Hyperuricemia
| Classification according to ICD-10 | |
|---|---|
| E79.0 | Hyperuricemia with no signs of inflammatory arthritis or topical gout |
| M10 | gout |
| ICD-10 online (WHO version 2019) | |
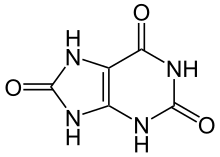
As a hyperuricemia (formerly referred to simply as Urikämie) is an elevated uric acid level in the blood called. It can lead to gout .
definition
An increase in the serum uric acid concentration to ≥ 6.5 mg / dl (387 µmol / l) is by definition hyperuricemia. This determination is based on the physical solubility limit for sodium urate (sodium salt of uric acid ) in plasma at 37 ° C and pH 7.4 of 6.4 mg / dl (381 µmol / l). This limit applies to both sexes.
In the hormone-active years, women have, on average, lower serum uric acid values than men. This is due to the female hormone metabolism, with the predominance of estrogens. In relation to the limit value for hyperuricemia of 6.5 mg / dl, the incidence of hyperuricemia in the general population is frequent. In one study, it was 2.6% for female blood donors and 28.6% for men.
Classification
In general, a distinction can be made between primary hyperuricemia (90%) and secondary hyperuricemia (10%).
Primary hyperuricemia
Primary hyperuricemia is also known as idiopathic or familial hyperuricemia. The cause is usually reduced uric acid excretion in the kidneys (approx. 99% of cases) with otherwise normal kidney function, only rarely is there an overproduction of uric acid due to a congenital disorder (enzyme defect) of the purine metabolism (approx. 1% of cases), such as B. a deficiency of the enzyme hypoxanthine guanine phosphoribosyl transferase (HGPRTase for short).
The delimitation of uric acid overproduction from reduced excretion by the kidneys can be done by determining the uric acid clearance (for the calculation, the uric acid excretion in the urine collection (over 24 hours) and the serum uric acid must be determined) or - less meaningfully - by determining the uric acid / creatinine quotient respectively.
Secondary hyperuricemia
In secondary hyperuricemia, hyperuricemia is the result of another disease (e.g. reduced excretion in the case of renal insufficiency, increased cell breakdown in starvation diets or malignancies (malignant tumor) ), drug therapy (e.g. certain diuretics) or increased purine intake through the Food (including meat, offal ).
- Increase in uric acid formation due to increased purine release due to increased cell turnover or cell breakdown
- Polycythemia vera
- chronic myeloid leukemia
- Tumor treatment with cytostatics
- Increase in uric acid production due to increased purine synthesis
- Glycogen storage disease type I
- Increase in uric acid production due to reduced breakdown in the purine metabolism
- Decrease in uric acid excretion by the kidneys (renal)
clinic
Hyperuricemia remains clinically asymptomatic in most cases. But you can, u. a. depending on the extent of the increase in the concentration of uric acid in the blood or tissues, manifest in different forms:
- acute gout attack
- chronic gout with soft tissue and bone tophi (nodules)
- Kidney disease ( kidney stones , urate nephropathy )
therapy
In principle, a lowering of the uric acid level should be aimed for through dietary measures. The intake of purines , which are broken down into uric acid by the metabolism, should be reduced ( low-purine diet ). Purines are cell components of animal, vegetable and fungal cells that arise either during the body's own breakdown or are ingested through food. Foods containing cells in particular are, for example, offal, meat products, fish and, in particular, the skin of fish and poultry. The purines can pass into the cooking water when they are boiled. No more than 3000 mg uric acid or 500 mg per day should be consumed weekly.
Drinks containing alcohol should be avoided if possible or only consumed in small quantities, as alcohol inhibits uric acid excretion via the kidneys. In addition, some fermented beverages may contain purines (e.g. beer and wine due to the yeast ).
A normalization of obesity can have a favorable impact on the level of uric acid in the blood. Fatty diets promote the formation of ketone bodies in the blood, which reduce the excretion of uric acid via the kidneys, but this plays only a minor role clinically. A rapid reduction in obesity is not advisable, however, because larger amounts of the urate deposit in the body are released from the fatty tissue into the blood and thus the uric acid level increases or stabilizes at a high value despite increased excretion.
The daily intake should be at least 2 liters. This results in improved uric acid excretion and if there is an increased amount of uric acid, the formation of uric acid stones can be avoided. In the majority of patients with hyperuricaemia (approx. 95%) there is a reduced excretion of uric acid via the kidneys and thus only a low risk of the formation of kidney stones from uric acid. Kidney stones from uric acid ( X-ray negative !) Are an indication of an increased attack of uric acid e.g. B. by an enzyme defect (most important: HGPRTase deficiency), increased cell breakdown (e.g. by malignancies and / or their treatment or extreme starvation diets) or excessive purine intake.
In the case of uric acid levels> 9 mg / dl, frequent attacks of gout or other complications of hyperuricemia, in addition to the dietary recommendations, drug treatment is useful or necessary.
For long-term therapy elevated uric acid levels is treatment with uricostatics ( febuxostat and allopurinol ) or uricosuric agents (eg. B. benzbromarone ), or a combined preparation of both (allopurinol + benzbromarone) possible. A withdrawal attempt immediately after the uric acid level has normalized by the medication is usually not useful, except in cases in which the cause of the hyperuricemia has been permanently eliminated in the meantime (e.g. weight normalization, discontinuation of a diuretic causing hyperuricemia, end of alcohol abuse) . The permanent lowering of the uric acid level should and can prevent the manifestation of complications (gout, kidney stones, nephropathy). It is essential to understand the urate depot in the body, which builds up with permanent values of> 6.5 mg / dl and which must first be significantly reduced. It can take several years to dissolve an extensive urate deposit (partly in adipose tissue).
In acute gout attacks , nonsteroidal anti-inflammatory drugs (NSAIDs) such as indomethacin , ibuprofen or diclofenac have long been the first choice. An alternative is colchicine , which is now used in low doses (e.g. 3 × 0.5 mg / day) because it is better tolerated. Because of the good effect with comparatively few side effects of short-term therapy, steroids are increasingly being used for the treatment of acute gout attacks.
Individual evidence
- ^ Günter Thiele: Handlexikon der Medizin , Volume 4 (S − Z), Urban & Schwarzenberg, Munich / Vienna / Baltimore 1980, p. 2551.
- ↑ U. Gresser u. a .: Uric acid levels in Southern Germany in 1989 . In: Klinische Wochenschrift 68, 1990, pp. 1222-1228.
- ↑ C. Gaster: Gout, a disease of affluence . In: UGB-Forum 4, 2012, pp. 192–195.
literature
- L. Thomas (Ed.): Laboratory and diagnosis . 5th edition. TH-Books-Verl.-Ges., Frankfurt a. M. 1998, ISBN 3-9805215-3-2 .
- U. Gresser: Diagnosis and therapy of gout . In: Deutsches Ärzteblatt . Volume 100, Issue 44, 2003, A 2862–2870.
- Attila Dunky, Rudolf Eberl: Gout and Hyperuricemia. G. Braun, Karlsruhe 1981 (= Rheuma-Forum. Volume 11), ISBN 3-7650-1632-2 .
Web links
- G. Bergmann: Diet in hyperuricemia and gout . - Bavarian State Ministry of Justice and Consumer Protection
- Wolfgang Groebner, Ingeborg Walter-Sack: Hyperuricemia and Gout - Diagnostic. In: DMW - German Medical Weekly. 127, p. 207, doi : 10.1055 / s-2002-19897 .