Review)
Individual evidence
- ↑ A. Becker et al.: A comparative study of clinically well-characterized human atherosclerotic plaques with histological, chemical, and ultrastructural methods. In: J Inorg Biochem. 98, 2004, pp. 2032-2038.
- ^ I. Böhm et al.: Molecular imaging of apoptosis in cardiovascular diseases. In: Fortschr Röntgenstr RöFo. 179, 2007, pp. 780-789.
- ↑ D. Steinberg, S. Parthasarathy, TE Carew, JC Khoo, JL Witztum: Beyond cholesterol. Modifications of low-density lipoprotein that increase its atherogenicity In: N. Engl. J. Med. Vol. 320, 1989, pp. 915-924.
- ^ ME Haberland, UP Steinbrecher: Modified Low-Density Lipoprotein: Diversity and biological relevance in atherogenesis. In: Monographs in human Genetics. Karger, Basel 1992, pp. 35-61.
- ↑ Susan V. Lynch, Oluf Pedersen: The human intestinal microbiome in health and disease . The New England Journal of Medicine 2016, Volume 375, Issue 24, December 15, 2016, pages 2369-2379, doi: 10.1056 / NEJMra16002266
- ↑ EV Kozarov: Human Atherosclerotic Plaque Contains Viable Invasive Actinobacillus actinomycetemcomitans and Porphyromonas gingivalis. In: Arteriosclerosis, Thrombosis, and Vascular Biology. 25, 2005, p. E17, doi: 10.1161 / 01.ATV.0000155018.67835.1a .
- ↑ Irina M. Velsko, Sasanka S. Chukkapalli u. a .: Active Invasion of Oral and Aortic Tissues by Porphyromonas gingivalis in Mice Causally Links Periodontitis and Atherosclerosis. In: PLoS ONE. 9, 2014, p. E97811, doi: 10.1371 / journal.pone.0097811 .
- ↑ Zahra Armingohar, Jørgen J. Jørgensen u. a .: Bacteria and bacterial DNA in atherosclerotic plaque and aneurysmal wall biopsies from patients with and without periodontitis. In: Journal of Oral Microbiology. 6, 2014, p. 23408, doi: 10.3402 / jom.v6.23408
- ^ Robert Franz Schmidt , Florian Lang, Manfred Heckmann (eds.): Physiology of humans . 31st edition. Springer Medizin Verlag, Heidelberg 2010, ISBN 978-3-642-01650-9 , p. 602-604 .
- ^ Herbert Renz-Polster , Steffen Krautzig: Basic textbook internal medicine. 4th edition. Elsevier 2008, ISBN 978-3-437-41053-6 , p. 218.
- ↑ Pia R. Kamstrup, Anne Tybjærg-Hansen, Børge G. Nordestgaard: Elevated Lipoprotein (a) and Risk of Aortic Valve Stenosis in the General Population In: Journal of the American College of Cardiology. doi: 10.1016 / j.jacc.2013.09.038
- ^ JO Gebbers: Atherosclerosis, cholesterol, nutrition, and statins - a critical review. (Atherosclerosis, Cholesterol, Diet, and Statins - A Critical Review). In: Ger Med Sci. 2007; 5; Doc04, online versions: PDF; 2.4 MB , HTML
- ↑ SD Adar, L. Sheppard, S. Vedal, JF Polak, PD Sampson, AV Diez Roux, M. Budoff, DR Jacobs, RG Barr, K. Watson, JD Kaufman: Fine particulate air pollution and the progression of carotid intima- medial thickness: a prospective cohort study from the multi-ethnic study of atherosclerosis and air pollution. In: PLoS medicine. Volume 10, Number 4, April 2013, p. E1001430, ISSN 1549-1676 . doi: 10.1371 / journal.pmed.1001430 . PMID 23637576 .
- ↑ Particulate matter pollution and nocturnal noise as independent risk factors for atherosclerosis, April 2013
- ^ UGB: Healthy food for a healthy heart ( Memento from September 28, 2007 in the Internet Archive ).
- ↑ Melchert HU, Limsathayourat N, Mihajlović H, Eichberg J, Thefeld W, Rottka H: Fatty acid patterns in triglycerides, diglycerides, free fatty acids, cholesteryl esters and phosphatidylcholine in serum from vegetarians and non-vegetarians. , Atherosclerosis. 1987 May; 65 (1-2): 159-66, PMID 3606730
- ↑ A. Ströhle, A. Hahn: Arginine in atherosclerosis. In: Deutsche Apotheker Zeitung. 20, 2012, pp. 97-102 and 21, 2012, pp. 74-83.
- ↑ Y. Bai et al. a .: Increase in fasting vascular endothelial function after short-term oral L-arginine is effective when baseline flow-mediated dilation is low: a meta-analysis of randomized controlled trials. In: Am J Clin Nutr. 89, 2009, pp. 77-84.