Hyperlipoproteinemia
| Classification according to ICD-10 | |
|---|---|
| E78 | Disorders of lipoprotein metabolism and other lipidemias |
| E78.0 | Pure hypercholesterolemia |
| E78.1 | Pure hypertriglyceridemia |
| E78.2 | Mixed hyperlipidemia |
| E78.3 | Hyperchylomicronemia |
| E78.6 | Lipoprotein deficiency |
| ICD-10 online (WHO version 2019) | |
Under hyperlipoproteinemia (HLP) or hyperlipidemia is generally understood as an increased concentration of cholesterol , the triglycerides and lipoproteins with displacement of the relative proportion of LDL - or VLDL fraction in the blood .
A distinction is made between primary and secondary hyperlipoproteinemia. Primary hyperlipoproteinemia is a disease of its own, mostly genetic, while secondary hyperlipoproteinemia is a sequela of other underlying diseases. Most patients with hyperlipoproteinemia have a combination of genetic predisposition (often polygenic, see point 1) and external factors (lifestyle, diseases or medication, see point 2).
Disorders of the lipoprotein metabolism are among the most frequently diagnosed diseases in Germany.
Primary hyperlipoproteinemia
The primary hyperlipoproteinemias can be differentiated using the Fredrickson classification . The values for total cholesterol , LDL cholesterol and HDL cholesterol as well as the triglycerides are taken into account. The color of the fasting serum and the result of gel electrophoresis ( lipid electrophoresis ) are also included in the classification. It should be noted that the Fredrickson classification does not take into account lipoprotein a or the genetic causes on which the hyperlipoproteinemia is based.
HLP type 1 (exogenous hyperlipidemia, hyperchylomicronemia)
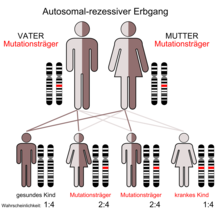
Rare; inherited as an autosomal recessive trait; Posthepatic lipoprotein lipase defect ; strongly delayed breakdown of chylomicrons; there is pathological deposition of lipids in the liver, spleen and skin ( xanthomas ). With HLP type 1 there is no increased risk of arteriosclerosis .
HLP type 1 is characterized in the laboratory by normal total cholesterol levels and increased triglycerides. LDL cholesterol and HDL cholesterol are lower than the reference values. The fasting serum is clear at the bottom and appears "creaming" on the surface. In gel electrophoresis, the band of the chylomicrons is very clear, the other bands (beta, pre-beta and alpha) are still clearly visible.
HLP type 2 (familial hyperlipidemia, hypercholesterolemia)
See also the main article Homozygous Familial Hypercholesterolemia
Frequently; inherited as an autosomal dominant trait; Defect of the LDL receptor as a result of a mutation of the receptor gene (on chromosome 19 ); Since LDL cannot be absorbed into the liver or can only be absorbed to a limited extent, the LDL cholesterol level in the blood increases. In addition, the lack of absorption of LDL by the liver means that the feedback inhibition of cholesterol synthesis is lost, which leads to excessive VLDL synthesis in the liver. The resulting LDL increases the serum cholesterol level massively.
In HLP type 2a, familial hypercholesterolemia , there is an isolated increase in LDL with the consequences described above, while in type 2b, mixed hyperlipidemia , the triglycerides are also slightly increased. This is likely due to an overproduction of ApoB, which increases VLDL formation.
In contrast to type 1, type 2a is characterized by increased total cholesterol values and normal triglyceride values. The LDL cholesterol is increased, the HDL cholesterol is often lowered to normal. The fasting serum is clear. A gel electrophoresis showing the bands alpha and pre-beta. Xanthomas are tendinous / tuberous.
85 to 90 percent of type 2a is caused by mutations in the LDL receptor gene; the mutation can be over 1,600 gene loci. Depending on whether the genetic defect affects only one or both homologous chromosomes, a distinction is made between a heterozygous or a homozygous form of familial hypercholesterolemia. The much more common, heterozygous familial hypercholesterolemia occurs when the genetic defect is inherited from only one parent. Their estimated prevalence is 1: 500. In homozygous familial hypercholesterolemia (HoFH), the genetic defect is passed on to the child from both parents. In general, a prevalence of around 1: 1,000,000 is assumed. Since the defective alleles are inherited from both parents in homozygous individuals, the disease is particularly pronounced. Patients with HoFH develop massive arteriosclerosis and circulatory disorders in childhood and suffer heart attacks early on. In the long term, xanthomas in the skin (cutaneous) and tendons (tendinous) as well as an early onset of cardiovascular disease with a correspondingly shorter life expectancy occur. Since hypercholesterolemia is a risk factor for cardiovascular events, drug treatment is usually useful for such patients. It is particularly important to bring patients in the high and high risk groups to their individual target values.
Type 2b has both increased total cholesterol and increased triglyceride levels. LDL cholesterol is high, HDL cholesterol is often low. The gel electrophoresis shows strong beta and pre-beta bands, the alpha band is visible. The fasting serum is slightly cloudy. Xanthomas are tendinous and tuberous.
HLP type 3 (remnant hyperlipidemia, broad beta disease)
Very rare; inherited as an autosomal recessive trait; abnormal apolipoprotein E leads to incomplete degradation of the chylomicron remnants and IDL, so that their plasma concentrations increase. The consequences are a massively increased risk of arteriosclerosis.
Type 3, like type 2b, has elevated total cholesterol levels and triglycerides in the laboratory. LDL cholesterol is often normal to slightly elevated. HDL cholesterol mostly lowered. Gel electrophoresis shows a clear pre-beta band and a lighter alpha band. Pre-β and β fractions are fused into one broad "band". The fasting serum is cloudy.
HLP type 4 (endogenous hyperlipidaemia, hypertriglyceridaemia)
Frequently; inherited as an autosomal dominant trait; there is an overproduction of endogenous triglycerides and a reduced utilization of VLDL triglycerides, which leads to an increase in VLDL. The consequences are epigastric colic (due to pancreatitis ), increased risk of arteriosclerosis, obesity, fatty liver, hyperuricemia (increased uric acid level, which can lead to gout ) and the like. v. m.
Type 4 shows normal to slightly increased total cholesterol and significantly increased triglyceride levels in the laboratory. LDL cholesterol is usually normal, HDL cholesterol is often low. The fasting serum is cloudy. Gel electrophoresis shows a clear pre-beta band and a weaker beta and alpha band.
HLP type 5 (combined hyperlipidemia, endogenous-exogenous hypertriglyceridemia)
The pathogenesis of HLP type 5 is unclear. The consequences are obesity , fatty liver , hepatosplenomegaly , epigastric colic and xanthomas of the skin. The risk of arteriosclerosis is not increased.
Type 5 shows normal to increased total cholesterol levels and increased triglyceride levels in the laboratory. LDL cholesterol is usually high, HDL cholesterol is often low. The fasting serum is cloudy and creamy. Gel electrophoresis shows clear pre-beta and chylomicron bands and weaker beta and alpha bands.
Secondary hyperlipoproteinemia
The following underlying diseases are named as causes of secondary hyperlipoproteinemia:
- alcoholism
- Overeating
- Malnutrition
- Nephrotic Syndrome
- Pancreatitis
- Liver disease
- Cholestasis
- Diabetes mellitus
- Hyperuricemia
- Hypothyroidism
- Acromegaly
- Glycogenoses
- Hypercalcemia
Temporary hyperlipoproteinemia can also develop through the use of ovulation inhibitors and through pregnancy . As a rule, the secondary hyperlipoproteinemia is cured by treating the respective underlying disease.
literature
- Regine Witkowski ao: Lexicon of Syndromes and Malformations. Causes, Genetics, and Risks. 7th edition. Springer Verlag, Berlin 2004, ISBN 3-540-44305-3 , p. 579ff.
Individual evidence
- ↑ Most frequent diagnoses in medical practices: Federal health reporting .
- ↑ ESC / EAS guidelines 2016: [1] .