Subcortical arteriosclerotic encephalopathy
| Classification according to ICD-10 | |
|---|---|
| I67.3 | Progressive subcortical vascular encephalopathy - Binswanger's disease |
| F01.2 | Subcortical vascular dementia |
| ICD-10 online (WHO version 2019) | |
The subcortical arteriosclerotic encephalopathy (SAE, synonyms: Binswanger's disease , Binswanger's disease , vascular encephalopathy ) is a by vascular changes ( arteriosclerosis caused) disease of the brain ( Enzephalon ) located below the cerebral cortex ( Cortex so) subcortical to damage ( pathology results) . It was first described by the Swiss neurologist Otto Ludwig Binswanger (1852–1929) in Jena .
Pathogenesis
The SAE is characterized by many infarcts in combination with a vascular demyelination of the medullary bed (i.e. a decrease in the nerve cell fibers that connect the cerebral cortex with the subcortical brain structures) with a diffuse reduction in density around the cerebral ventricle (periventricular) in the computed tomogram . These ischemias seem to be caused by changes in the vascular wall ( lipohyalinosis ) of small arteries in the deeper brain. There is a thickening of the vessel wall, which leads to a narrowing of the lumen . The demyelination appears to be ischemic , which is due to the decrease in perfusion pressure in hypotonic episodes. In patients with SAE, arterial hypertension , diabetes mellitus and recurrent infarctions can often be found in different brain regions.
Progressive multifocal leukoencephalopathy , leukodystrophy and mitochondrial diseases show a similar pathological-anatomical picture .
Symptoms
Characteristic symptoms can hardly be summarized since the small infarcts do not necessarily become symptomatic. However, since the medullary bed is primarily affected, one can assume that mainly disturbances in the conduction of excitation occur. Often, but not necessarily, and often only after several years of progress, intellectual and affective flattening (“leveling”) in combination with neuropsychological disorders can occur.
Later on, subcortical arteriosclerotic encephalopathy can lead to vascular subcortical dementia , which is probably responsible for most of the symptoms of vascular dementia. Characteristic symptoms of subcortical arteriosclerotic encephalopathy are:
Gait disorder
It is an unsteady, clumsy walk with legs apart, which is mostly described as "frontal" or "apractical", but does not imitate the small, rhythmic "shuffling" of Parkinson's disease . The muscle tone is spastically increased, so the pyramidal tract is involved in the symptoms. The emphasis on the lower extremities corresponds to the position of the pathways, whereby the topographical arrangement shows the pathways for the legs most medially (near the ventricle). The muscle reflexes are increased (weakened or absent in Parkinson's disease) and the pyramidal signs are often positive.
Bladder disorder
The imperative to urinate and urine loss up to urinary incontinence are common, the central bladder path is directly connected laterally to the path of the legs.
Subcortical dementia
Slowing down and loss of drive are similar to Parkinson's behavior, and social withdrawal is also an early symptom. As a result, paranoid-hallucinatory symptoms appear, while the noopsychic cortical functions such as abstract thinking and long-term memory remain unaffected for a long time. But the dementia is progressing.
Diagnostic criteria
- Limitation of the higher brain performance (dementia) as well
- Two of the following symptoms
- Hypertension or general vascular disease
- Chronic vascular insufficiency (disorder of blood vessels)
- Subcortical dysfunction (gait disorder, rigidity, bladder disorder)
The behavioral disorders in people with dementia are called BPSD (Behavioral and Psychological Symptoms of Dementia). These include apathy (76.0%), aberrant motor behavior (= wandering around aimlessly; 64.5%), eating disorders (eating inedible things; 63.7%), irritability / lability (63.0%), agitation / Aggression (62.8%), sleep disorders (53.8%), depression / dysphoria (54.3%), anxiety (50.2%), delusion (49.5%), disinhibition (29.5%), Hallucinations (27.8%), and euphoria (16.6%).
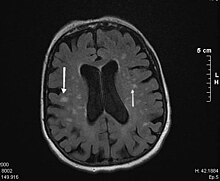
Imaging diagnostics
The diagnosis is confirmed with an MRI (magnetic resonance imaging = magnetic resonance imaging). In the T2-weighted images, this shows typical whitish confluent foci around the ventricles and a cap-like sclerosis zone, especially at the anterior and posterior ends of the lateral ventricles.
The “status lacunaris” must be differentiated from this in terms of differential diagnosis. Multi-infarct events, especially in atrial fibrillation , where small infarcts (micro-infarcts) produce a similar clinical picture in the same areas. CADASIL occurs very rarely .
therapy
A causal therapy does not yet exist because the exact cause of the SAE has not been clarified. There are no surgical treatment options. The possibilities of drug influence are small. The therapeutic goal should be to avoid both short-term hypotonic and long-term hypertonic episodes, as this combination is a significant risk factor for SAE. In addition, known risk factors should be “positively influenced”, such as B. by abstaining from nicotine, weight loss, treatment of heart failure and cardiac arrhythmias.
physical therapy
Because of the extrapyramidal movement disorder, which is in the foreground, this area is initially of the greatest importance. New strategies to compensate for imbalance, gait and coordination are necessary and must be started early.
Occupational therapy
Because of the coordination disorder, especially the two-handed coordination and the combination with apractical symptoms, their use is important. Incontinence counseling and the provision of appropriate means, supply of incontinence material and advice on drinking habits make life easier for those affected and their relatives.
Cognitive training and drug treatment
Is carried out by psychologists and occupational therapists or together and aims at independence, personal responsibility and better orientation. In the case of behavioral disorders, non-pharmacological interventions have recently been favored. Only if these are insufficient should medical help be used. Here are v. a. Antidepressants , serotonin inhibitors , antihypertensive drugs ) to treat the accompanying symptoms. Nootropics show effects of small magnitude and of limited duration in only a fraction of patients. The effect of acetylcholinesterase inhibitors, which have the most well-documented effects in the treatment of Alzheimer's disease, is being investigated on vascular disorders of the brain (status: 2000).
Differential diagnosis
- Multi-infarct dementia (MID) ICD 10: F01.1
- Normal pressure hydrocephalus
- Alzheimer's disease
- multiple sclerosis
- Radiation damage
- Leukodystrophy
- Brain edema
- HIV encephalopathy
- Progressive multifocal leukoencephalopathy
- CARASIL
literature
- Oliver Christian Hund: Analysis of neuropsychological failure profiles in cerebral microangiopathy. Inaugural dissertation to obtain the doctoral degree of the Medical Faculty of the Georg-August-Universität zu Göttingen, 2013. (Archived at the German National Library)
- Christiane Elisabeth Ehrenfeld: Subcortical arteriosclerotic encephalopathy and normal pressure hydrocephalus in comparison. Dissertation. University of Essen. 1997, DNB 954646517 .
- CG Olsen, ME Clasen: Senile dementia of the Binswanger's type. . In: Am Fam Physician. 1998 Dec; 58 (9), pp. 2068-2074. (Review: PMID 9861880 )
- Rupert Püllen, Rudolf Harlacher: Unfortunate Liaison. Stroke and vascular dementia. In: Geriatrics Practice. 10 (1998), pp. 46-49.
- T. Wetterling: Vascular dementia. A coherent concept? In: Journal of Gerontology and Geriatrics. 31 (1998), pp. 36-45, doi : 10.1007 / s003910050016 .
- T. Wetterling: Vascular dementia. Differential diagnosis and therapeutic approaches. In: Claus Wächtler (Ed.): Dementia. The challenge; Documentation of the 2nd annual meeting of the German Society for Gerontopsychiatry and Psychotherapy from 2-4. February 1995 in Hamburg. Singen 1996, ISBN 3-9804647-1-7 , pp. 161-163.
Web links
- Binswanger's disease in the lexicon at doccheck.com
Individual evidence
- ↑ D. Stuss, JL Cummings: Subcortical vascular dementia . In: JL Cummings (Ed.): Subcortical dementia. Oxford University Press, New York 1990, pp. 145-163.
- ↑ Subcortical arteriosclerotic encephalopathy . at Kranken.de, accessed on October 29, 2012.
- ↑ JL Cummings: The Neuropsychiatry of AD and Related Dementias . Taylor & Francis, London 2003.
- ^ J. Cohen-Mansfield: J. Nonpharmacologic interventions for inappropriate behaviors in dementia: a review, summary, and critique . In: Am J Geriatr Psychiatry. 2001 Fall; 9 (4), pp. 361-381. doi : 10.1097 / 00019442-200111000-00005
- ↑ Binswanger's disease on the website of the German Alzheimer Society (DAlzG)
- ↑ Willibald Pschyrembel : Clinical Dictionary . 266th edition. de Gruyter, Berlin / Boston 2014, p. 1393.